

Original Article - Year 2012 - Volume 27 - Issue 1
Surgical treatment of the sequelae of foot burns
Tratamento cirúrgico das sequelas de queimadura do pé
ABSTRACT
BACKGROUND: This article describes the sequelae of burn injuries on the feet and surgical techniques for their treatment. This paper aims to help doctors treating burn injuries by establishing parameters of normality to be sought and effective surgical techniques for treatment.
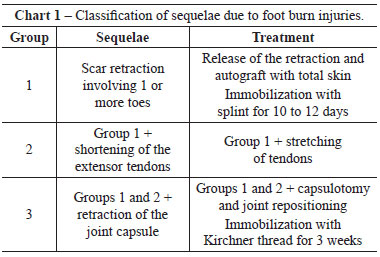
METHODS: The sequelae of burn injuries on the feet were classified into 3 groups on the basis of the degree of burns and the extent of involvement of the foot's anatomic structures. Suggested surgical approaches for each group are provided. Three patients with different deforming lesions treated surgically illustrate this classification.
RESULTS: Improvement in function was evident after using the surgical techniques in all analyzed patients.
CONCLUSIONS: There are several technical options for treating sequelae of burn injuries on the feet. The plastic surgeon must perform his/her role to assist these patients and treat these lesions. The treatment of these patients starts in the acute stage of the burn injury, during which it is necessary to prepare the area for future procedures. Restoring functionality must be the goal of the surgery, especially in growing children.
Keywords: Burns. Foot. Foot injuries. Plastic, surgery/methods.
RESUMO
INTRODUÇÃO: O artigo versa sobre as sequelas causadas por queimadura na região dos pés e as técnicas cirúrgicas para seu tratamento. Este trabalho visa a servir de auxílio a todos os médicos que tratam queimaduras, estabelecendo parâmetros de normalidade a serem buscados e técnicas cirúrgicas que auxiliem no tratamento.
MÉTODO: É apresentada classificação das sequelas de queimadura do pé em três grupos, baseando-se no grau de comprometimento de suas estruturas anatômicas, e propondo abordagens cirúrgicas distintas para cada grupo. Três pacientes com diferentes lesões deformantes ilustram essa classificação e são tratados cirurgicamente.
RESULTADOS: Houve evolução funcional com o emprego das técnicas cirúrgicas em todos os pacientes analisados.
CONCLUSÕES: Existem muitas opções técnicas para o tratamento das sequelas de queimadura do pé. É importante que o cirurgião plástico assuma seu papel na assistência cirúrgica a esses pacientes, devendo estar preparado para o tratamento dessas lesões. O manejo desses pacientes tem início na fase aguda da queimadura, havendo necessidade de preparo do local para futuros procedimentos. A devolução da funcionalidade deve ser o objetivo da cirurgia, principalmente em crianças em fase de crescimento.
Palavras-chave: Queimaduras. Pé. Traumatismos do pé. Cirurgia, plástica/métodos.
Although the feet comprise only 3.5% of the total body surface, lesions caused by burn injuries in these areas cause huge levels of morbidity and prevent patients from performing their usual activities over a long period1,2.
Since burn injury treatment is the plastic surgeon's responsibility, he/she must be prepared to treat the many types of lesions caused by burns.
The type of sequelae is determined according to the level of the burn injury, its depth, and the direct influence of the treatment during the acute stage of the burn injury.
Static inspection of the morphology of the foot would reveal the following characteristics of normality:
In a static position without support, in the plantar region, it must be possible to see 3 arches (i.e., the internal longitudinal, external longitudinal, and anterior transverse) as well as the main portions of the weight-bearing region in the plantar surface, which is characterized by the thickness of skin (Figures 1 and 2).
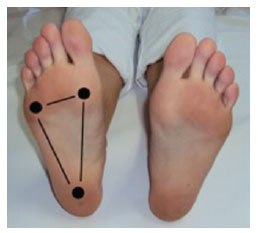
Figure 1 - Plantar support areas.

Figure 2 - Internal longitudinal arch.
In orthostatism with the full plantar surface touching the floor, the foot must be supported by 3 main points (i.e., the plantar fascia of the calcaneus, base of the first metatarsal bone, and base of the fifth metatarsal bone) with the calcaneus discreetly arched and all plantar projections of the toes touching the floor (Figures 3 and 4).

Figure 3 - Calcaneus discreet arch.

Figure 4 -Toes contacting the ground.
During the initial physical examination is when the surgeon knows what to do, by touching the affected area and realizing the extent of skin loss during palpation.
The abovementioned characteristics of normality3,4 must be kept in mind throughout treatment in order to formulate a clear and objective surgical plan. Surgery aims to restore the functionality of the structures involved; preserving aesthetics is the secondary objective.
This paper presents cases operated on using different techniques to correct sequelae resulting from foot burn injuries at the Plastic Surgery Service of Faculdade de Medicina de Nova Iguaçu (Nova Iguaçú Medical School), Hospital da Plástica (Rio de Janeiro, RJ, Brazil).
METHODS
An anatomic and functional evaluation of the foot was performed to establish the parameters of normality to be sought during the correction of deformities caused by burn injuries.
A proper classification was developed by dividing the sequelae from foot burn injuries into 3 groups (Chart 1). We adopted individual approaches and treatments for each group according to the seriousness of the injury, depth of burns, and involvement of structures.
Three cases that exhibited clearly different sequelae resulting from burn injuries and potential techniques to be used for treatment were selected.
Cases of burn injuries in the acute stage were excluded.
The first group was characterized by a lack of skin coverage on the dorsal side leading to the retraction of 1 to all toes. Case 1 exemplifies this group.
The proposed treatment consisted of the surgical release of the scar retraction, positioning of the toes in an anatomical position, and total skin autografting. The preferred donor areas for all 3 groups are the lower abdominal and inguinal regions.
The second group, exemplified by case 2, consisted of patients exhibiting the sequelae present in the first group in addition to being aggravated by the shortening of the extensor tendons and subsequent dorsiflexion of the metatarsophalangeal joints without stiffness.
The proposed treatment consists of the surgical release of the scar retraction, elongation of the compromised tendons using the union of 2 adjoining tendons or tendinous elongation of the tendon itself, positioning of the toes in an anatomical position, and total skin autografting.
This technique obtains 2 tendons for toes 2 to 5 (i.e., 1 tendon for 2 toes). No motor deficits are usually observed because the toes tend to undergo extension together.
If the retracted tendon is sufficiently thick, another option for tendinous elongation is the hemisection of the tendon at different levels and subsequent tenorrhaphy of the resultant stumps.
As in the first group, the bandage was opened after 5 to 7 days to inspect the graft; the bandage was then reapplied, and a plaster splint was placed and left for 10 to 12 days.
The third group includes cases in which the changes that occur in the first 2 groups are associated with the retraction of the joint capsule. In addition to the procedures adopted in the first 2 groups, dorsal capsulotomy, release of the collateral ligaments with the repositioning of the joint, and fixation in an anatomical position with the use of Kirschner thread were performed when necessary and kept for 3 weeks. Case 3 exemplifies this group.
RESULTS
Group 1
Group 1, characterized by scar retraction involving 1 or more toes, is exemplified by the case of a 25-year-old steel worker who received a burn injury caused by liquid metal that fell on his boot (Figure 5).

Figure 5 - Group 1 patient. In A, the aspect of burns treated with grafting in the acute phase showing a large longitudinal bridle and evident hypertrophy on the dorsum of the foot. In B, the lack of skin on the metatarsophalangeal region with incision markings aiming for longitude and transverse elongation. In C, a large bloody area is apparent after the completion of the planned incisions, indicating a need for skin coverage. In D, correction of the hypertrophy of the dorsum with the restoration of the interdigital commissures, full support of the toes on the ground, and the ability to flex them by repositioning the skin coverage promoted by the autograft.
The patient complained about pain in the burned region and was treated with grafting in the acute phase. He presented with a large longitudinal bridle, obvious hypertrophy on the foot dorsum, and a consequent lack of local skin coverage.
In the physical examination, a lack of skin in the metatarsophalangeal region was observed. Incisions aiming for longitudinal and transverse elongation were marked.
A large bloody area was apparent after the planned incisions, evidencing the need for skin grafting. The incisions were made irregularly in order to avoid a late scar bridle.
Dorsum hypertrophy was corrected, restoring the interdigital commissures with full placement of the toes on the floor as well as flexion ability by the replacement of skin by the autograft.
Group 2
Group 2, characterized by scar retraction involving 1 or more toes as well as shortening of the extensor tendons, is exemplified by the case of a 5-year-old patient who was burned by boiling oil at home (Figure 6).

Figure 6 - Group 2 patient. In A, important scar retraction due to the nongrafting in the acute phase of the burn injury. The misalignment of the toes without ground contact and hallux deviation is observed. In B, visible longitudinal gain of the foot with the descent of the toes and improved plantar support. In C, second surgery for refinement. As in case 1, broken incisions and skin grafting restored the interdigital commissures and alignment of the toes. In D, the second surgery restored not only the full contact of the toes with the ground, but their full flexion as well.
The child presented with greater scar retraction than the first case as a result of the nonperformance of grafting in the acute phase of the burn injury; this emphasizes the effect of a greater lack of skin. The toes were misaligned and did not contact the floor. In addition, deviation of the hallux was apparent.
After the procedure, there was a visible longitudinal elongation of the foot with the descent of the toes and improvement of plantar support, allowing the growth of the patient. However, there was still an obvious need for further surgery.
The second surgery was performed for refinement. As in the case of patient 1, irregular incisions and skin grafting were performed in order to restore the interdigital commissures and alignment of the toes.
Not only did the procedure allow the toes to fully contact the ground, it allowed their complete flexion, which was demonstrated by maneuvering with the surgeon's hand.
Group 3
Group 3, which was characterized by the same aspects of groups 1 and 2 in addition to retraction of the joint capsule, was exemplified by the case of a 3-year-old patient who was a victim of a burn injury caused by alcohol at home (Figure 7).

Figure 7 - Group 3 patient. In A, a large bridle extending from the knees to the dorsum of the foot with the involvement of the tibiotarsal joint. In B, the bridle was interrupted by transportation flaps and full-thickness skin grafts taken from the abdomen. Fixation with Kirchner threads in the neutral position of the hallux as well as the calcaneus with the tibia was performed, restoring the 90º angle of the tibiotarsal joint. In C, postoperative period, emphasizing the plantar support obtained.
In this case, there was great concern for the restoration of the 90º angle of the tibiotarsal joint, which was compromised by a large bridle that extended from the knee to the dorsum of the foot. The bridle was interrupted with transposition flaps and total skin grafts taken from the abdomen. Fixation with Kirchner threads of the hallux in a neutral position as well as the calcaneus with the tibia restored the 90º angle of the tibiotarsal joint. The treatment was ultimately successful: the patient was already on plantar support, ambulating, returning to her usual activities, and resuming normal development with no delays.
DISCUSSION
As seen in the cases presented above, the sequelae of severe foot burn injuries result in the complete loss of function of the involved structure. It is evident that the basic issue in burn injuries is skin loss.
The objective of treatment is to restore the sole and toes to their natural positions. The patient's foot function should be restored as soon as possible.
The surgical techniques employed should stem from basic principles including grafting and flaps, reserving microsurgery for more complex and deeper cases that these principles cannot solve. It is important to note that burned areas do not tolerate detachments. Therefore, skin grafting must be considered since tensioning sutures are useless when there is loss of skin.
Comparing the patients from groups 1 and 2 (Figures 5 and 6) revealed differences between an initially well-handled case that received correct treatment in the acute phase and another inadequately handled case that presented with more severe sequelae. This highlights the importance of the preparation of the team assisting burn patients from the acute phase to late complications represented by sequelae.
CONCLUSIONS
Sequelae of foot burn injuries occur more frequently in the dorsal region because the skin is thinner and less resistant to heat. In addition, the patient is usually in an orthostatic position (i.e., plantar support) when the burn injury occurs.
These lesions reduce the tibiotarsal joint extension and dorsiflexion of the metatarsophalangeal, eliminating the plantar support of the toes.
Skin grafting usually releases the lesions. However, tendinous elongation is sometimes necessary.
In cases involving greater compromise of deep structures, distance flaps, microsurgical or not, may be considered.
REFERENCES
1. Lima Jr. EM, Novaes FN, Piccolo NS, Serra MCVF. Tratado de queimaduras no paciente agudo. 2ª ed. São Paulo: Atheneu; 2008.
2. Brown DI, Borschel GH. Manual de cirurgia plástica de Michigan. Rio de Janeiro: Di Livros; 2006.
3. Viladot PA. Dez lições de patologia do pé. São Paulo: Roca; 1986.
4. Pardini A, Souza G, Salomão O. Clínica ortopédica: atualização em cirurgia do pé e tornozelo. São Paulo: Guanabara Koogan; 2001.
1. Full member of Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery) - SBCP, plastic surgeon working in a private clinic, assistant professor of Faculdade de Medicina de Nova Iguaçu (Nova Iguaçú Medical School), Hospital da Plástica, Rio de Janeiro, RJ, Brazil.
2. General surgeon, studying Plastic Surgery in a post-graduate course at Faculdade de Medicina de Nova Iguaçu (Nova Iguaçú Medical School), Hospital da Plástica, Rio de Janeiro, RJ, Brazil.
3. Full member of SBCP, plastic surgeon working in a private clinic, assistant professor of Post-Graduation Course in Plastic Surgery of the Pontifícia Universidade Católica do Rio de Janeiro, Rio de Janeiro, RJ, Brazil.
4. Full member of SBCP, director of the SBCP Accredited Education and Service Department, director of Plastic Surgery Service at Faculdade de Medicina de Nova Iguaçu (Nova Iguaçú Medical School), Hospital da Plástica, chief executive officer of Hospital da Plástica, Rio de Janeiro, RJ, Brazil.
5. Expert in Orthopedics and Traumatology accredited by the Sociedade Brasileira de Ortopedia e Traumatologia (Brazilian Orthopedics and Traumatology Society), full member of the Sociedade Brasileira de Medicina e Cirurgia do Pé (Brazilian Society of Medicine and Surgery of the Foot), Umuarama, PR, Brazil.
Luiz Mário Bonfatti Ribeiro
Hospital da Plástica
Rua Sorocaba, 552 - Botafogo
Rio de Janeiro, RJ, Brazil - CEP 22271-110
Email: lmbonfatti@uol.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: January 26, 2012
Article accepted: March 7, 2012
Study conducted at the Faculdade de Medicina de Nova Iguaçu (Nova Iguaçú Medical School), Hospital da Plástica, Rio de Janeiro, RJ, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter