ISSN Online: 2177-1235 | ISSN Print: 1983-5175
Treatment of Mammary Ptosis with Crossed Flaps without Skin Preresection
Tratamento das Ptoses Mamárias com Retalhos Cruzados sem Prévia Ressecção de Pele
Articles -
Year2000 -
Volume15 -
Issue
1
Arnaldo Lobo Miró
ABSTRACT
The author has been using this technique for more than 10 years in mammary ptosis cases - 90% of the cases in pure ptosis and 10% in ptosis with small hypertrophy cases. Once it is a technique that is easy to perform, it does not require the skin preresection in the initial phase nor the rigid demarcation upon surgery start, which shall be performed only when flaps are already positioned and skin may be fitted according to mamma shape. Previous marking serves just as reference. This is a safe procedure that preserves circulation, skin, fat and glandular component. It allows extensive rotation of mamma base with minimal bleeding and greatly favors tissue visualization. Scares are deployed on medial and lateral segment and areola and nipple rise are easily made.
Keywords:
Mammoplasty; crossed flaps; no skin preresection
RESUMO
O autor tem usado este tipo de técnica há mais de 10 anos, em casos de ptose mamária - 90% dos casos em ptose pura e 10% em casos de ptose com pequenas hipertrofias. Sendo uma técnica de fácil execução, ela nos permite não fazer a ressecção da pele na fase inicial e nem nos ater a uma demarcação rígida no início da cirurgia, fazendo-a somente quando os retalhos já se encontram posicionados, e a pele então pode ser acomodada de acordo com o formato da mama. A marcação prévia serve somente como referência.
É um procedimento seguro, que preserva a circulação, a pele, a gordura e o componente glandular. Permite uma rotação ampla da base da mama, com mínimo sangramento, e favorece enormemente a visualização dos tecidos.
As cicatrizes são distribuídas em segmento medial e lateral, e a ascensão da aréola e do mamilo se faz com facilidade.
Palavras-chave:
Mamoplastia; retalhos cruzados; sem ressecção prévia de pele
INTRODUCTION
Mammary ptosis treatment has been studied by surgeons since Pouson's work(1), in 1897. From then on, and up to 1957, a number of technigues and approaches were developed achieving better or worse results, but with high rates of complications. In 1957, Ariê(2) published a paper exposing the single vertical incision technigue. This work was the starting point for several studies, variations and enhancements for the pathology correction. The crossed-flap technique was enhanced based on Beisenberger's(3), Dufourmentel's(4), and Gillies(5) and Marino's surgeries, being divulged here and adopted by Brazilian authors such as Sperli(6), Pigossi(7), Hamke(8), etc.
Considering that mammary ptosis presents a great disparity between content (glandular fatty tissue) and container (skin), this latter being always excessive, we chose mammary flap intercrossing technique once it presents a number of favorable points in relation to other procedures.
We have used this technique in more than 100 patients for an 8-year period, the majority of cases being pure ptosis (90%) and the remaining (10%) being ptosis associated to small hypertrophies. More appropriate techniques are chosen for medium and large hypertrophies.
As it is easy to be performed and gives highly satisfactory results, in some cases it does not require previous skin resection, once cutaneous flaps will be fitted according to mammary cone build-up and not according to preestablished design. In these cases, marking serves just as a reference point. Thus, this procedure brought a considerable decrease on risk margin with relation to preoperative marking, mainly in those cases in which skin presents extreme resilience.
Along with these advantages, cutaneous, fatty and glandular circulatory component preservation are also granted, facilitating an effective rotation of mamma external pole and decreasing its base. Given glandular fatty flap superposition, it allows a marked projection forming a stable and good-consistence cone. In addition to presenting minimal bleeding, gland detachment in retromammary avascular area favors good tissue visualization and gives access to a possible existing pathology.
In most of the cases the resulting scars were small and the raise of the areola-nipple complex was performed with no tension level and with sensitivity integrally preserved.
SURGICAL TECHNIQUE
It follows mammary surgery general principies performed with the patient semiseated, general anesthesia, assisted local anesthesia or high peridural anesthesia, according to each patient.
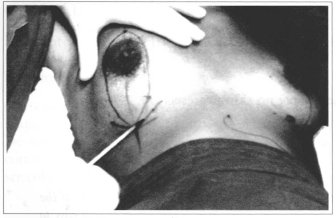
Point A is marked at humeral midline, always 1 to 2 cm above areola-nipple complex, points B and C are determined by clamping with the fingers the excessive skin to be hypothetically removed, and terminating 1 cm above mammary fold (Fig. 1).
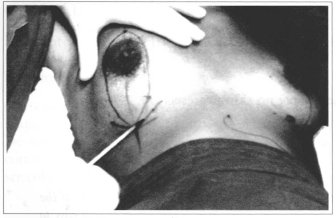
Fig. 1 - Marking of the reference point.
Then, stitches are joined in spindle-shape and lateral compensations that will form an inverted T when surgery is completed are marked.
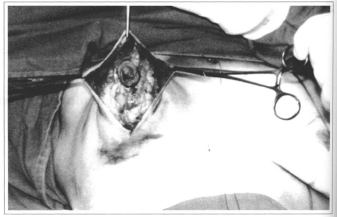
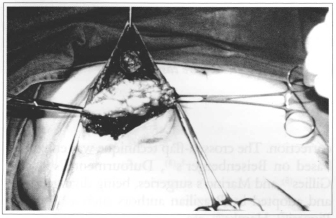
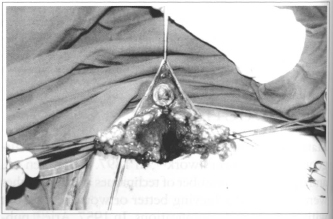
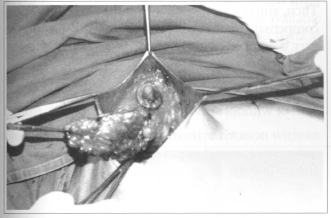
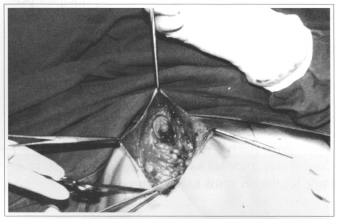
After areola-nipple complex demarcation, Schwartzman maneuver is performed around areola, with or without skin resection throughout the marked area. If doubt exists as to marking, surgery proceeds with a single median incision only (Fig. 2). Then, the whole retromammary gland space is detached from submammary fold using maximum of tissue available (Fig. 3). Detached gland is divided into two parts at it slower pole, forming two pediculate flaps: one medialand another lateral (Fig. 4). Afterwards, 3 to 4 em of skin will be released, trying to preserve vascular supply.
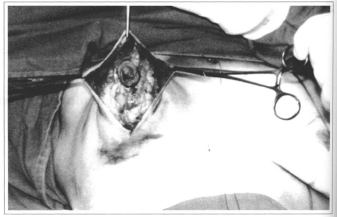
Fig. 2 - Anterior debridement with single medial incision.
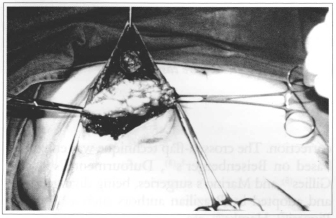
Fig. 3 - Gland debridement in the retromammary space.
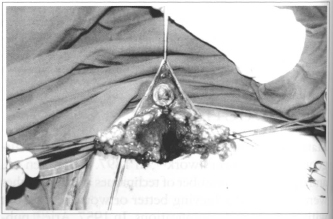
Fig. 4 - Mammary gland bipartition forming two pedicles (left and right).
Once released, they allow extensive rotation without difficulty. Formed flaps are rotated, one over another, towards retromammary space and their extremities fixed to muscular aponeurosis (Figs. 5 & 6).
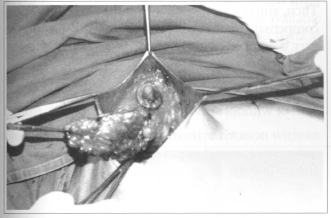
Fig. 5 - Rotation of the medial pedicle.
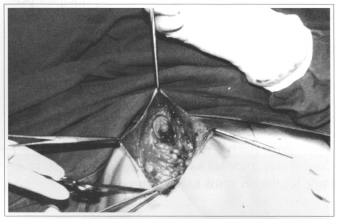
Fig. 6 - Rotation of the lateral pedicle.
Flaps will be also fixed among each other by sutures on their edges. If a small volume reduction is required, the tissue from the flap edge will be resected, forming the mammary cone. Lower edges will also be fixed to thoracic wall by means of sutures.
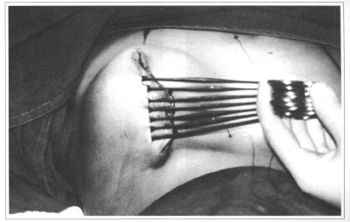
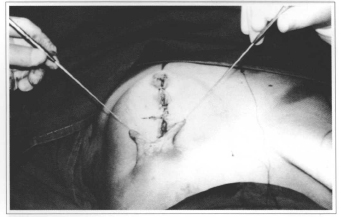
Then, skin accommodation is performed with the aid of Allis forceps or by digital maneuver, resecting as required. At this point, for the surgeon's safety, we recommend that cutaneous flaps are resected in segments (Fig. 7).
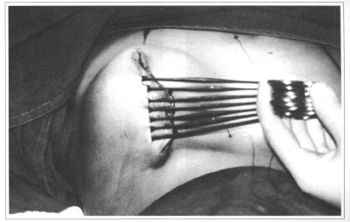
Fig. 7 - Skin accommodation wih Hallis forceps.
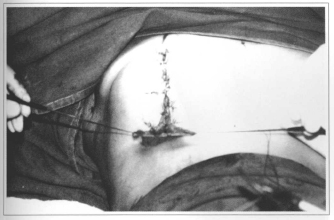
If previous resection is chosen, compensation triangles may be resected at the beginning of the surgery and readapted when required. If posterior skin resection is chosen, triangles will be prepared after median segment closure, being their length always of enough size for the mammary fold accommodation (Figs. 8 & 9).
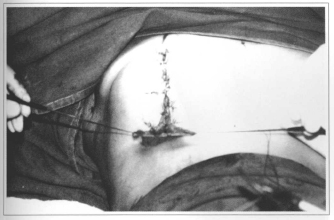
Fig. 8 - Remaining triangle.
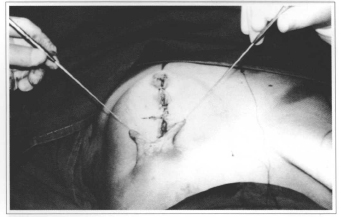
Fig. 9 - Remaining triangle.
Closure is made by Monocryl intradermic sutures covered with Micropore strips. The use of an elastic brassiere should be recommended for a minimum of 2 months.
COMPLICATIONS
Five per cent of the patients had a small lipolysis of lateral flap extremity that did not compromise, however, the final result nor mamma shape.
Three per cent of the cases presented discreet mammary asymmetry, which was reoperated. In addition to that, 3% of the cases presented mammary-areola complex diagonal elongation after accommodation (around 3 to 4 months) that deserved later repair.
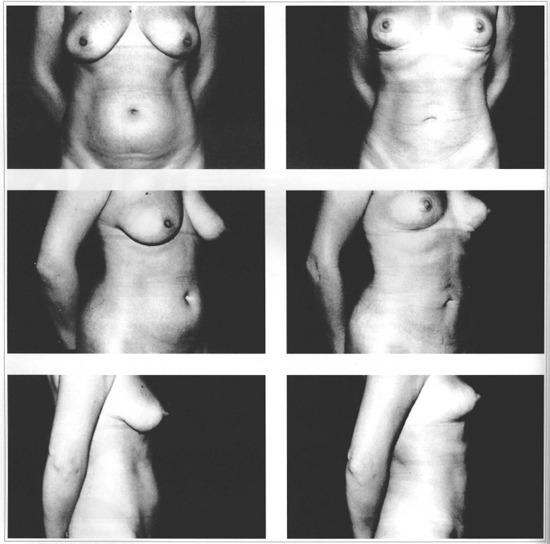
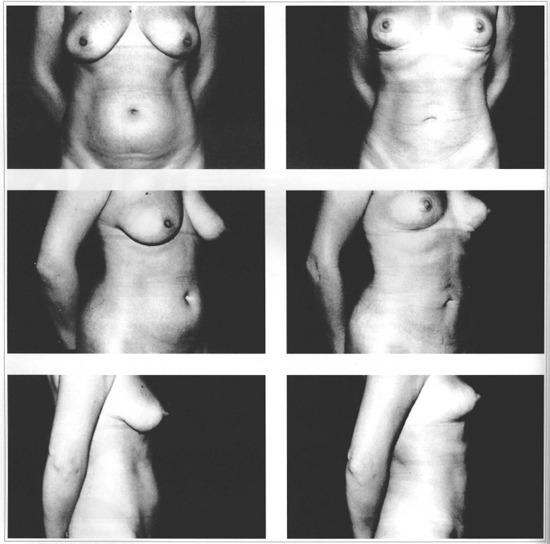
Fig. 10 - CASE 1: 42 years old patient presenting ptosis with moderate hypertrophy. Pre (left) and postoperative (right).
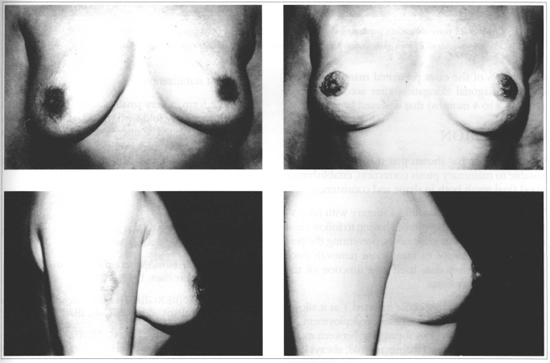
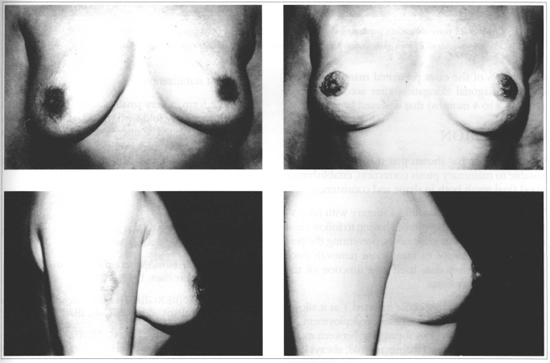
Fig. 11 - CASE 2: 32 years old patient presenting asymmetric ptosis. Pre (left) and postoperative (right).
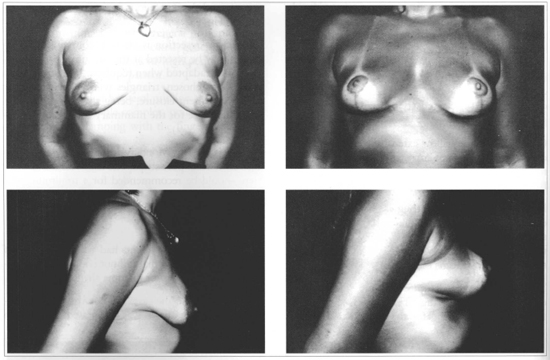
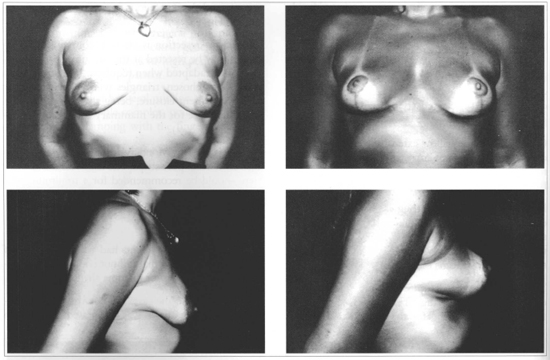
Fig. 12 - CASE 3: 23 years old patient presenting severe mammary ptosis. Pre (left) and postoperative (right).
CONCLUSION
Our experience has shown that this technique is favorable to mammary ptosis correction, establishing a good final result both in shape and consistency.
The possibility of performing a surgery with no previous skin resection and without having to follow rigid markings provides us great safety, preventing the performance of excessive or insufficient removals once skin must accommodate itself as a function of the formed mammary cone.
With relation to scar, we chose inverted T as it allows a good lateral and medial segment redeployment, in addition to a small distance shortening between mammary-areola complex and mammary fold, always long in ptosis cases. We believe this shortening also favors final result stabilization.
As to late form, a very small bascule, ample enough to cover mammary fold with the patient standing up, could be observed. The intercrossing of flaps forms a supporting loop at the lower pole, leading us to believe that it will prevent a great mobilization of this segment.
REFERENCES
1. POUSON M, MICHEL L. Sur un cas de mastopéxie. J. Méd. Bordeaux. 1897;27:495.
2. ARIE G. Nova técnica em mamaplastia. Rev. Latin. Amer. Cir. Plast. 1957;3:28.
3. BIESENBERGER HO. Eine neue Method der Mamaplastik. Zentralbl Chir. 1928;55:2382.
4. DUFOURMENTEL C, MOULY R. Modification of "periwinkleshell operation" for small ptotic breast. Plast. Reconstr. Surg. 1968;41:523.
5. GILLIES H, MARINO H. L'operation en colimaçon ou rotation spirale dans les ptoses mammaires moderées. Ann. Chir. Plast. 1958;3:90.
6. SPERLI A. Mastoplastia pela técnica dos retalhos cruzados. Rev. Soc. Bras. Cir. Plast. 1994;42-44.
7. PIGOSSI N, ANDRADE A, CALANGE H. Mamaplastia estética e funcional - experiência de 25 anos. Arq. Catar. Med. 1994;23:19-22.
8. HAKME F, GOMES FILHO BS, MULLER PM, SJOSTEDT C. Técnica em "L" nas ptoses mamárias com confecção de retalhos cruzados. Rev. Bras. Cir. 1983;73:87-91.
I - Honorary Member of the Brazilian Society of Plastic Surgery, Member of ISAPS, Guest professor of Medical Residence in Plastic Surgery of Hospital Universitário Evangélico de Curitiba, Member of Medical Residence teaching body in Plastic Surgery at PUC-PR, Director of Clínica de Cirurgia Plástica Dr. Arnaldo Miró.
Address for correspondence:
Arnaldo Lobo Miró, MD
R. Dom Pedro II, 749
80420-060 - Curitiba - PR Brazil
Phone: (5541) 342-7099 - Fax: (5541) 243-2332
 All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license
All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license