

Review Article - Year 2012 - Volume 27 -
Complications of classical liposuction performed for cosmetic purposes
Complicações em lipoaspiração clássica para fins estéticos
ABSTRACT
Liposuction for esthetic purposes aims to remove fat in healthy patients and reduce localized fat accumulation, called lipodystrophy, in order to improve body contour. In the last 3 decades, the liposuction technique has improved dramatically. However, like any other surgical procedure, it is not without complications. Here, we reviewed the literature on PubMed to identify complications after classic liposuction performed solely for esthetic purposes. In total, 210 articles were found using the term "complication in liposuction," 86 with "complication after liposuction," 27 with "fat embolism after liposuction," 7 with "fat embolism following liposuction," and 16 with "deaths related to liposuction." Among these articles, only 84 including cases of fat embolism after liposuction, visceral perforation, vascular injury, blindness, and herpes zoster infection among others were considered to be related to the subject. Based on the analyzed articles, we can conclude that liposuction is a highly effective procedure when well indicated and performed accurately. Despite this, there are inherent risks. This review found many articles addressing complications, predominantly pulmonary fat embolism, after liposuction for esthetic purposes.
Keywords: Lipectomy. Postoperative complications. Fat embolism.
RESUMO
A lipoaspiração realizada para procedimentos estéticos tem como objetivo a retirada de gordura em pacientes saudáveis e redução do acúmulo de gordura localizada, a chamada lipodistrofia, levando à melhora no contorno corporal. Nas últimas três décadas, a lipoaspiração vem sendo aperfeiçoada; porém, como qualquer outro procedimento cirúrgico, não é isenta de complicações. O objetivo deste estudo é realizar revisão da bibliografia, por meio do PubMed, identificando as complicações após lipoaspiração clássica, incluindo apenas aquelas realizadas com finalidade estética. Foram encontrados 210 artigos empregando a expressão "complication in liposuction", 86 artigos com "complication after liposuction", 27 artigos com "fat embolism after liposuction", 7 artigos com "fat embolism following liposuction" e 16 artigos com "deaths related to liposuction". Dentre esses artigos, apenas 84 foram considerados relacionados ao assunto, sendo encontrados casos de embolia gordurosa após lipoaspiração, perfuração visceral, lesão vascular, cegueira e infecção por herpes zoster, entre outros relatos. Com base nos artigos analisados foi possível concluir que a lipoaspiração é um procedimento altamente eficaz quando bem indicado e bem realizado, porém existem riscos inerentes ao ato cirúrgico. Este levantamento constatou que existem muitos artigos abordando complicações após lipoaspiração para fins estéticos, e a embolia gordurosa pulmonar apresenta alta incidência.
Palavras-chave: Lipectomia. Complicações pós-operatórias. Embolia gordurosa.
Liposuction performed as an esthetic procedure for the removal of fat in healthy patients is intended to reduce localized fat accumulation, called lipodystrophy, and improve body contour. In the last 3 decades, the liposuction procedure has undergone improvements to reduce the invasiveness of the surgery and preserve local circulation1,2. According to the statistics of the American Society of Plastic Surgeons (ASPS), approximately 198,000 individuals underwent liposuction in the United States in 20093, making it the 4th most common esthetic procedure. The Datafolha Institute and the Brazilian Society of Plastic Surgery (BSPS)4, which is among the largest plastic surgery entities worldwide, report that 629,000 plastic surgeries per year are performed in Brazil, and 73% of them are esthetic and 27% are reconstructive. Among the esthetic surgical procedures, 20% are liposuctions, second only to breast augmentation. More than 90,000 liposuction surgeries per year are carried out in Brazil4.
However, like any other surgical procedure, liposuction is not without local or systemic complications. Among several local complications, the most predominant are irregularities in the skin (visible and tangible), prolonged edema, ecchymosis, hyperpigmentation, changes in skin sensitivity, seromas, hematomas, lipodystrophy, insufficient correction, ulcers, necrosis of the skin, local infections, contact dermatitis, unesthetic scars, and persistent edema. Systemic complications of classic liposuction include visceral perforations, allergic reactions to medications during intra- and postoperative care, fever, systemic infection, cardiac arrhythmias, tachycardia, anemia, hypovolemic shock, pulmonary thromboembolism, severe vein thrombosis, fat embolism, fat embolism syndrome, sepsis, and even death5-8. Cases of complications, especially severe ones, are discussed extensively by the media and general population.
The objective of this study was to review the literature on PubMed to identify the complications associated with classic liposuction performed solely for esthetic purposes.
METHODS
The research was performed using the MEDLINE/PubMed database from July 2010 to March 2011. All published articles assessing complications in liposuction carried out for esthetic purposes were evaluated regardless of whether other surgical procedures were performed. The following search terms were used: "complication after liposuction," "complication in liposuction," "fat embolism after liposuction," "fat embolism following liposuction," and "deaths related to liposuction."
Articles were divided into case reports, experimental studies, complications in isolated liposuctions, or complications associated with other procedures. In total, 84 articles of interest were found after excluding all duplicate and irrelevant works and those not meeting the aim of the present study.
RESULTS AND DISCUSSION
In total, 210 articles were found using the expression "complication in liposuction," 86 with "complication after liposuction," 27 with "fat embolism after liposuction," 7 with "fat embolism following liposuction," and 16 with "deaths related to liposuction."
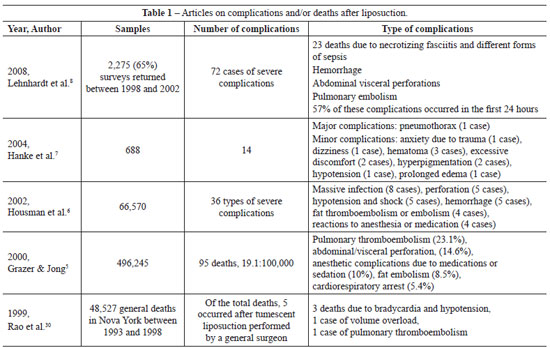
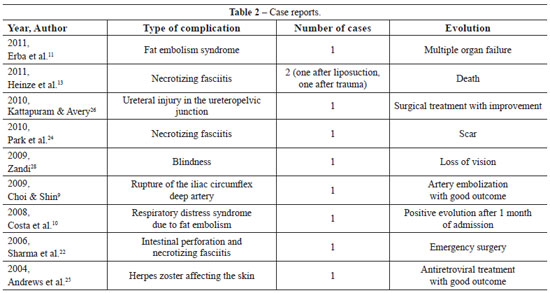
After careful selection and 5 different searches, we found 41 case reports9-17. Of these, 3 reported death after liposuction for esthetic purposes, and 2 of these reports were published in the last 5 years13,16. We also found 4 experimental studies on liposuction complications18-21.
Unusual complications were as follows: 1 case of vascular injury with perforation of a large vessel during liposuction9; 2 cases of intestinal perforation22; 4 articles reporting severe bacterial infections after liposuction23,24; 1 case of herpes zoster25; 1 case of urethral injury26; and 3 articles on vision loss associated with liposuction. However, there was 1 article which described a patient who previously had idiopathic intracranial hypertension, being two of these symptoms presented in the last five years27,28.
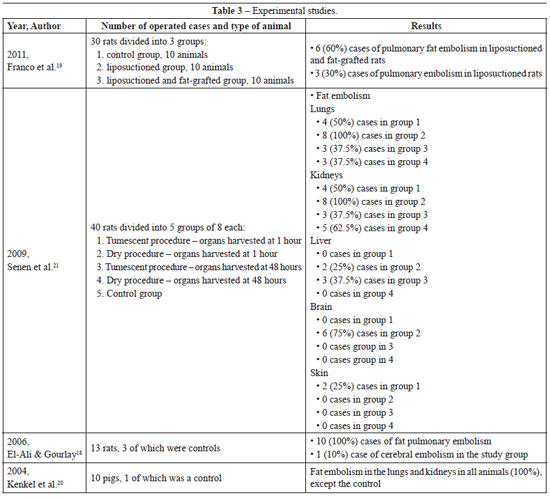
Four well-executed experimental studies addressing the complications of liposuction were selected18-21; 3 of these studies were carried out using Wistar rats, while the other 1 used pigs. These works assessed the variable incidence of pulmonary embolism after liposuction. The incidences of pulmonary embolism in rats after liposuction are higher in the studies performed by El-Ali & Gourlay18 and Senen et al.21 than that in the study carried out by Franco et al.19.
Pulmonary fat embolism after liposuction is often undiagnosable since the clinical presentation can vary greatly, ranging from slight dyspnea, tachycardia, elevated temperature, and petechiae on the skin to severe cases of respiratory failure and death. Its symptoms are nonspecific and often confused with those of pulmonary thromboembolism, thus resulting in severe vein thrombosis10,12,17,19. Although the exact risk of developing fat pulmonary embolism has not been established, death occurs in 15% of diagnosed cases. Mentz14 poses a relevant question: "how many subclinical cases were undetected, thus not being diagnosed and published so far?"
Grazer & Jong5 present a table of articles detailing the highly variable incidence of mortality in liposuction: from 3 per 100,000 cases of elective abdominal wall hernia and up to 162 per 100,000 cases.
Teimourian & Rogers29 retrospectively studied 75,000 cases and report the incidence of complications to be >0.1%; the complications include severe venous thrombosis, pulmonary thromboembolism, fat embolism, skin loss, anesthetic complications, cardiac arrhythmias, organ perforation, bleeding, and transfusion-related complications. They reported that 2 patients died as a result of fat embolism and thromboembolism, with an incidence of 2.6 per 100,000.
Costa et al.10 describe the case of a Caucasian woman, who underwent bilateral mastopexy, abdominal liposuction, and fat grafting in the gluteus; on the third postoperative day, she developed progressive dyspnea and dry cough without other symptoms and was hospitalized in the intensive care unit. Clinical examination revealed tachypnea, tachycardia, and hypoxia in room air without alterations in pulmonary auscultation; radiography showed minimal bilateral interstitial infiltrate. The patient's condition worsened on the second day of hospitalization with the development of respiratory acidosis and was intubated and placed on assisted ventilation. After several examinations, she was diagnosed with acute respiratory failure secondary to fat embolism syndrome. The patient's condition improved after 8 days of intubation; she was then extubated and discharged after 1 month of hospitalization.
Although fat embolism is a rare complication of liposuction, it has serious consequences and several cases have been reported. However, its symptoms are nonspecific and often underestimated because the exact risk of developing this complication after liposuction has not been established. Fat embolism syndrome is defined as the presence of 2 of the following 3 clinical symptoms in the first 48 hours after trauma: petechiae on the skin, pulmonary discomfort, and mental disorder. According to Costa et al.10, these findings are defined according to the criteria of Gurd and Wilson and are used to aid diagnosis. According to Mentz14, a lesion in the fatty tissues and blood vessels can occur during the liposuction procedure, causing a massive release of fat emboli into the bloodstream. After liposuction, the residual particles of fat globules and lipids in the treated area enter the circulation. The fat particles and/or triglycerides that enter the venous circulation mechanically obstruct the pulmonary circulation or promote an inflammatory local reaction; in turn, these conditions trigger endothelial damage, causing pulmonary spasms, hemorrhage, edema, and pulmonary impairment. Emboli passing through the pulmonary circulation may damage the brain, kidneys, liver, and other organs, leading to further complications. The presence of fat droplets in both lung lavage and urine has been detected in fat embolism syndrome and is associated with symptoms such as tachycardia, tachypnea, elevated temperature, hypoxia, thrombocytopenia, and neurological disorders. After suspected diagnosis, clinical support is the designated treatment14.
The collected data are presented in Tables 1 to 3.
CONCLUSIONS
Liposuction is a highly effective procedure when well indicated and performed accurately. However the risks associated with this surgical procedure need to be studied and understood in greater detail. We searched MEDLINE/PubMed and selected 84 articles of interest addressing the complications of liposuction performed solely for esthetic purposes. Fat embolism is a major complication reported in the articles studied and has also been demonstrated in experimental studies. Therefore, it should receive more attention since it's incidence after liposuction is relatively high regardless of whether it is associated with fat grafting. The experimental study of Franco et al.19 highlights this potential risk; moreover, several other studies report patients that developed respiratory distress as a result of pulmonary embolism.
The incidence of complications resulting from fat embolism in humans is still low, probably due to the lack of studies or difficulty in diagnosis, especially in cases with unclear clinical symptoms. The postoperative period following liposuction surgery in humans requires more attention and a higher commitment of doctors who perform this procedure. Moreover, when diagnosed, these cases should be published in proper medical literature to further establish the actual incidence and complications of fat mobilization, which are very evident in several experimental studies18-21. New studies emphasizing clinical significance are needed as well as experimental research and clinical studies on this controversial issue; these studies will be of great interest for general population and surgeons who work in this area.
Furthermore, in young patients and healthy patients in most cases, very little morbidity and mortality is expected during the intra- and postoperative periods of any type of surgical procedure such as liposuction.
REFERENCES
1. Illouz YG. Body contouring by lipolysis: a 5-year experience with over 3000 cases. Plast Reconstr Surg. 1983;72(5):591-7.
2. Katz BE, Bruck MC, Coleman WP 3rd. The benefits of powered liposuction versus traditional liposuction: a paired comparison analysis. Dermatol Surg. 2001;27(10):863-7.
3. American Society of Plastic Surgeons. Top 5 cosmetic procedures: statistics. Disponível em: http://www.plasticsurgery.org/Documents/news-resources/statistics/2009-statistics/2009-top-5-cosmetic-surgery-procedures-graph.pdf.
4. Sociedade Brasileira de Cirurgia Plástica. Cirurgia plástica no Brasil. Pesquisa Datafolha 2009. Disponível em: http://www2.cirurgiaplastica.org.br/images/Docs/pesquisa2009.pdf.
5. Grazer FM, Jong RH. Fatal outcomes from liposuction: census survey of cosmetic surgeons. Plast Reconstr Surg. 2000;105(1):436-46.
6. Housman TS, Lawrence N, Mellen BG, George MN, Filippo JS, Cerveny KA, et al. The safety of liposuction: results of a national survey. Dermatol Surg. 2002;28(11):971-8.
7. Hanke W, Cox SE, Kuznets N, Coleman WP 3rd. Tumescent liposuction report performance measurement initiative: national survey results. Dermatol Surg. 2004;30(7):967-77.
8. Lehnhardt M, Homann HH, Daigeler A, Hauser J, Palka P, Steinau HU. Major and lethal complications of liposuction: a review of 72 cases in Germany between 1998 and 2002. Plast Reconstr Surg. 2008;121(6):396e-403e.
9. Choi H, Shin T. Rupture of a deep circumflex iliac artery after abdominal liposuction: treatment with selective arterial transcatheter embolization. Cardiovasc Intervent Radiol. 2009;32(6):1288-90.
10. Costa AN, Mendes DM, Toufen C, Arrunátegui G, Caruso P, Carvalho CR. Adult respiratory distress syndrome due to fat embolism in the postoperative period following liposuction and fat grafting. J Bras Pneumol. 2008;34(8):622-5.
11. Erba P, Farhadi J, Schaefer DJ, Pierer G. Fat embolism syndrome after combined aesthetic surgery. J Plast Surg Hand Surg. 2011;45(1):51-3.
12. Gravante G, Araco A, Sorge R, Araco F, Nicoli F, Caruso R, et al. Pulmonary embolism after combined abdominoplasty and flank liposuction: a correlation with the amount of fat removed. Ann Plast Surg. 2008;60(6):604-8.
13. Heinze S, Püschel K, Tsokos M. Necrotizing fasciitis with fatal outcome: a report of two cases. Forensic Sci Med Pathol. 2011;7(3):278-82.
14. Mentz HA. Fat emboli syndromes following liposuction. Aesthetic Plast Surg. 2008;32(5):737-8.
15. Sherman JE, Fanzio PM, White H, Leifer D. Blindness and necrotizing fasciitis after liposuction and fat transfer. Plast Reconstr Surg. 2010;126(4):1358-63.
16. Terranova C, Sartore D, Snenghi R. Death after liposuction: case report and review of the literature. Med Sci Law. 2010;50(3):161-3.
17. Wessman DE, Kim TT, Parrish JS. Acute respiratory distress following liposuction. Mil Med. 2007;172(6):666-8.
18. El-Ali KM, Gourlay T. Assessment of the risk of systemic fat mobilization and fat embolism as a consequence of liposuction: ex vivo study. Plast Reconstr Surg. 2006;117(7):2269-76.
19. Franco FF, Tincani AJ, Meirelles LR, Kharmandayan P, Guidi MC. Occurrence of fat embolism after liposuction surgery with or without lipografting: an experimental study. Ann Plast Surg. 2011;67(2):101-5.
20. Kenkel JM, Brown SA, Love EJ, Waddle JP, Krueger JE, Noble D, et al. Hemodynamics, electrolytes, and organ histology of larger-volume liposuction in a porcine model. Plast Reconstr Surg. 2004;113(5):1391-9.
21. Senen D, Atakul D, Erten G, Erdogan B, Lortlar N. Evaluation of the risk of systemic fat mobilization and fat embolus following liposuction with dry and tumescent technique: an experimental study on rats. Aesthetic Plast Surg. 2009;33(5):730-7.
22. Sharma D, Dalencourt G, Bitterly T, Benotti PN. Small intestinal perforation and necrotizing fasciitis after abdominal liposuction. Aesthetic Plast Surg. 2006;30(6):712-6.
23. Araco A, Zaccheddu R, Araco F, Gravante G. Methicillin-resistant superinfection of the wound after body-contouring abdominal surgery. Aesthetic Plast Surg. 2008;32(4):681-3.
24. Park SY, Jeong WK, Kim MJ, Lee KM, Lee WS, Lee DH. Necrotising fasciitis in both calves caused by Aeromonas caviae following aesthetic liposuction. J Plast Reconstr Aesthet Surg. 2010;63(9):e695-8.
25. Andrews TR, Perdikis G, Shack RB. Herpes zoster as a rare complication of liposuction. Plast Reconstr Surg. 2004;113(6):1838-40.
26. Kattapuram TM, Avery LL. Ureteral tear at the ureteropelvic junction: a complication of liposuction. Emerg Radiol. 2010;17(1):79-82.
27. Ribeiro Monteiro ML, Moura FC, Cunha LP. Bilateral visual loss complicating liposuction in a patient with idiopathic intracranial hypertension. J Neuroophthalmol. 2006;26(1):34-7.
28. Zandi I. Blindness: a rare complication of liposuction: report of a case of unilateral blindness; notes on the effect of compassionate care. Plast Reconstr Surg. 2009;123(6):211e-2e.
29. Teimourian B, Rogers WB 3rd. A national survey of complications associated with suction lipectomy: a comparative study. Plast Reconstr Surg. 1989;84(4):628-31.
30. Rao RB, Ely SF, Hoffman RS. Deaths related to liposuction. N Engl J Med. 1999;13;340(19):1471-5.
1. Expert member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery) - SBCP, Doctorate in Surgery Sciences, Faculdade de Ciências Médicas da Universidade Estadual de Campinas (Faculty of Medical Sciences of the State University of Campinas) - FCM-Unicamp, volunteer plastic surgeon of the Plastic Surgery Course at FCM-Unicamp, Campinas, SP, Brazil.
2. Full member of SBCP, post-graduate student of the Department of Surgery of FCM-Unicamp, volunteer plastic surgeon of Plastic Surgery Discipline at FCM-Unicamp, Campinas, SP, Brazil.
3. Associate professor and teacher of Head and Neck Surgery Course of FCM-Unicamp, Campinas, SP, Brazil.
4. Full member of SBCP, Professor Doctor of Plastic Surgery Course of FCM-Unicamp, Chief of Plastic Surgery Service of FCM-Unicamp, Campinas, SP, Brazil.
Fernando F. Franco
State University of Campinas, Faculty of Medical Science
Department of Surgery, Plastic Surgery Course
Rua Tessália Vieira de Camargo, 126 - Cidade Universitária Zeferino Vaz - Barão Geraldo
Campinas, SP, Brazil - CEP 13083-887
E-mail: ffranco@fcmunicamp.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: April 28, 2011
Article accepted: October 6, 2011
Study conducted in the Plastic Surgery Course at the Department of Surgery of the Faculdade de Ciências Médicas da Universidade Estadual de Campinas (Faculty of Medical Sciences at the State University of Campinas) - FCM-Unicamp, Campinas, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter