ISSN Online: 2177-1235 | ISSN Print: 1983-5175
Gluteal flap as an alternative for the treatment of pressure ulcers in the ischial and sacral regions
Opções de retalhos da região glútea no tratamento da úlcera de pressão nas regiões isquiática e sacral
Original Article -
Year2013 -
Volume28 -
Issue
3
Fabiano Calixto Fortes de Arruda
ABSTRACT
BACKGROUND: Pressure ulcers are due to vascular insufficiency in tissues located mainly near bony prominences. More advanced wounds require microsurgical treatment using different types of flaps originating from the same or more distant areas. This study reports the use gluteal flaps for the treatment of pressure ulcers in the ischial and sacral regions.
METHODS: A total of 29 patients with National Pressure Sore Advisory Panel Consensus - 1989 stage III or IV pressure ulcers were followed in a tertiary hospital in metropolitan Goiânia between May 2010 and April 2012.
RESULTS: Among the 29 patients subjected to surgery, 10 (34.5%) were female and 19 (65.5%) were male, aged between 17 and 67 years (mean: 37.82 years). They had paraplegia resulting mainly (79%) from motorcycle accidents. Stage III (27.5%) and IV (72.5%) ulcers were treated with fasciocutaneous flaps (38%) or myocutaneous flaps (62%).
CONCLUSIONS: The use gluteal flaps for the treatment of pressure ulcers in the ischial and sacral regions is an excellent option that can aid patient recovery and rehabilitation.
Keywords:
Pressure ulcer. Surgical flaps. Reconstructive surgical procedures. Gluteal region flaps.
RESUMO
INTRODUÇÃO: A úlcera de pressão é o resultado de insuficiência vascular em tecidos localizados preferencialmente em áreas de proeminência óssea. O tratamento cirúrgico dessa lesão abrange fases mais avançadas dessa ferida, podendo ser realizados vários retalhos de origem local ou mesmo distante, por meio do uso da microcirurgia. Este estudo relata a experiência com o uso de retalhos da região glútea no tratamento da úlcera de pressão nas regiões sacral e isquiática.
MÉTODO: Foram estudados 29 pacientes portadores de úlcera de pressão com estágios III e IV (National Pressure Sore Advisory Panel Consensus - 1989), acompanhados em hospital terciário da região metropolitana de Goiânia no período de maio de 2010 a abril de 2012.
RESULTADOS: Dos 29 pacientes submetidos a cirurgia, 10 (34,5%) eram do sexo feminino e 19 (65,5%), do masculino, com idade variando de 17 anos a 67 anos (média, 37,82 anos), com paraplegia decorrente, em grande parte (79%), de acidente motociclístico. As úlceras eram de estágios III (27,5%) e IV (72,5%), e foram tratadas com retalhos fasciocutâneos (38%) ou miocutâneos (62%).
CONCLUSÕES: O uso de retalhos da região glútea no tratamento da úlcera de pressão nas regiões isquiática e sacral é uma ótima opção, podendo beneficiar o paciente em sua recuperação e reabilitação.
Palavras-chave:
Úlcera por pressão. Retalhos cirúrgicos. Procedimentos cirúrgicos reconstrutivos. Retalhos da região glútea.
INTRODUCTION
Pressure ulcers occur as a result of ischemic vascular insufficiency caused by pressure exceeding normal arterial pressure1 (32 mmHg) and involve tissues such as skin, subcutaneous tissues, and muscle. They are commonly located at bony prominences. There are reports of mummies circa 3000 BCE with pressure ulcers. However, this condition only became common after the First World War because of the large number of war casualties with spinal lesions and acute injuries in areas under the pressure of bony prominences2.3. After the Second World War, there was a marked change in the survival of these patients because of an improved understanding of the underlying mechanisms, use of antibiotic therapy, and the aid anesthesia; these factors collectively improved the therapeutic approach and reduced mortality from 61% to 3.8%2,3.
In Brazil, statistical data on the hospitalization cost of a patient with this comorbidity are unavailable. However, according to data from the Agency for Health Care Policy and Research, the total cost of pressure ulcer care in the United States in 2010 was US$15 billion; thus, the approximate cost per hospitalized patient with osteomyelitis caused by ulcers is US$59,0004.
The surgical treatment of ulcers was initially limited to the use of cutaneous and fasciocutaneous flaps. However, the use of muscle flaps to cover the area improved the quality of bone vascularization in patients with osteomyelitis, increasing the use of muscles as an indication for the treatment of these ulcers. The development of microsurgery and anatomical techniques has led to a new option involving the use of perforator flaps.
Pressure wounds may occur in several areas of the body, but the most affected areas are the ischial, sacral, and trochanteric regions5. The use of flaps from the gluteal region for covering affected areas offers satisfactory results with good structural appearance, favoring patient recovery and rehabilitation.
METHODS
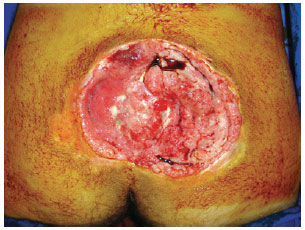
Pressure ulcers were graded according to the National Pressure Sore Advisory Panel Consensus - 1989. This study included a total of 29 patients with stage III pressure ulcers (lesion involving subcutaneous tissue and/or muscle with or without infection) or IV pressure ulcers (lesion involving bones or joints with or without infection) (Figures 1 and 2). The patients were followed at Rehabilitation Center Dr. Henrique Santillo, which is a tertiary hospital in metropolitan Goiânia, between May 2010 and April 2012. No patients presented with clinical intercurrences or alterations preventing or disqualifying them from surgical treatment. All patients were previously examined and assessed for the presence of anemia, alterations in kidney function, nutritional status, cardiac status, and surgical risk. Photographs of all treated patients were taken. All patients signed the consent form prior to participating.

Figure 1 - Stage III sacral ulcer.

Figure 2 - Stage IV sacral ulcer.
The surgical approach used in this study refers only to the use of fasciocutaneous and myocutaneous flaps originating from the gluteal region. Ulcers treated with these flaps were from the sacral and ischial regions. Even though it is possible to use gluteal flaps to treat ulcers in the trochanteric region, we primarily opted for the ipsilateral tensor fascia lata flap.
RESULTS
Among the 29 patients subjected to surgery, 10 (34.5%) were female and 19 (65.5%) were male; they were between 17 and 67 years old (mean: 37.82 years). Motor vehicle collision was the main cause of spinal cord injury, including 23 by motorcycle (79%) and 6 by car (21%), while in 1 patient (3.5%), it was caused by cerebrovascular disease. All patients were at least paraplegic, and their lesions occurred in other hospitals.
A total of 29 reconstructions were performed with flaps from the gluteal region, including 21 (72.5%) and 8 (27.5%) in the sacral and ischial regions, respectively. Regarding the therapeutic approach, 11 (38%) and 18 (62%) were fasciocutaneous and myocutaneous, respectively. All patients who underwent the fasciocutaneous approach had from flaps the sacral region. In the ischial region, all flaps were myocutaneous. Regarding stage, 8 (27.5%) and 21 (72.5%) patients had stage III and IV ulcers, respectively.
Only 1 patient (3.5%) had previously received treatment in the sacral region from another service; however, this patient was treated with a contralateral flap. Comorbidities were observed in 2 (7%) patients with managed diabetes mellitus; they consented to treatment and achieved good results.
There were only 4 (14%) cases of partial flap dehiscence, which were healed by secondary intention without requiring a new approach. There was only 1 case (3.5%) of wound infection during postoperative care. There were no cases of necrosis, seroma, or hematoma. As of writing, there have been no cases of recurrence.
Patients were hospitalized between 3 and 10 days, with a mean of 5.1 days. They were followed for 6 to 24 months. After 3 months of healing, the patients were referred to physiotherapy for rehabilitation.
DISCUSSION
The number of patients with pressure ulcers has increased in recent years; this is mainly due to the high number of motor vehicle collisions with rachimedullar injuries combined with insufficient care during the evolution of these patients while hospitalized in intensive care units or wards; this includes long periods without position changes, inadequate nutrition, lack of hygienic processes, and lack of physiotherapy support and qualified professionals5-11.
The treatment of pressure ulcers in their initial stages (i.e., stage I and II)6 and prevention are the best methods for limiting progression and avoiding surgery. Thus, a lack of preventive measures combined with inadequate patient care incurs significant public or private healthcare costs.
Patients who presented with adequate clinical conditions were initially selected. Patients who presented with comorbidities such as diabetes mellitus were first controlled before undergoing surgery. All patients in the present study had albumin > 3.5 g/dL, no absence anemia (i.e., Hb > 11 g/dL), and no clinical infection. Furthermore, the patients did not require colostomy for local reconstruction.
Ulcers treated with flaps from the gluteal region were mainly located in the sacral and ischial areas. Ulcers in the trochanteric region were primarily treated by using the ipsilateral tensor fascia lata flap.
In this study, the sacral region was reconstructed in 21 patients using V-H or O-H advancement fasciocutaneous flaps, V-Y advancement myocutaneous flaps, or rotation myocutaneous flaps (Figures 3-12). Flaps from the gluteal region, as described herein, are the primary choice for use in the sacral region. However, there are other options for treating this area, including lumbosacral, perforator, and microsurgical flaps.

Figure 3 - Debrided sacral ulcer and intraoperative marking.

Figure 4 - V-Y bilateral advancement fasciocutaneous flap.

Figure 5 - Debrided sacral ulcer with a V-Y flap on the right side and a V-Y flap with inferior pedicle on the left side.

Figure 6 - Postoperative aspect after bilateral V-Y flap.

Figure 7 - Debrided sacral ulcer.

Figure 8 - O-H unilateral fasciocutaneous flap.

Figure 9 - Sacral ulcer.

Figure 10 - Local advancement flap.
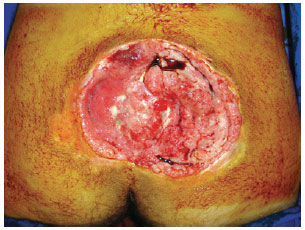
Figure 11 -Stage IV sacral ulcer.

Figure 12 - V-Y advancement myocutaneous flap.
The use of flaps from the gluteal region provides good results, because this area has good vascularization with 2 myocutaneous arteries (i.e., the superior and inferior gluteal arteries), making it suitable not only for local flaps, but also microsurgical flaps for breast reconstruction. The use of local flaps is usually the primary treatment choice. In the present case series, the use of fasciocutaneous flaps was a good option, because they are less sensitive to ischemia and more resistant to pressure; meanwhile, myocutaneous flaps are excellent for covering deep ulcers5,12-14.
The fasciocutaneous flap from the sacral region, which is known as a transverse lumbosacral flap, can be used in the sacral region15,16. The vascular pedicle of this flap is based on the lumbar artery perforators. However, this is not always the primary option. Therefore, the use of V-Y fasciocutaneous flaps5,17-20 is another option; this is an advancement flap that can be very useful for treating the sacral and even gluteal region as it can cover areas up to 10 cm long with diverse approaches such as the horizontal classic approach in the gluteal region with a vertical shape or a laterally positioned preserved pedicle. The O-H fasciocutaneous flap is another way of preparing the advancement flap and consists of a rectangular advancement covering the affected region. Perforator flaps5,21-25 of the gluteal region are similar to local flaps. However, they exhibit greater mobility as they are attached only through the perforators. Thus, they are also a useful alternative. Advancement myocutaneous flaps26-30 can be similar in shape to V-Y or O-H flaps, whereas rotational myocutaneous flaps allow adequate coverage and local vascularization. Microsurgical flaps are a secondary option and are mainly indicated in cases of recurrence in which local flaps cannot be reused.
Myocutaneous flaps were selected for treating the ischial region of patients because they allow better coverage and local vascularization, increasing the lifespan of local bones, which are often degenerated by local trauma owing to a lack of protection of muscle and adipose tissue. We used rotational and island myocutaneous flaps in the present case series5,31-34 (Figures 13-18). Flaps from other areas such as muscles of the posterior thigh, femoral, and semitendinosus biceps can also be used.

Figure 13 - Left ischial ulcer.

Figure 14 - Island myocutaneous flap.

Figure 15 - 12 months postoperatively.

Figure 16 - Stage IV right ischial ulcer.

Figure 17 - Advancement myocutaneous flap.

Figure 18 - Partial dehiscence at donor site.
The posterior thigh fasciocutaneous flap is usually selected for treating the ischial region5,7,35,36 because it enables good coverage of the area and can be advanced once more if new approaches are required. Although this study describes the use of flaps from the gluteal region for treating the ischial region, this is not necessarily our first option for treating ulcers in this region. The inferior gluteus maximus myocutaneous flap is used more frequently. However, island flaps can also be used with satisfactory results. Perforator, microsurgical, and local myocutaneous flaps can also be used but not as a primary approach.
There were no cases of recurrence during the study period. This can be explained by 3 factors: the sample was not large enough, follow-up was only 24 months, and strict inclusion criteria for surgery candidates were adopted. These factors may have eliminated issues that could lead to increased complications such as dehiscence. Nonetheless, the long-term recurrence rate would likely have been similar to that described in the literature (>16%)5,9, reflecting the difficulty of keeping these patients under long-term rehabilitation.
Patients under postoperative care receive physiotherapy and treatment with enoxaparin according to joint evaluation by a vascular surgeon. A first-generation cephalosporin is administered on the first day. All debrided material is sent for culture analysis. Antibiotic treatment is initiated if the patient develops clinical signs of infection according to analysis of the local flora. Drainage takes place 48 hours after drain removal is requested. After 3 months, if the site is healed without the presence of dehiscence, the patient is referred for physiotherapy and rehabilitation.
CONCLUSIONS
There are several options for closing pressure ulcers, and there is no consensus on the best flap for each ulcer type.
The approach should provide maximum coverage and improve local vascularization. Accordingly, the present results show that the use of flaps from the gluteal region is an excellent initial treatment option for the surgical treatment of pressure ulcers in the sacral or ischial regions, favoring patient recovery and rehabilitation.
REFERENCES
1. Kosiak M. Etiology of decubitus ulcers. Arch Phys Med Rehabil. 1961;42:19-29.
2. Bennet G. Historical chapter. In: Howorth MB, Petrie JG, eds. Injuries of the spine. Baltimore: Williams and Wilkins; 1964. p. 1-19.
3. Silver JR. History of the treatment of spinal injuries. Postgrad Med J. 2005;81(952):108-14.
4. AHRQ. National Healthcare Disparities Report, 2011. Chapter 2. Effectiveness of Care (continued, 4). Functional Status Preservation and Rehabilitation Importance. Disponível em: http:/www.ahrq.gov/qual/nhdr11/chap2d.htm. Acesso em: 1º/6/2012.
5. Bauer J, Phillips LG. Pressure sores. Plast Reconstr Surg. 2008;121(1 Suppl):1-10.
6. Ferreira LM, Calil JA. Etiopatogenia e tratamento das úlceras de pressão. Diagnóstico & Tratamento. 2001;6(3):36-40.
7. Levi B, Rees R. Diagnosis and management of pressure ulcers. Clin Plast Surg. 2007;34(4):735-48.
8. Souza Filho MVP, Cardoso DP, Girão RA. Tratamento cirúrgico das úlceras de pressão com retalhos cutâneos e musculocutâneos. Experiência de três anos no Hospital Geral Dr. Waldemar de Alcântara. Rev Bras Cir Plást. 2009;24(3):274-80.
9. Keys KA, Daniali LN, Warner KJ, Mathes DW. Multivariate predictors of failure after flap coverage of pressure ulcers. Plast Reconstr Surg. 2009;125(6):1725-34.
10. Fisher AR, Wells G, Harrison MB. Factors associated with pressure ulcers in adults in acute care hospitals. Adv Skin Wound Care. 2004;17(2):80-90.
11. Vidal J, Sarrias M. An analysis of the diverse factors concerned with the development of pressure sores in spinal cord injured patients. Paraplegia. 1991;29(4):261-7.
12. Mathes SJ, Nahai F. Reconstructive surgery: principles, anatomy and technique. New York: Churchill Livingstone; 1997.
13. Wong TC, Ip FK. Comparison of gluteal fasciocutaneous rotational flaps and myocutaneous flaps for the treatment of sacral sores. Int Orthop. 2006;30(1):64-7.
14. Rubayi S, Burnett CC. The efficacy of single-stage surgical management of multiples pressure sores in spinal cord-injured patients. Ann Plast Surg. 1999;42(5):533-9.
15. Hill HL, Brown RG, Jurkiewicz MJ. The transverse lumbosacral back flap. Plast Reconstr Surg. 1978;62(2):177-84.
16. Balakrishnan C, Brotherston TM. Transverse lumbar flap for sacral bed sores. Plast Reconstr Surg. 1992;89(5):998-9.
17. Borman H, Maral T. The gluteal fasciocutaneous rotation-advancement flap with V-Y closure in the management of sacral pressure sores. Plast Reconstr Surg. 2002;109(7):2325-9.
18. Pu LL. Reconstruction of a large gluteal soft-tissue defect with the double-opposing V-Y fasciocutaneous advancement flap. Plast Reconstr Surg. 2007;119(2):599-603.
19. Park C, Park BY. Fasciocutaneous V-Y advancement flap for repair of sacral defects. Ann Plast Surg. 1988;21(1):23-6.
20. Ay A, Aytekin O, Aytekin A. Interdigitating fasciocutaneous gluteal V-Y advancement flaps for reconstruction of sacral defects. Ann Plast Surg. 2003;50(6):636-8.
21. Prado A, Ocampo C, Danilla S, Valenzuela G, Reyes S, Guridi R. A new technique of "double-A" bilateral flaps based on perforators for the treatment of sacral defects. Plast Reconstr Surg. 2007;119(5):1481-90.
22. Coskunfirat OK, Ozgentas HE. Gluteal perforator flaps for coverage of pressure sores at various locations. Plast Reconstr Surg. 2004;113(7):2012-7.
23. Ahmadzadeh R, Bergeron L, Tang M, Morris SF. The superior and inferior gluteal artery perforator flaps. Plast Reconstr Surg. 2007;120(6):1551-6.
24. Scheufler O, Farhadi J, Kovach S, Kukies S, Pierer G, Levin LS, et al. Anatomical basis and clinical application of the infragluteal perforator flap. Plast Reconstr Surg. 2006;118(6):1389-400.
25. Verpaele AM, Blondeel PN, Van Landuyt K, Tonnard PL, Decordier B, Monstrey SJ, et al. The superior gluteal artery perforator flap: an additional tool in the treatment of sacral pressure sores. Br J Plast Surg. 1999;52(5):385-91.
26. Ohjimi H, Ogata K, Setsu Y, Hagara I. Modification of the gluteus maximus V-Y advancement flap for sacral ulcers: the gluteal fasciocutaneous flap method. Plast Reconstr Surg. 1996;98(7):1247-52.
27. Fisher J, Arnold PG, Waldorf J, Woods JE. The gluteus maximus musculocutaneous V-Y advancement flap for large sacral defects. Ann Plast Surg. 1983;11(6):517-22.
28. Ichioka S, Okabe K, Tsuji S, Ohura N, Nakatsuka T. Distal perforator-based fasciocutaneous V-Y flap for treatment of sacral pressure ulcers. Plast Reconstr Surg. 2004;114(4):906-9.
29. Rubayi S, Doyle BS. The gluteus maximus muscle-splitting myocutaneous flap for treatment of sacral and coccygeal pressure ulcers. Plast Reconstr Surg. 1995;96(6):1366-71.
30. Lee HB, Kim SW, Lew DH, Shin KS. Unilateral multilayered musculocutaneous V-Y advancement flap for the treatment of pressure sore. Plast Reconstr Surg. 1997;100(2):340-5.
31. Ramirez OM, Hurwitz DJ, Futrell JW. The expansive gluteus maximus flap. Plast Reconstr Surg. 1984;74(6):757-70.
32. Scheflan M, Nahai F, Bostwick J 3rd. Gluteus maximus island musculocutaneous flap for closure of sacral and ischial ulcers. Plast Reconstr Surg. 1981;68(4):533-8.
33. Stallings JO, Delgado JP, Converse JM. Turnover island flap of gluteus maximus muscle for the repair of sacral decubitus ulcer. Plast Reconstr Surg. 1974;54(1):52-4.
34. Stevenson TR, Pollock RA, Rohrich RJ, Vanderkolk CA. The gluteus maximus musculocutaneous island flap refinements in design and application. Plast Reconstr Surg. 1987;79(5):761-8.
35. Hurteau JE, Bostwick J, Nahai F, Hester R, Jurkiewicz MJ. V-Y advancement of harmstring musculocutaneous flap for coverage of ischial pressure sores. Plast Reconstr Surg. 1981;68(4):539-42.
36. Foster RD, Anthony JP, Mathes SJ, Hoffman WY. Ischial pressure sore coverage: a rationale for flap selection. Br J Plast Surg. 1997;50(5):374-9.
Specialist, plastic surgeon of the Rehabilitation and Reestablishment Center Dr. Henrique Santillo, full member of the Brazilian Society of Plastic Surgery, Goiânia, GO, Brazil
Correspondence to:
Fabiano Calixto Fortes de Arruda
Rua T-50, 540 - Setor Bueno
Goiânia, GO, Brazil - CEP 74215-200
E-mail: doutorfabianocalixto@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: July 26th, 2012
Article accepted: December 15th, 2013
Work performed at the Rehabilitation and Reestablishment Center Dr. Henrique Santillo, Goiânia, GO, Brazil.
 All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license
All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license