ISSN Online: 2177-1235 | ISSN Print: 1983-5175
Lip reconstruction after tumor resection
Reconstrução labial após ressecção de tumores
ABSTRACT
Introduction: Reconstruction of lip defects is popular owing to lip location and its anatomy. Thus, the objective of this work was to discuss the best options available for lip reconstruction.
Methods: This retrospective study included 50 patients who had undergone primary upper and lower lip reconstruction using local flaps, between January 2000 and January 2014. The defects were divided according to their location and size: defects affecting up to 1/3 of the lip and affecting more than 1/3 of the lip. The postoperative follow-up varied from 2 months to 3 years.
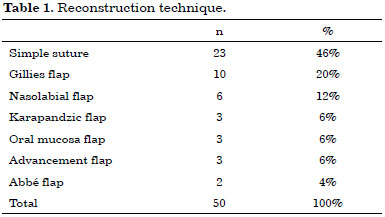
Results: Patient age ranged from 22 to 91 years. Most patients were in their seventies. Of the 50 reconstructions performed, 33 were in the lower lip (66%) and 17 in the upper lip (34%). For small defects affecting up to 1/3 of the lip, simple sutures were used (23 cases). The other 27 cases, in which more than 1/3 of the lip was affected, required interventions of different complexities.
Conclusion: When repairing defects up to 1/3 of the lower lip, the direct suture is the most suitable option. For defects affecting more than 1/3 of the lower lip, the Gillies and the Karapandzic flaps should be chosen instead, as they are reliable and allow the reestablishment of lip functionality. For defects affecting > 50% of the lip, and the Gillies and the Karapandzic flaps should not be considered, specifically to avoid microstomia.
Keywords:
Lip; Surgery; Reconstruction.
RESUMO
INTRODUÇÃO: O interesse antigo na reconstrução dos defeitos labiais pode ser explicado pela sua localização e pela singularidade da sua anatomia. Assim, o objetivo deste trabalho é discutir as melhores alternativas para a reconstrução labial.
MÉTODOS: Foi realizada uma análise retrospectiva de 50 casos submetidos à reconstrução primária dos lábios superior e inferior com o emprego de retalhos locais, no período de janeiro de 2000 a janeiro de 2014. Os defeitos foram divididos quanto à sua localização e quanto ao tamanho: defeitos que acometem até 1/3 do lábio e mais de 1/3 do lábio. O período de acompanhamento pósoperatório variou de 2 meses a 3 anos.
RESULTADOS: A idade dos pacientes variou entre 22 e 91 anos. A maior incidência foi na 7ª década de vida. Dentre as 50 reconstruções realizadas, 33 foram no lábio inferior (66%) e 17 no lábio superior (34%). Para defeitos pequenos, de até 1/3 do lábio, empregou-se a sutura simples (23 casos). Os demais 27 casos, cujos defeitos eram maiores que 1/3 do lábio, exigiram procedimentos com graus variáveis de complexidade.
CONCLUSÕES: Para a reparação dos defeitos de até 1/3 do lábio inferior, a sutura direta é a melhor opção. Para a reconstrução de defeitos maiores que 1/3 do lábio inferior, devemos optar pelos retalhos de Gillies e Karapandzic, pois são confiáveis e capazes de restaurar a função labial. No caso de defeitos maiores que 50% do lábio, devemos evitar as técnicas de Gillies e Karapandzic, a fim de evitar a microstomia.
Palavras-chave:
Lábio; Cirurgia; Reconstrução.
INTRODUCTION
Lip reconstruction has evoked interest since centuries. Lip reconstruction was mentioned for the first time in 1000 BC by Sushruta. Celsus, in 25 AD, performed a relaxing incision in the cheek to facilitate the surgical closure of a defect in the lower lip. However, it was Louis, in 1768, who was credited for the first wedge excision of a lip lesion using direct suture repair of the lesion margins. This atemporal interest can be because of the location of the lips, in the middle of the lower facial third segment and owing to the lip anatomy; scars and lip defects have a negative effect on the perception of honesty, the likelihood of a job offer, and reliability and overall abilities of an individual.
Since then, several techniques have been described for lip reconstruction with different complexities and with a variety of outcomes.
OBJECTIVES
The objective of this study was, thus, to discuss the best options available for lip reconstruction that would lead to the best functional and esthetic outcomes.
METHODS
A retrospective study was performed on patients who had undergone lip reconstruction after tumor resection; the study was conducted from January 2000 to January 2014, at the University Hospitals Clementino Fraga Filho, Antonio Pedro and Mario Kroeff, and at a private Clinic. The inclusion criteria were lip defects because of tumor resection, immediate reconstruction at the time of surgery, and reconstruction using local flaps. The exclusion criteria were late reconstruction and microsurgical free flaps. The defects were divided according to location (upper or lower lip) and size, that is, defects affecting up to 1/3 of the lip and more than 1/3 of the lip.
RESULTS
In total, 50 patients with lip reconstruction were included. The majority of the lip resections performed was owing to malignant and premalignant tumors, including basal cell carcinomas, squamous cell carcinomas, and actinic keratosis. Only one case was due to a hemangioma.
Patient age ranged between 22 and 91 years (average, 60.90 years). The incidence was higher in patients in their seventies (60 to 69 years, 12 patients); 50% of the patients were in their sixties or seventies.
Postoperative follow-up varied between 2 months and 3 years, with average of 10.7 months.
Of the 50 reconstructions performed, 33 were in the lower lip (66%) and 17 in the upper lip (34%).
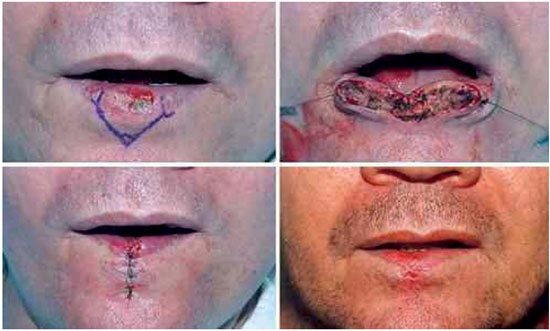
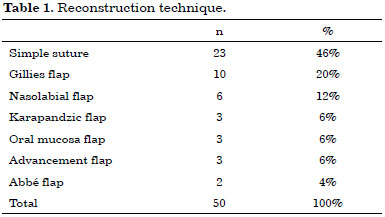
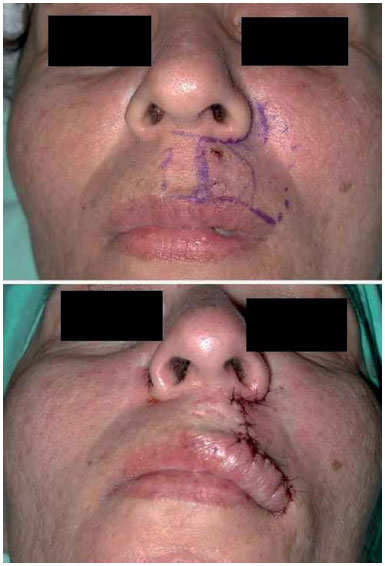
For small defects affecting up to 1/3 of the lip, the simple suture technique was used (Figure 1). For defects affecting more than 1/3 of the lip, interventions of different complexities were required (Table 1).
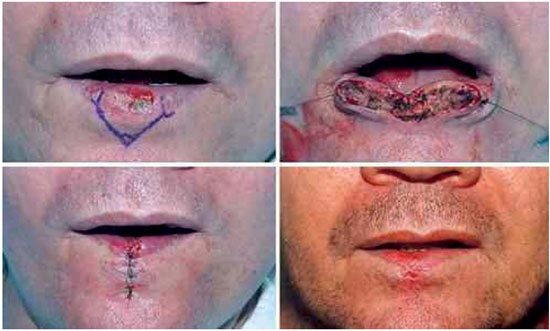
Figure 1. Resection and simple suture.
DISCUSSION
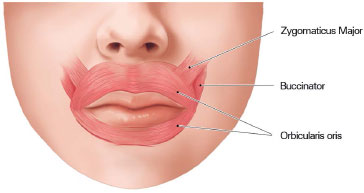
Multiple outcomes are aimed for when performing lip reconstruction. The first to consider is functionality. An esthetically pleasant reconstruction becomes inconsequential if oral competence is not restored1. This capacity depends of the orbicularis oris muscle, with most of its fibers horizontally oriented (Figure 2). It is also important to preserve the nerves, as lips with sensitivity are considered a better outcome than those in which sensitivity is not preserved1. The best results are achieved when the sphincter is reconstituted and sensitivity is maintained1.
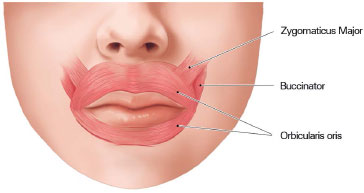
Figure 2. Orbicularis oris muscle. The main muscle behind lip function. Author of the illustration: Luciane dos Santos Mori.
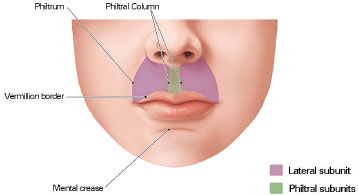
Therefore, to achieve functionality, the reconstructed lip should function as a sphincter, so that liquids are retained; lip opening should enable food consumption, hygiene, and use of dental prosthetics; and maintain sensitivity. To guarantee the most esthetically pleasant results, a few aspects should be taken into consideration when planning a lip reconstruction procedure (Figure 3):
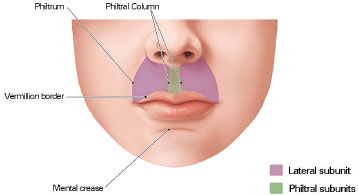
Figure 3. Borders and aesthetic subunits of the lips: important reference points in the reconstruction of the lips. Author: Luciane dos Santos Mori.
1. Local flaps should be used, including muscles with nerves, because those flaps offer the best resemblance, concerning color, texture, and thickness, with lip tissues2,3.
2. Topographic limits and esthetical units should be maintained, thus placing the sutures in these facial clefts or alternatively, following the lines connecting these facial subunits2-4.
3. Symmetry between the upper and lower lips should be preserved5.
4. The vermillion border should be perfectly aligned, and sutures in this area should be avoided.6,7
If these principles are not obeyed, the quality of the final results may be compromised, for example, with the appearance of visible scars, which may be immediately perceived even by casual observers1,4. In this study, the reconstruction technique carried according to lesion size and location, and the author's experience.
Flaps from distant tissues or micosurgical flaps should only be used when reconstruction with local flaps is not a viable option, or when complex reconstructions are with additional structures are required, such as the floor of the mouth, chin and mandible1,5,7-9.
Upper lip
In the upper lip, the use of primary suture should be restricted to small defects, but local flaps that can be realistically used are not abundant, as they often distort the philtrum and the "cupid's bow", nose, cutaneous-mucous line, and nasal cleft1,10.
For larger defects that cannot be repaired with primary sutures, advancement skin flaps, which are drawn in the same esthetic unit of the upper lip, are preferred10, as it involves minimal distortion of the perioral wrinkles, philtrum, and nose hair10. This flap moves forward in the direction of the defect through the excision of a portion of tissue around the wing of the nose, in the form of a "compensation perialar crescent" (Figure 4)1,8,11. Another method to move the flap forward, without distorting the skin-mucous transition line, is through an incision along the border of the redness area, creating a scar in the form of an inverted T, with the vertical axis of the scar aligned with the philtral column (Figure 5)5. In this study, there were no complications arising from the use of advancement skin flaps in three patients, who had excellent esthetic outcomes.
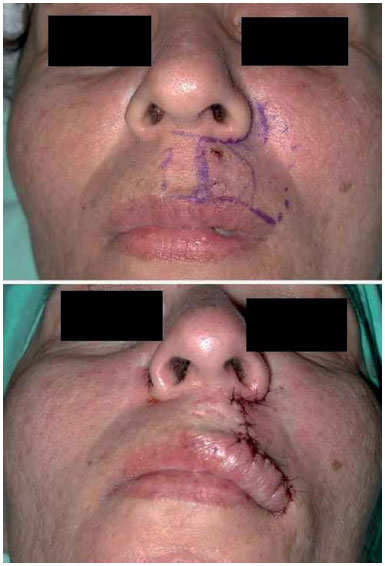
Figure 4. Skin flap, advanced after the removal of a skin perialar crescent for compensation. Attention is drawn to the final positioning of the scars.

Figure 5. Skin advancement flap: final positioning of the scars in the form of an inverted T, in the direction of the philtral column and the vermillion border.
The peri-labial transposition flaps can also be used in the reconstruction of defects that partially affect the thickness of the upper lip and have the advantage of recruiting more tissue than advancement flaps10. The most commonly used flaps is the nasal flap that can be obtained both using upper and lower pedicles. Flaps with upper pedicles are usually used to repair defects affecting the central portion of the upper lip10. Flaps with lower pedicles are commonly used to repair defects in the lateral portion of both the upper and lower lips2,10.
This flap is advantageous from an esthetic point of view: it can cause significant distortion in the relevant topographic limit established by the philtrum (Figure 6)2,10, can lead to clamping of the reconstructed lip2, and can lead to the development of permanent edema in its inferior border10. Of the 50 patients reported here, the nasal flap was used in 6 cases, with one case of local relapse of the lesion; in this case, the patient was later underwent a new surgical excision and closure with a primary suture. In two other patients, esthetic complications were observed: one patient had clamping of the upper lip, probably following contraction of the flap scar due to a narrow flap. The patient underwent cheiloplasty via the Millard technique, and had a good final result. In the second patient, permanent edema occurred in the lower border of the flap (Figure 7). To avoid cleft distortion, a V-Y advancement flap can be used as an alternative to the nasal flap, as described by Griffin et al.12. This flap is an excellent option when repairing skin defects larger than 1 cm and localized in the lateral portion of the upper lip that does not affect the wing of the nose or vermillion12.

Figure 6. Nasolabial flap with lower peduncle. Attention is drawn to the total loss of the left philtrum ridge.

Figure 7. Permanent edema of the lower end of the flap and loss of the philtrum.
The Abbé13 flap, first described by Pietro Sabattini in 1838, is created by transferring tissue from the lower to the upper lip (or vice-versa), while maintaining the flap pedicle in the lip artery (Figure 8). None of the two cases using Abbé flap had complications (Figure 9). However, there was a case of local relapse of the lesion. The flap can be single or double, quadrilateral, or even an island flap, and the flap should have approximately half the length of the defect to be repaired2. This flap is widely used to repair defects that are not thicker than half of the upper lip, both central and lateral defects, not involving the oral commissure1,7,10,14. This is advantageous because it allows the complete vertical portion, formed by the skin and redness area, to be repositioned7. The main disadvantage is that it remains pedunculated for 14 to 21 days1, which demands high collaboration from the patient. In this study, there were no complications with this flap; however, one case of local relapse of the tumor was observed owing to incomplete tumor excision.
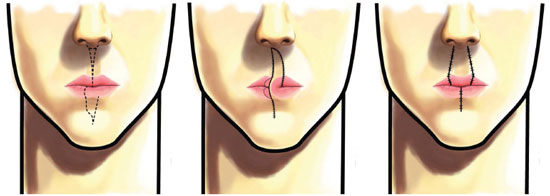
Figure 8. Abbé flap. Author of the illustration: Eduardo Furtado Souza.
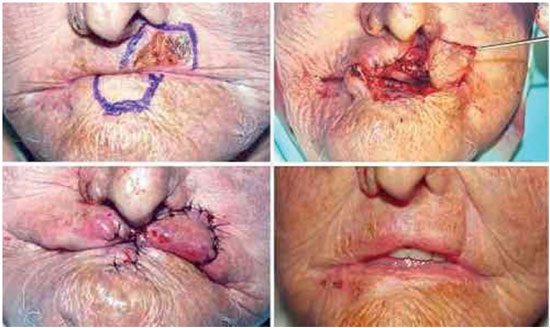
Figure 9. Abbé flap.
Lower lip
Defects affecting up to 1/3 of the lip
The V excision, followed by primary synthesis, should be the first option to repair defects affecting up to 30% of the lower lip1,2,7-11,15,16. Of the 23 cases of defects affecting up to 1/3 of the lip, reconstructed with primary sutures, V excisions were performed in all but one case, in which a W excision was performed (Figure 10). However, the V excision, associated with the lack of exams performed at the borders of the excision (following freezing of the excised tissues), may have caused a local relapse in three patients and in two patients in whom the margins were affected by the lesions. These patients underwent another surgery for the resection of the compromised margins.

Figure 10. W excision, to avoid extending the final scar beyond the mental crease.
In a series with 899 lip cancer patients, Papadopoulos et al.17 found a lower rate of relapse at 5 years in patients undergoing excision and direct suture compared with patients undergoing vermilionectomy or tumor excision, followed by reconstruction using flaps. These results were attributed to the insufficient removal of the resection margins, and additional studies were recommended to validate the results. In contrast, Casal et al.18 did not observe any statistical difference in mortality rates after local relapse associated with different types of reconstructions used. In cases when the V excision is too large and to avoid narrowing the margins of the resection, a relaxing incision should be performed along the mental crease or should be altered to a W excision10,19. Faulhaber et al.19 proposed that defects up to 15% of the lower lip are treated with a V excision and primary suture, whereas defects between 15% and 30% are treated with a W excision or with a zetaplasty.
For better esthetic results, the V excision should be planned so that its axis is oriented in the direction of the skin tension lines10. As such, in the region of the oral commissures, a more oblique V should be performed1. At last, to avoid depressed or retracted scars, lip reconstruction should be performed in four layers: in the mucosa, muscle, subcutaneous layer, and skin9,10.
For small cutaneous lesions in the lips, only one wedge excision followed by a simple suture is possible, with the axis in the same direction as the tension lines of the skin. M-plasty can be used to suture incisions so that the border of the vermillion is not transposed10.
Defects affecting more than 1/3 of the lip
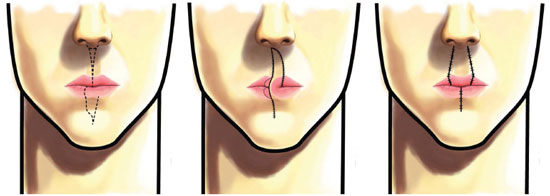
When more than 1/3 of the lip is lost, the local flaps are the best options for reconstruction1,2,5,7-11. The most commonly used techniques, which offer good results, are the use of rotation and advancement flaps in the oral commissure, such as the Gillies20 and Karapandzic21 flaps, as well as lip transfer flaps such as the Abbé13 and Estlander22 flaps.
The flap described by Gillies and Millard, in 195720, is compatible with the reconstruction of defects affecting 1/3 to 2/3 of the lip2, possibly up to 80% of the lip1, but the final esthetic results are less pleasant because these procedures can lead to lip shortening, loss of the oral commissures, or microstomia1. There were no complications in the 10 patients treated with the Gillies flap (Figure 11). However, local relapse occurred in one patient with xeroderma pigmentosum and with scattered facial lesions, who was lost to follow-up. The Gillies flap is created using three layers of the cheek region, unilaterally or bilaterally, allowing the tissue rotation around the oral commissure, similar to the Estlander flap, but including more tissue from the nasolabial region23. When planning the procedure, the new mouth angle should be drawn by defining the pedicle of the flap as having < 1.5 cm width and then rotating the angle 60º towards the defect23. A relaxing vertical incision is performed in the donor area, which leads to a certain degree of reinnervation of the flap within 12 to 18 months24.

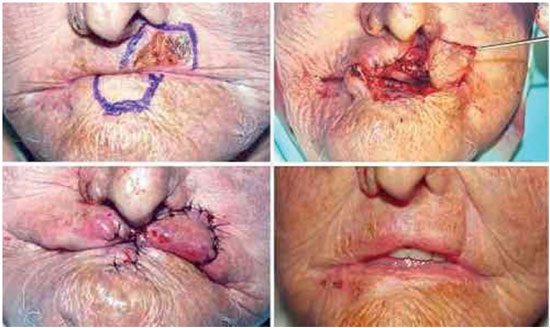
Figure 11. Gillies flap.
The Karapandzic21 flap, described in 1974, involves the use of two semilunar nasolabial flaps with upper pedicles to preserve the majority of the vascular structures and local nerves, allowing the transfer of the innervated muscles to the reconstruction site21,25. For smaller defects, the unilateral flap is enough, but for defects affecting more than 50% of the lip, bilateral flaps are necessary1. In these cases, however, the esthetic result is not as pleasant because the oral commissures will be softened and rounded. When outspread, this flap can restore up to 100% of the lip26. However, larger defects can increase the possibility of microstomia1,25,27. In this study, there was no post-surgical complication in the three patients who underwent reconstruction with the Karapandzic flap (Figure 12).

Figure 12. Karapandzic flap.
The Gillies and the Karapandzic procedures have two esthetic advantages: they preserve the oral commissure and the main scar is located along or above the medial cleft10, which is less obvious in the long term.
Although it should not be considered a complication, microstomia is a direct consequence, inevitable in some cases of large reconstruction using the Gillies and Karapandzic flaps.1,7. The anatomy of the oral commissures is preserved following flap rotation, but the commissures can still slightly advance in the medial direction. Of the three cases in which Karapandiz flaps were used, two experienced microstomia; of the ten patients who received Gillies flaps, four experienced microstomia (Figure 13). Of the 6 patients with microstomia, 4 underwent commissuroplasty (Figure 14), 1 was lost to follow-up (the patient with xeroderma pigmentosum mentioned above) and 1 did not receive further treatment, the reasons for which are unknown. However, not all cases of microstomia require commissuroplasty. When the patient can eat normally and if there is no saliva retention or speech impairment, microstomia will not be required21,28. There were no other recurrences or complications resulting from reconstructions performed using the Gillies and Karapandzic flaps.

Figure 13. Microstomia following reconstruction using a bilateral Gillies flap.

Figure 14. Commissuroplasty. Pre-surgery, immediate, and late post-surgery.
For defects affecting 50% or more of the lateral portion of the lower lip and to avoid microstomia, a cross transfer lip flap can be used, as described by Estlander22 in 1872 (Figure 15). This is a triangular flap with complete thickness, drawn in the lateral portion of the upper lip and rotated 180º around the commissure22.
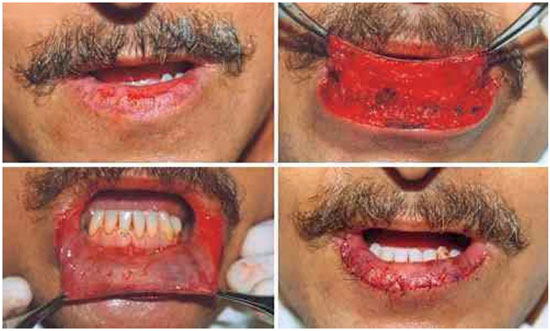
Figure 15. Oral mucosa advancement flap.
The "staircase technique" described by Johanson et al.29 in 1974, is an alternative to the Gillies20 and Karapandzic21 flap for reconstructions of defects affecting up to 2/3 of the lower lip29. This method uses two flaps of complete thickness that advance medially through a formation that resembles a "staircase".
In case of extensive lip loss (> 60%) and to avoid microstomia, McGregor23, Nakajima30 Webster-Bernard31 flaps, or a combination of different technical procedures can be used.
The method introduced by McGregor23, a modification of the Gillies20 procedure, can be used to reconstruct defects affecting up to 100% of the lower lip. This flap is mostly used for reconstructing lateral lip defects10, as it uses the commissure as a rotation point, thus preventing its distortion. Nevertheless, the use of this flap leads to changes in the direction of the perioral muscle fibers and loss of innervation of the reconstructed portion; in addition, reconstruction of the vermillion23 is required, which may use a flap from the tongue. The upper lip can also be repaired in this way.
The Nakajima30 method, which involves rotation over the oral commissure, preserves this structure, and also involves vermillion reconstruction. However, in contrast to the method proposed by McGregor, which uses complete thickness of the tissue, the Nakajima flap has partial thickness, directing the blood through the facial artery and not the labial artery. In this way, it is possible to extend the upper incision to a point near the vermillion border, making a larger flap with less left over tissue ("puppy ear")30.
The Webster-Bernard31 technique is based on the idea introduced by Bernard and Von Burrou and that modification, by Webster in 1960. This technique consists on the medial advancement of a cheek flap, preserving vascular structures and nerves, as well as the sphincter function of the lip. Despite excellent functional results, there are esthetical disadvantages associated, such as the formation of a cleft in the central lip incision, flattening of the reconstructed lip, and consequent protrusion of the upper lip, shortening of the cheeks, and reduction of the gum to lip cleft7,8,32.
The use of bilateral nasolabial gate flaps, as introduced by Fujimori3, is another option for reconstruction of defects that affect the totality of the lower lip. With this technique, flaps of up to 3 cm larger than the nasolabial flaps can be used without reaching the borders of oral commissures, which is inevitable with the Gillies20 and Karapandzic21 flaps and that leads to microstomia. In addition, the muscular and mucosal layers of the pedicle are not compromised, which allows the innervation of reconstructed area - innervated flaps are functionally advantageous - and are island flaps, that do not result in the formation of "puppy ears"3.
Another approach for the reconstruction of large lower lip defects is the combination of different techniques, such as the Webster with Karapandzic33, Webster with Abbé (Meyer-Abul-Failat)10, or Webster with "Staircase"34.
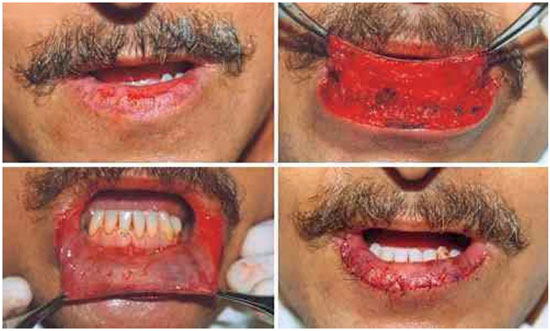
Vermillion
After resection, the lower lip vermillion can be reconstructed by directly suturing its borders or by preparation for an advancement flap of the oral mucosa1,2,10. In the 3 vermillion reconstruction cases in this study, an advancement flap was applied that was detached from the remaining oral mucosa up to the gum to the lip cleft, advancing anteriorly, and good results were achieved without complications1,2. The oral mucosa in the flap for vermillion reconstruction is the most natural procedure for this type of reconstitution10, as it highly resembles the lip vermillion and thus leads to almost invisible scars. Meanwhile, the exact reconstruction of the anterior line of the vermillion border can be difficult to achieve, which may cause some degree of asymmetry10. Sand et al.35 observed a more pleasing esthetical outcome and less vermillion reduction in patients who underwent reconstruction with mucosa advancement flaps compared with the group in which reconstruction was performed using a primary closure. As such, this author proclaims the use of primary closures in elderly patients and inpatients having comorbidities35.
Another excellent option for vermillion reconstruction of the lower lip is the use of tongue flaps, as their remarkable vasculature makes them highly reliable2,36, and as these can repair significant vermillion losses. The tongue flaps involves the ventral portion of the tongue36, as it mimics color and texture of the vermillion. The big disadvantage is that the procedure is performed in two separate stages, while the flap has to remain pedunculated for 14 days2.
Despite constant research on the best esthetic outcomes, the main focus of lip reconstruction involving restoration of functionality after localized disease control, should not be overlooked1,5,11. However, all plastic surgeons opt for techniques that correct repair and result in the smallest possible scars. In addition, most public hospitals do not provide have facilities for freezing the borders of resected tissues, which may explain local relapses and affected borders reported here. All cases with affected borders and local relapses underwent new excision and suture, without complications, except for one patient who had xeroderma pigmentosum and lived in a distant and impoverished area, and who was lost to follow-up.
CONCLUSIONS
For reconstruction of upper lip defects, advancement skin flaps can used, as they lead to good esthetic outcomes associated with minimal distortion of the lip anatomy. In the future, alternatives to the nasolabial flap should be implemented, as these flaps can cause important distortions of the nasolabial cleft and lead to poorer esthetic results.
For repair of defects affecting up to 1/3 of the lower lip, the direct suture is the best esthetic option, as long as the excision in V, if required, can be modified into a W excision to adjust the resection borders. For the reconstruction of defects affecting more than 1/3 of the lower lip, the Gillies and Karapandzic flaps should be the first choice, as these are reliable, can restore lip function, and associated scars are acceptable esthetically. For defects affecting more than 50% of the lip, Gillies and Karapandzic technical approaches should be chosen to avoid microstomia.
REFERENCES
1. Neligan PC. Strategies in lip reconstruction. Clin Plast Surg. 2009;36(3):477-85. DOI: http://dx.doi.org/10.1016/j.cps.2009.02.013
2. Anvar BA, Evans BC, Evans GR. Lip Reconstruction. Plast Reconstr Surg. 2007;120(4):57e-64e. DOI: http://dx.doi.org/10.1097/01.prs.0000278056.41753.ce
3. Fujimori R. "Gate flap" for the total reconstruction of the lower lip. Br J Plast Surg. 1980;33(3):340-5. PMID: 7426811
4. Burget CG, Menick FJ. Aesthetic restoration of one-half the upper lip. Plast Reconstr Surg. 1986;78(5):583-93. DOI: http://dx.doi.org/10.1097/00006534-198611000-00005
5. Sbalchiero JC, Anlicoara R, Cammarota MC, Leal PRA. Reconstrução labial: abordagem funcional e estética após ressecção tumoral. Rev Soc Bras Cir Plást. 2005;20(1):40-5.
6. Kogut J, Sbalchiero JC, Leal PRA. Reconstrução labial. In: Mélega JM, ed. Cirurgia Plástica: fundamentos e arte. Rio de Janeiro. Medsi; 2002. p.930-48.
7. Baumann D, Robb G. Lip reconstruction. Semin Plast Surg. 2008;22(4):269-80. DOI: http://dx.doi.org/10.1055/s-0028-1095886
8. Langstein H, Robb G. Lip and perioral reconstruction. Clin Plast Surg. 2005;32(3):431-45. DOI: http://dx.doi.org/10.1016/j.cps.2005.02.007
9. Siqueira EJ, Alvarez GS, Laitano FL, Martins PDE, Oliveira MP. Estratégias em reconstrução do lábio inferior. Rev Bras Cir Plást. 2012;27(4):536-41. DOI: http://dx.doi.org/10.1590/S1983-51752012000400011
10. Renner GJ. Reconstruction of the lip. In: Baker SR, ed. Local flaps in facial reconstruction. 2nd ed. St. Louis: Mosby; 2008. DOI: http://dx.doi.org/10.1055/s-2008-1080042
11. Pepper JP, Baker SR. Local flaps: cheek and lips reconstruction. JAMA Facial Plast Surg. 2013;15(5):374-82. DOI: http://dx.doi.org/10.1001/jamafacial.2013.1608
12. Griffin G, Weber S, Baker SR. Outcomes following V-Y advancement flap reconstruction of large upper lip defects. Arch Facial Plast Surg. 2012;14(3):193-7. DOI: http://dx.doi.org/10.1001/archfacial.2012.35
13. Abbe R. A new plastic operation for the relief of deformity due to double harelip. Plast Reconstr Surg. 1968;42(5):481-3.
14. Salgareli AC, Sartorelli F, Cangiano A, Collini M. Treatment of lower lip cancer: an experience of 48 cases. Int J Oral Maxillofac Surg. 2005;34(1):27-32. DOI: http://dx.doi.org/10.1016/j.ijom.2004.01.027
15. Dupin C, Metzinger S, Rizzuto R. Lip reconstruction after ablation for skin malignancies. Clin Plast Surg. 2004;31(1):69-85. DOI: http://dx.doi.org/10.1016/S0094-1298(03)00118-4
16. Dediol E, Luksić I, Virag M. Treatment of squamosu cell carcinoma of the lip. Coll Antropol. 2008;32 Suppl 2:199-202.
17. Papadopoulos O, Konofaos P, Tsantoulas Z, Chrisostomidis C, Frangoulis M, Karakitsos P. Lip defects due tumor excision: apropos of 899 cases. Oral Oncol. 2007;43(2):204-12. DOI: http://dx.doi.org/10.1016/j.oraloncology.2006.02.015
18. Casal D, Carmo L, Melancia T, Zagalo C, Cid O, Rosa-Santos J. Lip Cancer: a 5-year review in a tertiary referral centre. J Plast Reconstr Aesthet Surg. 2010;63(12):2040-5. DOI: http://dx.doi.org/10.1016/j.bjps.2009.12.022
19. Faulhaber J, Gérard C, Goerdt S, Koenen W. Functional and aesthetic reconstruction of full-thickness defects of the lower lip after tumor resection: analysis of 59 cases and discussion of a surgical approach. Dermatol Surg. 2010;36(6):859-67. DOI: http://dx.doi.org/10.1111/j.1524-4725.2010.01561.x
20. Siegert R, Weerda H. The history of lip reconstruction. Facial Plast Surg. 1990;7(2):63-71. DOI: http://dx.doi.org/10.1055/s-2008-1064666
21. Karapandzic M. Reconstruction of lip defects by local arterial flap. Br J Plast Surg. 1974;27(1):93-7. DOI: http://dx.doi.org/10.1016/0007-1226(74)90068-X
22. Estlander J. Eine Methode, aus der einen Lippe Substanzverluste der anderen zu ersetzen. Arch Klin Chir. 1872;14:622.
23. McGregor IA. Reconstruction of the lower lip. Br J Plast Surg.1983;36(1):40-7. DOI: http://dx.doi.org/10.1016/0007-1226(83)90008-5
24. Rea JL, Dawis WE, Rittenhouse LK. Reinnervation of an Abbe-Estlander and a Gillies fan flap of the lower lip: electromyographic comparison. Arch Otolaryngol. 1978;104(5):294-5. DOI: http://dx.doi.org/10.1001/archotol.1978.00790050060014
25. Azevedo DM, Nagassaki E, Carvalho AS, Lafayette KAS, Cação EG, Inforzato HCB, et al. Reconstrução do lábio inferior pela técnica de Karapandzic. Rev Bas Cir Plást. 2013;(28)1:168-71. DOI: http://dx.doi.org/10.1590/S1983-51752013000100028
26. Hanasono MM, Langstein HN. Extended Karapandzic flaps for near-total and total lower lip defects. Plast Reconstr Surg. 2011;127(3):1199-205. DOI: http://dx.doi.org/10.1097/PRS.0b013e318205f3ce
27. Brinca A, Andrade P, Vieira R, Figueiredo A. Retalho de Karapandzic e retalho de Bernard-Burrow-Webster na reconstrução do lábio inferior. An Bras Dermatol. 2011;86(4 Suppl 1):S156-9. DOI: http://dx.doi.org/10.1590/S0365-05962011000700041
28. Jabaley ME, Clement RL, Orcutt TW. Myocutaneus flaps in lip reconstruction. Applications of the Karapandzic principle. Plast Reconstr Surg. 1977;59(5):680-8.
29. Johanson B, Aspelund E, Breine U, Holmström H. Surgical treatment of non-traumatic lower lip lesions with special reference to the step technique. A follow-up on 149 patients. Scand J Plast Reconstr Surg.1974;8(3):232-40. DOI: http://dx.doi.org/10.3109/02844317409084399
30. Nakajima T, Yoshimura Y, Kami T. Reconstruction of the lower lip with a fan-shaped flap based on the facial artery. Br J Plast Surg. 1984;37(1):52-4. DOI: http://dx.doi.org/10.1016/0007-1226(84)90042-0
31. Webster RC, Coffey RJ, Kelleher RE. Total and partial reconstruction of the lower lip with innervated muscle-bearing flaps. Plast Reconstr Surg Transplant Bull. 1960;25:360-71. DOI: http://dx.doi.org/10.1097/00006534-196004000-00007
32. Huguier V, Berheuil N, Parry F, Robiolle C, Dagrégorio G. et al. Reconstruction post-traumatique de la lèvre inférieure après amputation totale ou subtotale selon la technique de Camile-Bernard modifiée Webster - avantages, inconvénients, limites: à propos de trois cas. Ann Chir Plast Esth. 2013;58(2):166-74. DOI: http://dx.doi.org/10.1016/j.anplas.2012.12.003
33. Westreich R, Meisner J, Reino A, Lawson W. The use of combined Bernard-Webster and Karapandzic flaps for subtotal lower lip reconstruction. Plast Reconstr Surg. 2008;121(5):340e-1e. DOI: http://dx.doi.org/10.1097/PRS.0b013e31816b12e9
34. Hamahata A, Saitou T, Ishkawa M, Beppu T, Sakurai H. Lower lip reconstruction using a combined technique of the Webster and Johanson methods. Ann Plast Surg. 2013;70(6):654-6. DOI: http://dx.doi.org/10.1097/SAP.0b013e318243353f
35. Sand M, Altmeyer P, Bechara FG. Mucosal advancement flap versus primary closure after vermilionectomy of the lower lip. Dermatol Surg. 2010;36(12):1987-92. DOI: http://dx.doi.org/10.1111/j.1524-4725.2010.01762.x
36. Kheramand AA, Garajei A. Ventral tongue myomucosal flap: a suitable choice for shaved lower vermilion border reconstruction. J Craniofac Surg. 2013;24(2):e114-6.
1. Universidade Federal Fluminense, Niterói, RJ, Brazil
2. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
Institution: Hospitais Universitários Clementino Fraga Filho e Antonio Pedro, Mario Kroeff e na clínica privada. Trabalho apresentado no exame para Membro Titular da Sociedade Brasileira de Cirurgia Plástica em 2014, Niterói, RJ, Brazil.
Corresponding author:
Pedro Leonardo Sanches Faveret
Rua Pinheiro Machado, 22, apto 205, bloco 2, Laranjeiras
Rio de Janeiro, RJ, Brazil Zip code 22231-090
E-mail: contato@pedrofaveret.com.br
Article received: November 17, 2014.
Article accepted: April 21, 2015.
 All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license
All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license