

Ideas and Innovation - Year 2025 - Volume 40Issue 1
Surgical Tactics in Breast Explants
Táticas cirúrgicas nos explantes mamários
ABSTRACT
Introduction Demand for breast implants and capsule removal has increased over the last 5 years. Plastic surgeons have the skills to perform capsulectomy, but there are surgical tactics details that depend on the degree of contracture and the plane of implant placement. Breast reconstruction following this procedure also has its particularities. Therefore, it would be ideal to identify the significant factors in choosing surgical tactics for intact total capsulectomy and to develop a decisionmaking flowchart to assist the surgeon in each case.
Materials and Methods Description of surgical tactics and decision-making flowchart based on the author's experience in 712 patients undergoing total intact capsulectomy from June 2021 to 2023 in São Paulo, Brazil.
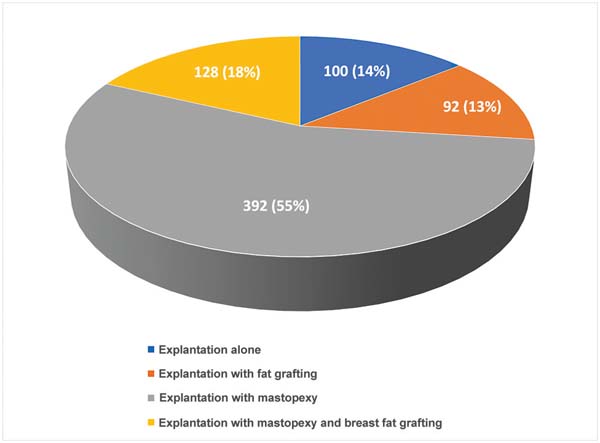
Results Most patients (78%) presented subglandular explants, followed by submuscular ones in 22%. Implants consisted of silicone alone in 89% and polyurethane coated in 11% of cases. In this series, 55% of patients underwent explantation withmastopexy, followed by explantation with mastopexy and fat grafting in 18%, explantation alone in 14%, and explantation with fat graft in 13%.
Conclusion Capsular contracture degree, implant position, and previous scarring on the breasts are important factors in surgical planning for intact total capsulectomy. The choice of breast repair tactic depends on factors such as breast volume and sagging. Observation of the decision flowchart for these procedures can be an instrument for planning and standardizing surgical tactics.
Keywords: breast; breast implantation; breast implants; implant capsular contracture; mammaplasty
RESUMO
Introdução A demanda pela remoção do implante de mama e da cápsula aumentou nos últimos 5 anos. Há detalhes de tática cirúrgica na capsulectomia que dependem do grau de contratura e do plano em que o implante está colocado. A reparação das mamas após esse procedimento também apresenta suas particularidades. Diante disso, seria ideal identificar os fatores importantes na escolha das táticas cirúrgicas na capsulectomia total intacta e desenvolver um fluxograma de tomada de decisão para auxiliar o cirurgião em cada caso.
Materiais e Métodos Descrição de tática cirúrgica e fluxograma de decisão baseado na experiência do autor em 712 pacientes submetidas à capsulectomia total intacta entre junho de 2021 e 2023 em São Paulo, Brasil.
Resultados A maior parte dos pacientes (78%) tinham implantes subglandulares, seguidos por submusculares em 22%. Os implantes eram totalmente de silicone em 89% dos casos e revestidos de poliuretano em 11%. Na casuística, 55% dos casos foram submetidos à explante com mastopexia, seguido de explante com mastopexia e lipoenxertia em 18%, explante somente em 14% e explante com lipoenxertia mamária em 13%.
Conclusão O grau de contratura capsular, a posição do implante e a cicatriz prévia nas mamas são fatores importantes no planejamento cirúrgico da capsulectomia total intacta. A escolha da tática de reparação de mama depende de fatores como volume e queda das mamas. A observação do fluxograma de decisão para esses procedimentos pode ser um instrumento para planejamento e padronização das táticas cirúrgicas.
Palavras-chave: contratura capsular em implantes; implante mamário; implantes de mama; mama; mamoplastia
Introduction
Demand for breast implant and capsule removal has been increasing over the last 5 years. This demand results from patients’ fear of local implant-related complications, including rupture and contracture, or the appearance of systemic symptoms from Asia syndrome or silicone disease.1-3
Although it is not the most proper term, conventional and social media refer to implant and capsule removal as explantation or block explantation. Patients request the removal of intact breast implants and capsules in their entirety, with no damage. Therefore, as some authors discussed, the most correct term would be intact total capsulectomy. This article uses both terms.4,5
Simple breast implant removal is less complex than capsulectomy. Plastic surgeons learn how to perform it during their training. However, each situation has specific features, such as capsular contracture and whether the implant is in a subglandular or submuscular position.6,7
Many cases require breast repair in addition to capsulectomy. Some present with ptotic breasts requiring mastopexy, and others wish to enlarge their breasts with fat grafting. Submuscular implants may require the reattachment of pectoral muscles.8,9
Given this new demand and the particularities of breast explantation and repair, it would be ideal to identify the factors for surgical tactic selection and develop a decisionmaking flowchart to assist surgeons in each case.
Objective
This study aimed to identify the significant factors for planning intact total capsulectomy and breast repair surgical tactics.
Also,toassessifadecision-makingflowchartfor intact total capsulectomy and breast repair can assist this surgical planning.
Materials and Methods
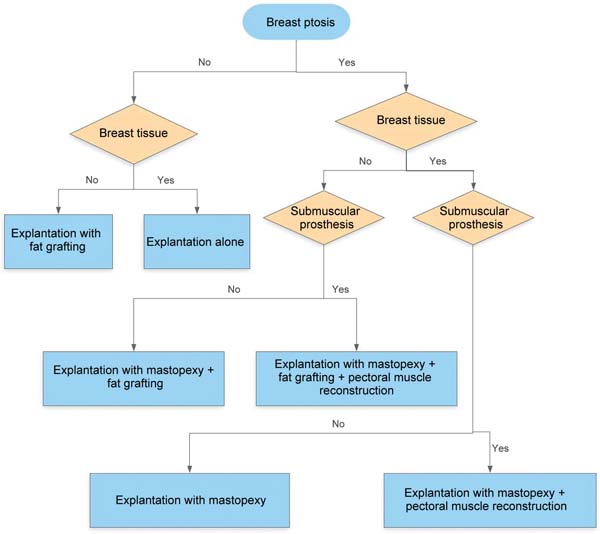
This study described surgical tactics and a decision-making flowchart based on the author’s experience with 712 patients undergoing intact total capsulectomy from June 2021 to 2023 in São Paulo, Brazil. Breast repair after intact total capsulectomy followed the flowchart presented in ►Fig. 8. The Research Ethics Committee from Plataforma Brasil approved this study under number 74568023.4.0000.5442.
Surgical tactics for intact total capsulectomy
Explantation alone, subglandular plane implantation
In these cases, the surgeon begins the incision at the previous scar, often in the inframammary fold, and continues the dissection up to the capsule. Next, the capsule is detached from the pectoralis major muscle posteriorly and from the breast tissue anteriorly.
The remaining detachment releases the breast tissue capsule from medial to lateral. This dissection can be complex in the superior or superolateral portion, so an option is to pull the implant and the capsule out of the incision to expose the attached segment for better dissection.
The implant curvature may require a mounted gauze to lower and pull the implant to access points further away from the detachment.
In the cases with previous periareolar scar, the explantation can be performed throughan incision at thescar, with anterior detachment of the capsule, followed by a detachment from medial to lateral. This tactic provides better access for the posterior detachment of the capsule between the implant and the pectoralis major. Patients with small areolas or grade III or IVcontractures (►Fig. 1) may require a lateral extension of the periareolar incision shaped like the Greek letter omega.
Explantation alone, submuscular plane implantation
The detachment sequence follows the same strategy as for subglandular plane implants. The surgeon performs the posterior detachment by dissecting the capsule from the rib periosteum and intercostal muscles. In the anterior portion, the capsule is detached from the pectoralis major muscle and, finally, it is dissected from medial to lateral (►Fig. 2).
Some cases present a capsule adhered firmly to the rib periosteum, making total intact capsulectomy unfeasible. Posterior capsule infiltration with saline solution in an attempt to create a plane does not work in the author’s practice. In cases with a firm adherence of the capsule to the periosteum, it can be cauterized.
Explantation with mastopexy, subglandular plane implantation
An explantation with mastopexy results in greater exposure. The surgeon opens the entire T-shaped incision and reflects the upper pedicle flap (►Fig. 3).
The lateral and superolateral portions of the breast, towards the axilla, show more adherence between the capsule and the pectoralis major muscle. The lateral portion detachment is less complex from medial to lateral.
After reaching the superolateral region, the detachment can be craniocaudal, following the fibers of the pectoralis major muscle to where they are attached to the ribs.
Explantation with mastopexy, submuscular plane implantation
These cases require an anterior detachment between the capsule and the pectoralis major muscle, in addition to a posterior detachment between the capsule, the intercostal muscle, and the rib periosteum. Next, the surgeon detaches the capsule from the adjacent tissues from medial to lateral.
If the adherence between the posterior capsule and the periosteum is too strong, it is possible to cauterize it and remove the anterior capsule alone.
Postintact total capsulectomy repair
With no ptosis and little breast tissue
In this case, the option is an intact total capsulectomy through the original (inframammary or periareolar) incision and observation for breast retraction.
Fat grafting can be used, often in multiple planes, starting in the deep breast tissue and proceeding superficially into the subcutaneous tissue. Grafting must include all quadrants, with special attention to the lower and medial portions, which can present breast tissue atrophy resulting from the weight of the implant.
The grafting ratio is 1:1. As such, if the estimated volume of theresidualbreastis200mL,thegraftmusthavethen200mLof fat.Theabsorptionrateisapproximately50%ofthevolume.10,11
For subglandular implant cases, the area between the pectoralismajorandminormusclescanreceive100to250mLoffat graft(►Fig.4).Forgraftingintothepectoralmuscle,theamount of fat is the maximum amount possible depending on the muscle elasticity and size. Pectoral muscles with larger areas and greater elasticity can carry a greater graft volume. The region below the pectoralis major muscle is an additional plane forfatgrafting,especiallyinpatientswiththinbreasttissue.12,13
Fat distribution occurs throughout the pectoral muscle, and its injection is in a bolus. Submuscular fat grafting increases the volume and projection in the upper part of the breast, but with inferior results in the lower part.
With no ptosis and proper breast tissue
These cases require total intact capsulectomy alone, with no need for repair. Breast fat grafting can be performed for cleavage increase, at discretion of the surgeon.
With ptosis and little breast tissue
Mastopexy can be periareolar, circumvertical, L-shaped, or Tshaped. The surgeon can perform fat grafting between the pectoralis major and minor muscles in patients with subglandular implants.
For pseudoptosis, the surgeon can perform a horizontal wedge excision of up to 3 cm in the inframammary fold, with no significant change in the areolar height. Another option is an internal mastopexy technique with sutures for pillar approximation, but with limited outcomes.14
In grade-I ptosis, periareolar mastopexy is an option, but it reduces breast projection. The author prefers to perform a circumvertical or L-shaped mastopexy in these cases.
For grade-III ptosis requiring an areolar elevation higher than 4cm, the author uses the superomedial pedicle with a Tshaped scar. For other cases, the superior pedicle is preferred (►Fig. 5) as it is easy to prepare during capsulectomy.15 For areolas firmly attached to the implant, the lower pedicle is an option to avoid a very thin upper pedicle.
The fat graft plan can be subcutaneous, in the breast tissue, or submuscular. The upper quadrant receives around 60% of the graft volume. For explantation with mastopexy, it is not recommended to perform a fat graft in a ratio greater than 1:1 of the removed implant’s volume.16,17
With ptosis and proper breast tissue
The same previous incision and pedicle selection options apply to this group of patients. These cases do not require breast fat grafting.
Pectoralis major refixation should be considered for all submuscular plane implants. Suture the pectoralis major muscle with separate X-shaped stitches at the upper edge of the sixth rib.18,19 This procedure prevents the muscle from healing in a nonanatomical position, resulting in the breast sinking or moving during contraction.
Tactics to reduce “dog ears” incidence
The decreased breast volume tends to increase skin sagging. This can potentially lead to the formation of “dog ears” on the medial and lateral corners of the inframammary fold incision (►Fig. 6).
To avoid this, when starting to suture the breast, place the patient in a sitting position with their arms along the body for skin sagging assessment. An alternative maneuver is bringing both breasts medially and downwards to assess medial sagging and placing them downwards and laterally for lateral sagging.
In addition to extending the incision to correct sagging, it is necessary to remove the corner volume by tissue resection. The first incision in the inframammary fold is beveled and directed to the lower portion, removing volume.
Results
The average age of the patients was 41.3 years, and most patients had silicone implants in the subglandular plane (►Table 1).
| N = 712 | |
|---|---|
| Mean age | 41.3 years |
| Inclusion plan and implant type: n (%) | |
| Subglandular implant | 555 (78%) |
| Submuscular implant | 157 (22%) |
| Silicone-based implant | 633 (89%) |
| Polyurethane-coated implant | 79 (11%) |
The most frequent complication was surgical wound dehiscence (►Table 2).
| Complications: n (%) | N = 712 |
|---|---|
| Dehiscence | 8 (1.12%) |
| Hematoma | 6 (0.84%) |
| Surgical wound infection | 5 (0.7%) |
| Partial areola necrosis | 1 (0.14%) |
The most performed surgery was explantation with mastopexy, with or without breast fat grafting (►Fig. 7).
►Fig. 8 shows a decision-making flowchart for breast repair after implant removal and intact total capsulectomy. ►Figs. 9 and 10 demonstrate the outcomes following these surgical tactics and the decision-making flowchart.
Discussion
The average age of the patients operated on was 41 years, reflecting the author’s reality of operating mostly on women who have had children. Some degree of breast ptosis is expected in these patients, which is consistent with the data of 55% requiring mastopexy after intact total capsulectomy in the present study.8,13
The implant was in the subglandular plane in 78% of cases, which makes total intact capsulectomy technically easier.
Polyurethane-coated prostheses were present in 11% of patients, which are associated with a thicker capsule and, therefore, a lower riskof capsule rupture during dissection.20 The incidence of complications was consistent with the literature, and the most common complications included small dehiscences at the mammary column and hematomas requiring surgical drainage. The only case of areola necrosis was partial, involving approximately 40% of the area.7
The literature and the author’s experience served as the basis for developing a decision-making flowchart for planning and discussing surgical options with patients, both in intact total capsulectomy and breast repair.8,21,22
One of the most common indications for total intact capsulectomy is capsular contracture, ranging from grades I to IV and occurring in 2.8 to 18.9% of patients.22 Grade III or IV contractures require total removal to avoid seroma or palpability.23
For grade-I and -II contractures, it is more difficult to find the detachment plane between the capsule and the breast tissue. There is a higher risk of rupture but removal is less complex through a smaller incision, as in cases of explantation alone, due to its higher elasticity.
For grade-III and -IV contractures (►Fig. 1), it is easier to find the dissection plane, and the chance of rupture is smaller. However, implant removal through a small incision is more complex due to the low elasticity of the capsule.
Capsulectomy can be partial, sparing part of the capsule. Total, in which the entire capsule is removed, with risk of tears, but removal occurs without tears in the total intact technique. In this study, all patients underwent intact total capsulectomy for standardization purposes.
In nonptotic breasts, the incision for intact total capsulectomy follows the previous one for breast implant insertion. In most cases, the previous incision was in the inframammary fold and, to a lesser extent, in the periareolar region. Although the literature describes intact total capsulectomy via the axillary approach, the author prefers to use an inframammary fold incision for implant insertion via the axillary approach.24
The removal sequence described in the methodology facilitates dissection and improves exposure of the capsule. Using the periareolar approach, dissection of the capsule’s posterior portion is harder, and the risk of breast sinking in the periareolar scar region is higher.
Capsule dissection in submuscular implants can be challenging and result in complications, such as bleeding and pneumothorax.9,20 The posterior portion of the capsule adheres firmly to the region of the rib periosteum and less to the intercostal spaces containing muscle. Dissecting thin capsules from the pectoralis major muscle is a complex procedure.
Capsulectomy in subglandular implants is technically easier. When the implant or pocket is large, it may be difficult to approach the capsule for dissection in its uppermost and superolateral portions, closer to the origin of the pectoralis major muscle. The difficulty is higher in explantation alone, as the exposure is smaller than in mastopexy.
The increased demand for implant removal resulted in a higher need for breast repair. Young patients with no ptosis do not require repair, as explantation alone can be sufficient. The retraction risk is higher when there is little breast tissue, usually occurring in the lower and medial portions, where atrophy due to implant compression is more intense.
In small breasts and subglandular implants, explantation alonecanbeperformedwithfatgraftingbetweenthepectoralis major and minor muscles, reducing the risk of retraction. Fat grafting is unfeasible below the muscle in submuscular implants. Potential complications of fat grafting include the formation of oily cysts, steatonecrosis, and infection. The volume of fat grafted influences the development of oily cysts and steatonecrosis, with incidences of 4.5 and 6.2%, respectively.18
In patients with breast ptosis and sufficient tissue, the option is explantation with mastopexy. In these cases, fat grafting is an alternative to provide a little more volume and cleavage. The author prefers the upper pedicle, which has a lower chance of pseudoptosis. It is also versatile and can be fixed in a somersault at the level of the areola or inferiorly as if it were an inferior pedicle.
For submuscular implants, breast repair follows the same principles as subglandular ones (►Fig. 8). The difference is the pectoral muscle reattachment with interrupted sutures on the upper edge of the sixth rib in submuscular cases.25
Some studies recommend explantation alone followed by mastopexy in patients with breast ptosis, smokers, with breast tissue thickness < 4 cm, or requiring areola elevation higher than 4 cm.8,21 This has not been the author’s conduct, who always performs mastopexy at the same surgical time as the explantation in ptosis cases.
Some authors recommend using an inferior pedicle to raise the areola by more than 6 to 8 cm. The inferior pedicle is an option, but it makes the explantation a little more complex and it has a higher risk of pseudoptosis. In these cases, the author has preferred a superomedial pedicle.21
The breast implant may rupture the ligaments of the inframammary fold and migrate below the fold, resulting in a double-bubble defect. These cases require an internal bra, returning the fold to its original site with sutures between the scar and the fascia of the pectoral muscle.26
One of the main complications of explantation is hematoma. To reduce it, the author prefers ligating arterial vessels instead of cauterizing them. All patients undergoing explantation, regardless of the type of repair, received number 15 Blake drains.
Additionally, the author has routinely used 1 g of tranexamic acid during induction and, after reviewing hemostasis, washes the site with a solution of 2 vials of 500 mg tranexamic acid in 10 mL of saline solution.27,28
One criticism of this study is that all patients underwent intact total capsulectomy, even in the lack of surgical indication, such as rupture, grade-III or -IV contracture, large recurrent seromas, or anaplastic large cell lymphoma. No scientific evidence supports that this surgical technique to improve the symptoms of silicone disease or Asia syndrome. Some studies demonstrated the improvement of systemic symptoms associated with breast implants regardless of the capsulectomy type, that is, total intact, total, or partial.2,5,29
Intact total capsulectomy with no surgical indication depends on the surgeon’s experience and judgment in each case. This surgery should not increase the risk of postoperative complications. Surgeons with more experience with intact total capsulectomy will naturally decrease surgical time and postoperative complications.
Conclusion
The capsular contracture degree, implant position, and previous breast scarring are significant factors in surgical planning for intact total capsulectomy. The choice of breast repair tactic after this technique depends on aspects such as breast volume and sagging.
The decision-making flowchart for intact total capsulectomy and breast repair can act as a tool for planning and standardizing surgical tactics.
REFERENCES
1. Magnusson MR, Cooter RD, Rakhorst H, McGuire PA, Adams WP Jr, Deva AK. Breast Implant Illness: A Way Forward. Plast Reconstr Surg 2019;143(3SA Reviewof BreastImplant-AssociatedAnaplastic Large Cell Lymphoma)74S-81S. Doi: 10.1097/PRS.0000000000005573
2. Glicksman C, McGuire P, Kadin M, Barnes K, Wixtrom R, Lawrence M, et al. Longevity of Post-Explantation Systemic Symptom Improvement andPotential Etiologies:Findings From the ASERF Systemic Symptoms in Women - Biospecimen Analysis Study: Part 4. Aesthet Surg J 2023;43(10):1194-1204. Doi: 10.1093/asj/sjad098
3. Swanson E. Breast Implant Illness, Biofilm, and the Role of Capsulectomy. Plast Reconstr Surg Glob Open 2020;8(07): e2999. Doi: 10.1097/GOX.0000000000002999
4. Gerzenshtein J. The Dishonesty of Referring to Total Intact Capsulectomyas“EnBloc”ResectionorCapsulectomy.PlastReconstrSurg 2020;145(01):227e-228e. Doi: 10.1097/PRS.0000000000006362
5. Glicksman C, McGuire P, Kadin M, Lawrence M, Haws M, Newby J, et al. Impact of Capsulectomy Type on Post-Explantation Systemic Symptom Improvement: Findings From the ASERF Systemic Symptoms in Women-Biospecimen Analysis Study: Part 1. Aesthet Surg J 2022;42(07):809-819. Doi: 10.1093/asj/sjab417
6. Melmed EP. A review of explantation in 240 symptomatic women: a description of explantation and capsulectomy with reconstruction using a periareolar technique. Plast Reconstr Surg 1998;101 (05):1364-1373. Doi: 10.1097/00006534-199804050-00036
7. Afshari A, Nguyen L, Glassman GE, Perdikis G, Grotting JC, Higdon KK. Incidence and Preoperative Risk Factors for Major Complications After Capsulectomy: Analysis of 3048 Patients. Aesthet Surg J 2022; 42(06):603-612. Doi: 10.1093/asj/sjac004
8. Rohrich RJ, Parker TH III. Aesthetic management of the breast after explantation: evaluation and mastopexyoptions. Plast Reconstr Surg 2007;120(01):312-315. Doi: 10.1097/01.prs.0000264400.42376.e9
9. Katsnelson JY, Spaniol JR, Buinewicz JC, Ramsey FV, Buinewicz BR. Outcomes of Implant Removal and Capsulectomy for Breast Implant Illness in 248 Patients. Plast Reconstr Surg Glob Open 2021;9(09):e3813. Doi: 10.1097/GOX.0000000000003813
10. Abboud MH, Dibo SA. Immediate Large-Volume Grafting of Autologous Fat to the Breast Following Implant Removal. Aesthet Surg J 2015;35(07):819-829. Doi: 10.1093/asj/sjv073
11. Kim HY, Jung BK, Lew DH, Lee DW. Autologous Fat Graft in the Reconstructed Breast: Fat Absorption Rate and Safety based on Sonographic Identification. Arch Plast Surg 2014;41(06): 740-747. Doi: 10.5999/aps.2014.41.6.740
12. Kandulu H, Terzibasioglu AE. Male Pectoralis Major Muscle Augmentation with Autologous Fat Transplantation Using VASER Lipoaspirate: Evaluation with MRI. Plast Reconstr Surg Glob Open 2023;11(04):e4945. Doi: 10.1097/GOX.0000000000004945
13. Herold C, Ueberreiter K, Cromme F, Grimme M, Vogt PM. [Is there a need for intrapectoral injection in autologous fat transplantation to the breast? - An MRI volumetric study]. Handchir Mikrochir Plast Chir 2011;43(02):119-124. Doi: 10.1055/s-0030-1269931
14. Scioscia PJ, Hagerty RC. Internal mastopexy following explantation. Plast Reconstr Surg 1996;97(05):1014-1019, discussion 1020-1022. Doi: 10.1097/00006534-199604001-00019
15. Azevedo DM, Pinto EBdS, Romani HM, Gonçalves Júnior P, Morela MMV, Morelli LHU. Mamoplastia redutora com cicatriz vertical assistida por lipoaspiração. Rev Bras Cir Plást 2010;25(3 Suppl 1):58. Available from: https://www.rbcp.org.br/details/668/pt-BR
16. Mangialardi ML, Ozil C, Lepage C. One-Stage Mastopexy-Lipofilling after Implant Removal in Cosmetic Breast Surgery. Aesthetic Plast Surg 2022;46(04):1542-1550. Doi: 10.1007/s00266-02102727-0
17. Graf RM, Closs Ono MC, Pace D, Balbinot P, Pazio ALB, de Paula DR. Breast Auto-augmentation (Mastopexy and Lipofilling): An Option for Quitting Breast Implants. Aesthetic Plast Surg 2019; 43(05):1133-1141. Doi: 10.1007/s00266-019-01387-5
18. Avashia YJ, Rohrich RJ, Gabriel A, Savetsky IL. Surgical Management of the Explant Patient: An Update on Options for Breast Contouring and Volume Restoration. Plast Reconstr Surg 2020; 146(05):978-985. Doi: 10.1097/PRS.0000000000007288
19. Bark AA Jr, Minikowski GC, Mujahed IBU. Multiplane L-Scar Augmentation Mastopexy: An Individualized Approach to Muscle, Glandular Tissue, and Skin. Plast Reconstr Surg 2024;153(04): 801-809. Doi: 10.1097/PRS.0000000000010850
20. Oliveira KCd, Pereira RMR, Salgado IV, Baptista EVdP, Arantes GC, Luna IC. Options for capsulotomy and capsulectomy in the treatment of capsular contracture: are there clinical treatment alternatives to surgery? A literature review. Rev Bras Cir Plást 2015;30(01):123-128. Doi: 10.5935/2177-1235.2015RBCP0127
21. Mowlavi A, Asghari A, Heydarlou D, Gavilanes E, Sin Z, Mirzania H. Breast Lift Algorithm for the Treatment of Breast Implant Illness Requiring Implant Removal. Aesthetic Plast Surg 2023;47(03): 934-943. Doi: 10.1007/s00266-022-03178-x
22. Tanna N, Calobrace MB, Clemens MW, Hammond DC, Nahabedian MY, Rohrich RJ, et al. Not All Breast Explants Are Equal: Contemporary Strategies in Breast Explantation Surgery. Plast Reconstr Surg 2021;147(04):808-818. Doi: 10.1097/PRS.0000000000007784
23. Nahabedian MY. The Capsule Question: How Much Should Be Removed with Explantation of a Textured Device? Plast Reconstr Surg 2021;147(5S):44S-50S. Doi: 10.1097/PRS.0000000000008045
24. Hung CC. Endoscopic transaxillary capsulectomy with immediate reimplantation performed as a single-operator outpatient procedure. J Plast Reconstr Aesthet Surg 2020;73(12):2225-2231. Doi: 10.1016/j.bjps.2020.05.054
25. Bark AA Jr, Minikowski GC, Moreto L, Mujahed IBU. Creating a New Inframammary Fold, Raising the Breast Footprint, and Elongating the Torso with a Multiplane Concept. Plast Reconstr Surg 2024;154 (06):1084e-1090e. Doi: 10.1097/PRS.0000000000011265
26. Atiyeh B, Ibrahim A, Saba S, Karamanoukian R, Chahine F, Papazian N. The Inframammary Fold (IMF): A Poorly Appreciated Landmark in Prosthetic/Alloplastic Breast Aesthetic and Reconstructive Surgery-Personal Experience. Aesthetic Plast Surg 2017; 41(04):806-814. Doi: 10.1007/s00266-017-0854-7
27. Weissler JM, Banuelos J, Jacobson SR, Manrique OJ, Nguyen MDT, Harless CA, et al. Intravenous Tranexamic Acid in Implant-Based Breast Reconstruction Safely Reduces Hematoma without Thromboembolic Events. Plast Reconstr Surg 2020;146(02):238-245. Doi: 10.1097/PRS.0000000000006967
28. Ausen K, Fossmark R, Spigset O, Pleym H. Safety and Efficacy of Local Tranexamic Acid for the Prevention of Surgical Bleeding in Soft-Tissue Surgery: A Review of the Literature and Recommendations for Plastic Surgery. Plast Reconstr Surg 2022;149(03): 774-787. Doi: 10.1097/PRS.0000000000008884
29. Miranda REd. What is the impact of capsulectomy on systemic symptoms attributed to silicone breast implant? Systematic literature review. Rev Bras Cir Plást 2023;38(04):e0816. Doi: 10.5935/2177-1235.2023RBCP0816-EN
1. Private practice, São Paulo, SP, Brazil
Address for correspondence Ricardo Eustáchio de Miranda, Rua Bandeira Paulista 530, sala 43, São Paulo, SP, CEP 04532-001, Brasil (e-mail: ricardomiranda@hotmail.com).
Article received: August 27, 2023.
Article accepted: May 20, 2025.
Conflict of Interests
The author has no conflict of interests to declare.






















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter