ISSN Online: 2177-1235 | ISSN Print: 1983-5175
Palatoplasty training model
Modelo de treinamento em palatoplastia
Special Article -
Year2011 -
Volume26 -
Issue
4
Allysson Antonio Ribeiro Gomes1; Flavius Vinícius Cabral Soares2; Salustiano Gomes de Pinho Pessoa3
ABSTRACT
Cleft lip and palate is the most common facial defect and causes several aesthetic and functional problems. The use of training models is recommended for training new surgeons, especially for surgeries in the oral cavity where surgical access and instrument handling are difficult. This paper describes a replicable training model of cleft palate closure that helps new surgeons acquire the technical skills required to carry out safe palatoplasty surgeries. The training model is composed of 5 steps, including theoretical classes, monitoring of real surgery procedures, and the preparation of the training model. The training model proposed here allows the surgeon to become familiar with surgery in the small and deep oral cavity; to learn how to use magnifying glasses and/or microscopes; and to perform incisions, dissection, and suturing at a depth. The model can be made manually and inexpensively, and is easy to replicate. The proposed simulator provides realistic training in palatoplasty and can be used to teach surgical techniques.
Keywords:
Palate/surgery. Training. Simulation.
RESUMO
A fissura labiopalatina é o defeito facial mais facilmente encontrado e implica diversos problemas estéticos e funcionais. O uso de modelos de treinamento é uma opção recomendável no treinamento de jovens cirurgiões, principalmente em cirurgias da cavidade oral, em que o acesso cirúrgico e o manejo dos instrumentos são dificultados. O objetivo deste artigo é descrever um modelo reprodutível de treinamento em fechamento de fendas palatinas, desenvolvendo segurança e habilidade técnica nos jovens cirurgiões para realização da palatoplastia. O modelo de treinamento é constituído de cinco etapas, incluindo aulas teóricas, vivência do ato operatório e confecção do modelo de treinamento. O modelo de treinamento proposto neste artigo permite que o cirurgião se familiarize com o trabalho em cavidade pequena e profunda, aprenda a utilizar lentes de aumento e/ou microscópio, e treine incisões, dissecção e sutura em profundidade, podendo ser confeccionado manualmente e com baixo custo. O simulador proposto permite treinamento realístico em palatoplastia, podendo ser usado para o ensino da técnica cirúrgica, sendo facilmente reprodutível.
Palavras-chave:
Palato/cirurgia. Capacitação. Simulação.
INTRODUCTION
Cleft lip and palate is the most common facial defect; it is present in 1 in 500 to 2000 live births depending on the studied population and causes many aesthetic and functional problems1.
Since the 19th century when Von Graefe and Roux successfully carried out surgical treatment of the cleft soft palate, surgical procedures have constantly evolved to better meet the main goal of palatoplasties: better speech quality and restoration of craniofacial bone development as close to normal as possible2. However, palatoplasty is not an innocuous and complication-free procedure since it depends on many factors3. Surgeon expertise and proper care during the postoperative period are among the main factors. Therefore, the use of surgery simulators in labs or training models allows surgeons in training to improve their technical skills, and these skills can be evaluated before their first in vivo procedure4.
The oral cavity presents several very specific characteristics that make surgical access and instrument handling difficult5. A model simulating a cleft palate is reported to be a dynamic mode for training plastic surgery residents to develop the skills required to safely perform this type of procedure4.
This paper aims to describe a replicable training model of cleft palate closure using a simulator.
METHODS
The proposed training model is an easy procedure comprising of 5 steps, with 60 hours allocated to the first 4 steps (Chart 1). The fifth step - in vivo surgery - is not included in this training protocol.
The first step of the training is intended to aid the surgeon's understanding of the disease. It consists of classes conducted by assistants and is separated into 2 modules of 4 hours each:
Introduction: the child with cleft lip and palate in the context of complete care; embryology of the face and etiopathogenesis of cleft lip and palate. Velopharyngeal insufficiency and cleft palate: classification and treatment (surgical techniques).
The second step involves observing a surgical procedure for cleft palate correction and includes the following:
Preoperative period: family context, multidisciplinary preparation, and checking the patient's physiological condition with relevant laboratory evaluations;Intraoperative period: humanization of the operating room, anesthetic preparation, steps of the surgical procedure (patient positioning, antisepsis technique, preparation of the operative field, markings, anesthetic infiltration, hydrodissection, flaps construction, palate reconstruction, sutures and bandage), and awakening from anesthesia; Postoperative period: immediate and late periods as well as complications and postoperative follow-up.
The third step involves making of the training model that will be incorporated into the individual training protocol. The training model of palate surgery is made using the materials listed in Table 1, following the steps described below:
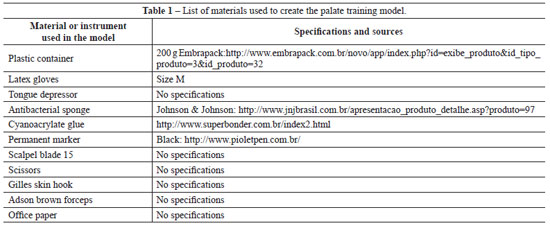
Separate all the material on a wide table (Figure 1A);
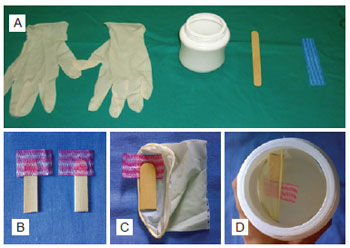
Figure 1 - In A, latex gloves, plastic container, wooden tongue depressor, and antibacterial fabric. In B, making the hard and soft palate muscles simulator. In C, assembly of the hard palate and muscles between the layers of the mucous membrane. In D, assembly of the glove-fabric-depressor set in the incision of the container.
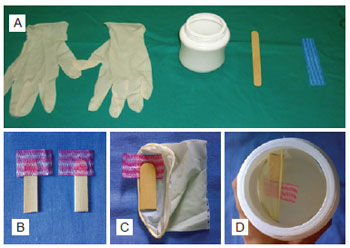
Copy the mold using office paper, observing the described dimensions (Figure 2);
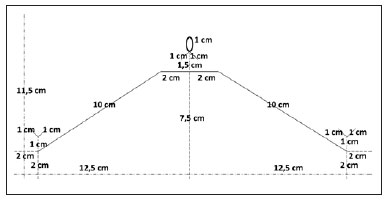
Figure 2 - Scheme for marking and cutting the plastic container.
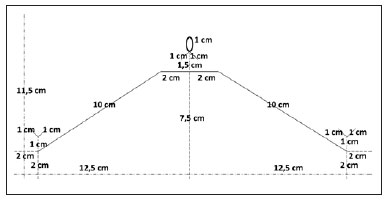
Cut along the continuous lines of the mold and glue the borders of its largest axis with adhesive tape, making an 11.5-cm-high cylinder; Position the mold around a plastic container and make markings with pen in places where it is to be cut; Take the paper mold from the plastic container and cut the marked places with a scalpel; scissors are allowed to complete cutting; Make markings on the procedure gloves, keeping a 6-cm margin from the wrists, and cut them; Mark and cut the tongue depressors, keeping a 4-cm margin from the ends; Mark and cut 2 rectangles (2 × 3.5 cm) of antibacterial fabric; Glue the antibacterial fabric rectangles in the tongue depressors with cyanoacrylate glue, maintaining their perpendicular axes and ensuring that two thirds of the fabric should be on one side of the tongue depressor and each depressor-fabric set should mirror the other (Figure 1B); Glue the depressor-fabric set at the border of the glove wrist with the fabric surface facing the glove, and repeat this procedure with the other glove (Figure 1C); Pass a glove-fabric-depressor set in each side of the plastic container with the help of an anatomic clamp and a Gilles skin hook; tie them at points a and b on each side of the container and keep the tongue depressors at the highest place of the container and at the innermost part of the glove (Figure 1D); Maintain the glove-fabric-depressor sets extended in the container, fixing the part of the glove that is out of the container with adhesive tape; Draw the palate on the gloves (Figure 3).

Figure 3 - Model ready for training.
The fourth stage of the training reinforces the knowledge and skills acquired in the previous stages through surgical technique training using the model. During this stage, the surgeon needs to get used to performing surgery on a small cavity with poor visualization, perform perception and depth sutures with and without magnifying glasses, manipulate extremely delicate tissues, and work with small angles providing limited access to the surgeon and assisting physician. This stage is divided into 2 sub-stages:
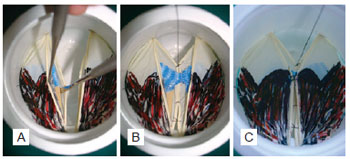
Simple sutures to be performed in a single stage; Simulation of all steps of the palatoplasty: marking, anesthetic infiltration, hydrodissection, incision, dissection, and suturing. At this stage, the surgeon will have the opportunity to make sutures with increasing levels of difficulty; the sutures are performed in 2 stages (i.e., the simulation of nasal and oral mucous membranes) with inverted stitches, in a U-shape with muscle sutures, which are part of the in vivo procedure (Figure 4).
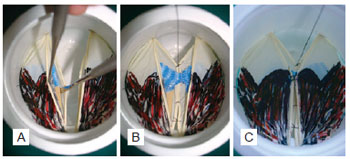
Figure 4 - Training. In A, simulation of dissection by stages. In B, first stage of suturing of the mucus membrane and muscles. In C, second stage of suturing (oral mucous membrane).
DISCUSSION
The traditional educational structure in surgery, which includes clinical sessions, conferences, and classic principles such as "watch once, make once, teach once" is not empirically supported and cannot be applied to the case of palatoplasty4. Several studies on adult learning have pointed toward the use of simulators that are safe; enable a cognitive, motor, and sensorial exercise that contribute to self-evaluation; and present a sequence of appropriate activities to yield the relevant acquisition of technical skills while not putting patients at risk4.
Cleft palate is a serious social, dental, and medical problem that stands out among surgical procedures performed by plastic surgeons due to its anatomical and technical complexity. To overcome this challenge, several authors propose models simulating palatoplasty6, including Furlow's technique5,7, oronasal fistula treatment and jaw bone graft8, nasal deformities in cleft lips9, and cleft lips10.
Cohen et al.8 and Fisher & Mann9 developed models for teaching cleft anatomy; the model created by the former demonstrates oronasal fistula and jaw bone graft using silicone molds obtained from the skeleton of the face of a person suffering from cleft palate. Owing to its high cost, it can only be assembled in a prosthesis laboratory and cannot be used for surgical training. The second model describes nasal deformities in cleft lip but does not allow suturing training.
The training model proposed herein allows surgeons to become familiar with working on small and deep cavities; learn how to use magnifying glasses and/or microscopes; and perform incisions, dissection, and deep suturing (Figure 4) in the same way as with the model presented by Vadodaria et al.6, in 2007. However, this model uses simple materials that can be easily acquired and does not require prefabricated or latex-molded structures unlike the previous model.
In 1999, Matthews7 described a home model for teaching Furlow's technique. Made with simple materials such as paperboard or polystyrene and latex, the model facilitates easy understanding of the procedure but does not include suturing training or enhance manual skills.
Recently in 2009, Nagy & Momaerts5 reported an advanced simulator of techniques for repairing cleft palates. They used materials that are cheap but difficult to handle in a prosthesis laboratory, requiring plastic and alginate molds. This model has disadvantages in that it does not allow the simulation of the entire surgical procedure and it only allows for training of Furlow's technique; further, the creation of the model takes a few days.
The training model proposed in the present study simulates the dimensions of the oral cavity of a child that will be operated on, helps enhance surgeons' manual skills, and does not require the use of any alginate or silicone molds. It is a low-cost simulator that produces satisfactory training results unlike the computer cleft lip simulator proposed by Schendel et al.10. The model and the proposed protocol presented here are inexpensive, the need for which has been highlighted by several authors11.
Completion of the basic training does not mean that a surgeon is capable of handling complex procedures in a clinical context. This initial training cannot be considered sufficient for the proper execution of the technique; it is still necessary to successfully complete all stages of the protocol by performing in vivo surgeries supervised by a more experienced surgeon.
CONCLUSIONS
The proposed simulator provides a realistic training simulation of palatoplasty and can be used for developing surgical techniques that involve the use of many types of sutures.
The present training model and proposed protocol are advantageous compared to others because they permit the learning process to go beyond the restrictions of laboratories.
The model can easily be made at a low cost by surgeons in training.
REFERENCES
1. Martins DMFS. Fissuras labiopalatinas. In: Schor N, ed. Guia de Cirurgia Plástica. São Paulo: Manole; 2007. p. 391-406.
2. De La Pedraja J, Erbella J, McDonald WS, Thaller S. Approaches to cleft lip and palate repair. J Craniofac Surg. 2000;11(6):562-71.
3. Baptista EVP, Salgado IV, Pereira R. Incidência de fístula oronasal após palatoplastias. Rev Soc Bras Cir Plast. 2005;20(1):26-9.
4. Dunkin B, Adrales GL, Apelgren K, Mellinger JD. Surgical simulation: a current review. Surg Endosc. 2007;21:357-66.
5. Nagy K, Mommaerts MY. Advanced s(t)imulator for cleft palate repair techniques. Cleft Palate Craniofac J. 2009;46(1):1-5.
6. Vadodaria S. The first cleft palate simulator. Plast Reconstr Surg. 2007;120(1):259-61.
7. Matthews MS. A teaching device for Furlow palatoplasty. Cleft Palate Craniofac J. 1999;36(1):64-6.
8. Cohen M, Polley JW, Figueros A, Habakuk SW, Iwamoto C. Teaching model for closure of oronasal fistula and bone grafting of the maxilla. Cleft Palate Craniofac J. 1996;33(3):198-01.
9. Fisher DM, Mann RJ. A model for the cleft lip nasal deformity. Plast Reconstr Surg. 1998;101(6):1448-56.
10. Schendel S, Montgomery K, Sorokin A, Lionetti G. A surgical simulator for planning and performing repair of cleft lips. J Craniomaxillofac Surg. 2005;33(4):223-8.
11. Dias IS, Pessoa SGP, Benevides AN, Macêdo JE. Treinamento inicial em microcirurgia. Rev Bras Cir Plast. 2010;25(4):595-9.
1. Plastic surgery resident practitioner of the Plastic Surgery Services at Universidade Federal do Ceará, Fortaleza, CE, Brazil.
2. Medical Academic Member of Universidade Federal do Ceará, Fortaleza, CE, Brazil.
3. Full member of the Brazilian Society of Plastic Surgery, in charge of the Plastic Surgery Service at Universidade Federal do Ceará, Fortaleza, CE, Brazil.
Correspondence to:
Allysson Antonio Ribeiro Gomes
Rua Coronel Américo Porto, 303, ap. 701 - Lauritzen
Campina Grande, PB, Brazil - CEP 58401-381
E-mail: aaribgomes@hotmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Paper received: August 8, 2011
Paper accepted: October 20, 2011
Study performed at Universidade Federal do Ceará, Fortaleza, CE, Brazil.
 All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license
All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license