

Original Article - Year 2012 - Volume 27 -
Reverse-flow sural flap: 10 years of clinical experience and modifications
Retalho sural de fluxo reverso: 10 anos de experiência clínica e modificações
ABSTRACT
BACKGROUND: The reverse flow sural flap has been featured as a relevant option for reconstruction of the distal region of the legs and feet. However, some common mistakes are made while surgeons are learning how to employ this flap. The aim of this study was to analyze use of the flap by surgeons in with 10 years of experience by comparing the first 5 years to the last 5 years in order to identify technical alterations that contribute to better results. This study also aimed at alerting the surgeons in the learning phase regarding the most important details that should be addressed when using this technique.
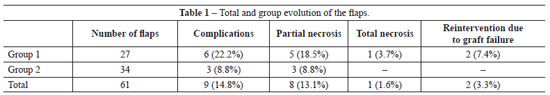
METHODS: We studied the results obtained for 61 reverse flow sural flaps used from January 2002 to December 2011. The patients were divided into 2 groups: group 1, patients that underwent surgery from January 2002 to December 2006 and group 2, patients that underwent surgery from January 2007 to December 2011. In group 2, we made changes to the fasciocutaneous flaps that included dissection of a fasciosubcutaneous margin exceeding the cutaneous portion of the flap and preservation of a lane of skin over the pedicle.
RESULTS: In group 1, the incidences of partial necrosis and total necrosis were 18.5% and 3.7%, respectively, whereas group 2 had an 8.8% incidence of partial necrosis and no cases of total necrosis.
CONCLUSIONS: The reverse flow sural flap is a good option for the treatment of the distal region of the legs and feet. Experience with this technique and the additional cautions described herein may contribute to even better results.
Keywords: Surgical flaps. Reconstructive surgical procedures/methods. Leg injuries/surgery.
RESUMO
INTRODUÇÃO: O retalho sural de fluxo reverso tem se destacado como importante opção para reconstrução da região distal de pernas e pés. Alguns erros, porém, são comuns na fase de aprendizagem de emprego desse retalho. O objetivo deste estudo é analisar 10 anos de experiência com o emprego do retalho, comparando os primeiros 5 anos aos 5 anos subsequentes, buscando identificar se as alterações técnicas introduzidas contribuíram para obtenção de melhores resultados. Este estudo busca, ainda, alertar para os principais cuidados que os cirurgiões que estão em fase de aprendizagem da técnica devem tomar.
MÉTODO: Foram estudados os resultados obtidos em 61 retalhos surais de fluxo reverso realizados no período de janeiro de 2002 a dezembro de 2011. Os pacientes foram alocados em dois grupos: grupo 1, constituído por pacientes operados de janeiro de 2002 a dezembro de 2006; e grupo 2, pacientes operados de janeiro de 2007 a dezembro de 2011. No grupo 2, foram realizadas alterações nos retalhos fasciocutâneos, como dissecção de uma borda fasciossubcutânea excedendo a porção cutânea do retalho e preservação de uma faixa de pele sobre o pedículo.
RESULTADOS: No grupo 1, a incidência de necrose parcial foi de 18,5% e de necrose total, de 3,7%; no grupo 2, houve 8,8% de necrose parcial e nenhum caso de necrose total.
CONCLUSÕES: O retalho sural de fluxo reverso é uma boa opção para o tratamento da região distal de pernas e pé. A experiência com a técnica e os cuidados implementados sugerem obtenção de melhores resultados.
Palavras-chave: Retalhos cirúrgicos. Procedimentos cirúrgicos reconstrutivos/métodos. Traumatismos da perna/cirurgia.
The leg contains a thin subcutaneous layer and few muscles, thus, the tibia and tendons can easily become exposed due to trauma. Therefore, leg injuries are often associated with a loss of soft tissues and exposed fractures. Because the skin in this region has low flexibility and the subcutaneous circulation does not allow the use of long randomized flaps, the task of finding regional flaps to cover bones or tendons in wounds with cutaneous loss in the legs and feet is difficult.
The sural flap acts as an axial flap and has 3 sources of nutrition: the vascular plexus of the deep fascia; the medial superficial sural artery, which follows the medial sural nerve; and the arteries that follow the minor saphenous vein1,2. Venous return is ensured by the minor saphenous vein3, which may be used as a distal pedicle to provide reverse flow. This vein must be preserved at least as high as the caliber perforator of the fibular artery, which is located 5-cm above the lateral malleolus and spreads with the medial superficial sural artery1,2.The reverse flow sural flap without microsurgery is one of the few treatment options in the distal regions of the legs and feet.
Several studies have shown good results with the use of this flap4-13. Because several errors are common during the learning phase of this technique, describing these errors may improve the initial results and may support the continued use of this flap. In this study, our goal was to describe the most frequent errors and to share important details that might decrease the incidence of complications.
METHOD
A retrospective study of reverse flow sural flaps was performed from January 2002 to December 2011 as a continuance of the work of a master's thesis defended in 2004. The results obtained for 61 sural flaps were evaluated: 27 cases from January 2002 to December 2006 (group 1) and 34 cases from January 2007 to December 2011 (group 2). Although most patients came from public hospitals where the author worked, some cases were from his private clinic.
The etiology of the lesions varied and included tumors, firearm injuries, motorcycle accidents, car accidents involving pedestrians, chronic ulcers, and chronic osteomyelitis. Most cases resulted from acute trauma like car and motorcycle accidents, with a loss of large parts of soft tissue in the distal area of the leg and bone exposure, with or without fracture. We compared the incidence of complications in the first 5 years (group 1) with those in the subsequent 5 years (group 2) to decrease the bias related to the learning curve and to verify if the newly introduced technical changes contributed to better results and influenced the incidence of complications. The changes introduced to the technique were dissection of the fasciocutaneous margin exceeding the cutaneous portion of the flap and preservation of a lane of skin over the pedicle.
We used fasciocutaneous and fasciosubcutaneous flaps with a distal pedicle and without restrictions regarding the use of tissue from the upper one-third of the leg for the flap. These surgeries were performed in 1 sitting.
Fisher's exact test was used for statistical analysis.
Surgical Technique
Surgeries began with wound debridement. Next, the size of wounds was measured to assess the required size of the flap and the distance between the rotation point (pivot; 5 cm above the lateral malleolus), and the wound was measured to determine the size of the pedicle. These measurements were transferred to the central axis of the posterior region of the leg; this process was aided by palpation of the space between the medial and lateral flesh areas of the gastrocnemius (Figure 1). We made an incision in the upper margin of the flap and dissected the subcutaneous area with shears in a beveled and ascending manner to prepare a fasciocutaneous margin larger than the piece of skin. The minor saphenous vein and the medial sural nerve were connected and sectioned (Figures 2 and 3). These structures were in the superfascial plane in dissections in the medial third of the leg and were in the subfascial plane in the upper third of the leg. If necessary, the flap was redesigned in order to maintain the structures in their middle axes. In these cases, dissection of the flap was continued only after maintenance of these structures. Dissection proceeded from the proximal to the distal region while ensuring that the deep fascia, medial sural nerve, and minor saphenous vein were included (Figure 4).

Figure 1 - Marking the graft. The rotation point is 5 cm above the lateral malleolus (the limit for dissection of the pedicle). The length of the pedicle is identical to the distance between the rotation point of the flap and the wound. The size of the flap is identical to the size of the wound.

Figure 2 - Beginning the flap dissection. The dissection begins in the upper margin, in a beveled and ascending manner, in order to generate a fasciosubcutaneous margin beside the cutaneous margin of the flap.
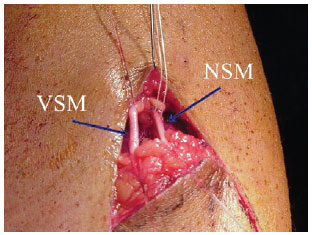
Figure 3 - Selection of the pedicle. All structures that should be in the flap must be identified. NSM = medial sural nerve (medial cutaneous nerve of the sura). VSM = medial minor saphenous vein of the nerve.
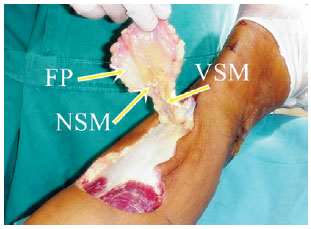
Figure 4 - Important structures for flap nutrition. The superfascial plexus, the medial superficial sural artery, which follows the nerve, and the arteries that follow the vein vascularize the flap and must always be a part of the flap and its pedicle. FP = Deep fascia. NSM = medial sural nerve. VSM = minor saphenous vein.
Herein, we highlight technical details such as maintaining at least 1 cm of the fasciosubcutaneous margin beside the cutaneous portion of the flap and maintaining a lane of skin of at least 1.5 cm width over the pedicle (Figure 5). When transposition was performed by folding the pedicle over itself (like a book sheet) or through a subcutaneous tunnel, it was necessary to remove the piece of the skin of the pedicle (Figures 6 and 7). Esmarch bandages and pneumatic tourniquets were used only in group 1 because we learned from experience that these were unnecessary.

Figure 5 - Modifications to the technique. Dissection of the fasciosubcutaneous margin surrounding the skin of the flap improves circulation and leaving a lane of skin over the pedicle prevents the requirement for a skin graft.

Figure 6 - The fasciosubcutaneous flap. A, in wounds in the heel or over the lower Achilles tendon, the best option is to generate a fasciosubcutaneous flap by folding it over its rotation point, like a book sheet. The fascial side, which is the side that receives the skin graft, should be facing upwards. In these cases, the skin of the flap and the pedicle should be removed. B, the flap after the skin graft.

Figure 7 - A flap transposed through a subcutaneous tunnel. The flap can be transposed through a subcutaneous tunnel to avoid a scar between the rotation point and the wound. However, this technique has a high risk of compression of the pedicle due to edema and vascular congestion in the flap. In these cases, the lane of skin is not left in the pedicle.
RESULTS
The surgery was satisfactory in 96.7% of the patients: 92.6% in group 1 and 100% in group 2.
In group 1, partial necrosis of the graft occurred in 5 (18.5%) cases. Reintervention was required in only 1 of these cases because the necrosis did not compromise the results in the other 4 cases. Total graft necrosis occurred in only 1 case (3.7%) in this group.
In group 2, we did not observe any cases of total loss of the graft but partial necrosis occurred in 3 (8.8%) cases, without the need for reintervention (Table 1).
In total, 52 fasciocutaneous and 9 fasciosubcutaneous graft surgeries were performed. The treated areas were the foot (17 cases: 10 in the heel and 7 in the dorsum) and the distal third of the leg (44 cases: 9 anterior, 21 anteromedial, 5 anterolateral, 6 medial, and 2 lateral).
DISCUSSION
The reverse flow sural graft was used in lesions localized in the distal region of the leg and the proximal region of the foot with bone exposure. These lesions were frequently accompanied by an exposed fracture or exposed tendons. Experience with this technique was accumulated over 10 years with 61 grafts.
The incidence of complications was quite acceptable when compared to the incidence that is generally observed in grafts. The results for the patients that underwent surgery in the last 5 years were better than the results of those who underwent surgery in the first 5 years. This was evidenced by a decrease in partial necrosis from 18.5% to 8.8% (p = 0.46), loss of the graft from 3.7% to null (p = 0.44), the general index of complications from 22.2% to 8.8% (p = 0.16), and need for reinterventions from 7.4% to null (p = 0.19). Therefore, this study suggests that the outcome tends to improve and the results are quite positive when surgeons have passed the learning phase and when the technique has been perfected. However, the more number of cases must be evaluated for these observations to be statistically significant.
We cannot state that the proposed alterations such as maintaining a fasciosubcutaneous margin that exceeds the skin flap and maintaining a lane of skin over the pedicle (group 2) are responsible for the improved results because the learning phase also influenced the results in group 1. However, these results reinforce the findings of previous studies, which show the importance of paying attention to technical details when preparing the flap 11,12 and avoiding the most common errors committed during the learning phase.
The most important details that should be addressed and the most frequent errors committed by surgeons who are in the process of learning this technique are mentioned below:
1. Failure to take all structures that should compose the graft at the beginning of the dissection.
The sural nerve is frequently not included in the dissection when surgeons perform this procedure before they are familiar with the anatomy of the region. Articles and books describe the location of the medial sural nerve in the same plane as, but lateral to, the minor saphenous vein1,2,5. However, dissection of the higher margin of the flap occurs in the proximal third of the leg, and the saphenous vein may be located superfascially and the nerve may be subfascial in this region11-13. Thus, the surgeon may inadvertently take only the saphenous vein and several nearby nerves, leaving the sural nerve out of the flap. The sural nerve is noticed when the dissection reaches the middle third of the leg, where the sural nerve crosses the dissection plane and moves from the subfascial to the superfascial plane. The sural nerve is hereby sectioned and taken with the flap and its pedicle, but a large part of the flap will not contain the medial superficial sural artery, which is the major source of nutrition. To avoid this, the surgeon must always search for the sural nerve between the 2 portions of the gastrocnemius, dissecting the areolar and fatty tissue where the nerve is located until the soleus muscle just below the gastrocnemius is located. This procedure ensures that the medial sural nerve will be included. Furthermore, the deep fascia, the minor saphenous vein, and the medial sural nerve must be included at the beginning of the dissection of the flap; the flap and the pedicle must be centralized around the nerve and the vein. If needed, the flap may be redrawn to be more lateral or medial and the pedicle should be progressively dissected up to its rotation point. The structures of the pedicle will progressively become more lateral in the distal region of the leg. These structures must be followed and they should always be maintained in a central position in the axis of the pedicle.
2. Compression of the pedicle
The delicate pedicle has a width of approximately 4 cm and is composed of deep fascia and subcutaneous tissue, with the medial sural nerve and the minor saphenous vein as its main structures. Therefore, the pedicle may easily become crushed or compressed after transposing the flap to the wound to be treated1,2,5-7,10.
The surgeon should observe the best direction of rotation, whether medial or lateral, to avoid compression. This is particularly important when the wound is located in the anterior region of the distal third of the leg or foot. The fasciosubcutaneous flap should be used for wounds located in the lower Achilles tendon or in the heel. In these cases, the flap should be rotated like a book sheet with the cutaneous graft placed on the fascial surface of the flap (Figure 6).
To avoid compression of the pedicle, the flap should not be transposed through a subcutaneous tunnel because the skin in this area is tight and local edema may compromise venous return through the pedicle. Therefore, many authors propose that an incision should be made between the rotation point of the flap and the wound to accommodate the pedicle, and that a skin graft should be placed over it (Figure 8). The suggestion to leave 1 lane of skin that is approximately 1.5 cm in width over the pedicle has several advantages: the pedicle is firmer and more protected, which helps to avoid compression, and a skin graft is not required over the pedicle, which enables this lane of skin to be sutured to the skin of the flap without oppressing it (Figure 9).

Figure 8 - Reverse flow sural flap in an island with the graft over the pedicle of the flap. This procedure was usually performed using the conventional technique.

Figure 9 - Lane of skin over the pedicle. The flap technique was modified so that a lane of skin was left over the pedicle. This made the area firm and protected, thus avoiding both compression and the requirement for a skin graft.
3. Lesion to the most distal part of the saphenous vein
In the distal third of the leg, the minor saphenous vein becomes quite superficial and is essentially right under the skin in thin people. For this reason, one must cautiously make an incision in the skin and dissecting the superficial side of the pedicle in this region.
4. Compression of the pedicle by the wound dressing
The dressing of the wound is the last part of the procedure. Allowing a person who lacks knowledge of the physiology of the flap to perform the dressing may result in a bad outcome if the dressing is placed too tightly on the pedicle, thereby causing compression.
5. Patient positioning that results in leaning on the flap or pedicle
Teaching the patients to position themselves correctly is important since lying on the posterior region of the leg may cause compression of the pedicle. A prone or side position is preferable to the supine position. If the supine position is necessary, pillows must be placed in the proximal part of the leg or knee and under the heel (if this is not the area of the graft) to avoid compression in the posterior region of the distal third of the leg at the point of rotation of the pedicle (Figure 10).

Figure 10 - Details that should be addressed when the patient is placed in the supine position. The patient must not lean on the flap or its pedicle. The best positions are prone or side. However, if the patient needs to lie in the supine position, a pillow should be placed over the heel and knee so the posterior area of the leg is suspended, without compression.
The advantages of the technical alterations introduced herein include the benefits of leaving a lane of skin under the pedicle, as described. Furthermore, the fasciosubcutaneous margin around the cutaneous part of the flap improves venous return in the extremities of the cutaneous portion of the flap, decreasing congestion or epidermolysis.
After the above-mentioned details were considered on a routine basis, the incidence of complications decreased 13.4%, the incidence of partial necrosis of the flap decreased 9.7%, total necrosis dropped 3.7%, and graft failure (in which it was necessary to perform another flap) dropped 7.4%. More cases are required for these results to be statistically significant.
Although several studies have described transferring the flap via interpolation14,15, which requires 2 surgeries, we did not use this technique because complications are not very frequent.
The flap maintains the common disadvantages of fasciocutaneous flaps: an unaesthetic scar in the donor area and hypoesthesia in the lateral region of the leg and foot. To improve the aesthetics of the scar in the donor area, we tried to limit the cutaneous portion of the flap to a width that allowed primary closure, extending the fasciocutaneous portion according to the requirements of the wound and subsequently placing a skin graft over it. The lack of patient complaints may be attributed to properly informing the patients about the sequelae caused by the flap. Although we did not receive requests for retouching the scar, this could be performed, if necessary.
CONCLUSIONS
The incidence of complications may be decreased by dissecting the fasciosubcutaneous margin, preserving a lane over the pedicle, and using a surgeon with experience.
The reverse flow sural flap is one of the few alternatives for covering important structures such as bone or tendons in the distal region of the leg, particularly when the institution does not have a capable microsurgery team. This flap is also an appropriate option at institutions that perform microsurgery because the surgery is simple and fast.
REFERENCES
1. Masquelet AC, Gilbert A. Atlas colorido de retalhos na reconstrução dos membros. Rio de Janeiro: Revinter; 1997. p. 160-6.
2. Nakajima H, Imanishi N, Fukuzumi S, Minabe T, Fukui Y, Miyasaka T, et al. Accompanying arteries of lesser saphenous vein and sural nerve: anatomic study and its clinical applications. Plast Reconstr Surg. 1999; 103(1):104-20.
3. Imanish N, Nakajima H, Fukuzumi S, Aiso S. Venous drainage of distally based lesser saphenous-sural veno-neuradipofascial pedicled fasciocutaneous flap: a radiographic perfusion study. Plast Reconstr Surg. 1999;103(2):494-8.
4. Akhtar S, Hameed A. Versatility of the sural fasciocutaneous flap in the coverage of lower third leg and hind foot defects. J Plast Reconstr Aesthet Surg. 2006;59(8):839-45.
5. Almeida MF, Costa PR, Okawa RY. Reverse-flow island sural flap. Plast Reconstr Surg. 2002;109(2):583-91.
6. Baumeister SP, Spierer R, Erdmann D, Sweis R, Levin LS, Germann GK. A realistic complication analysis of 70 sural artery flaps in a multimorbid patient group. Plast Reconstr Surg. 2003;112(1):129-40.
7. Belém LFMM, Lima JCSA, Ferreira FPM, Ferreira EM, Penna FV, Alves MB. Retalho sural de fluxo reverso em ilha. Rev Soc Bras Cir Plást. 2007;22(4):195-201.
8. Cheema TA, Saleh ES, Carvalho AF. The distally based sural artery flap for ankle and foot coverage. J Foot Ankle Surg. 2007;46(1):40-7.
9. El-Shazly M, Yassin O. Increasing the success rate of the reversed-flow fasciocutaneous island sural flap: a clinical experience in 26 cases. Ann Plast Surg. 2006;57(6):653-7.
10. Touam C, Rostoucher P, Bhatia A, Oberlin C. Comparative study of two series of distally based fasciocutaneous flaps for coverage of the lower one-fourth of the leg, the ankle, and the foot. Plast Reconstr Surg. 2001;107(2):383-92.
11. Vendramin FS. Estudo prospectivo do retalho sural de fluxo reverso na reconstrução do pé e da região distal da perna [dissertação de mestrado]. Rio de Janeiro: Universidade Federal do Rio de Janeiro, Faculdade de Medicina; 2004. 152p.
12. Vendramin FS, Cláudio-da-Silva CS. Retalho sural estendido de pedículo distal. Rev Col Bras Cir. 2004;31(4):248-52.
13. Ayyappan T, Chadha A. Super sural neurofasciocutaneous flaps in acute traumatic heel reconstructions. Plast Reconstr Surg. 2002;109(7):2307-13.
14. Garcia AMC. Retalho sural reverso para reconstrução distal da perna, tornozelo, calcanhar e do pé. Rev Bras Cir Plást. 2009;24(1):96-103.
15. Maffi TR, Knoetgen J 3rd, Turner NS, Moran SL. Enhanced survival using the distally based sural artery interpolation flap. Ann Plast Surg. 2005;54(3):302-5.
Master and Doctor at the Universidade Federal do Rio de Janeiro (Federal University of Rio de Janeiro) -UFRJ, Rio de Janeiro, RJ, Brazil; professor of Surgical Technique at the Universidade Federal do Pará (Federal University of Pará) -UFPA, supervisor of the Service of Plastic Surgery at the Hospital Metropolitano de Urgência e Emergência (Metropolitan Hospital of Urgency and Emergency), full member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery), Belém, PA, Brazil.
Correspondence to:
Fabiel S. Vendramin
Av. Generalíssimo Deodoro, 391 - Umarizal
Belém, PA, Brazil - CEP 66035-140
E-mail: fabiel@doctor.com
Study conducted at the Hospital Metropolitano de Urgência e Emergência (Metropolitan Hospital of Urgency and Emergency), Belém, PA, Brazil; Hospital Universitário Clementino Fraga Filho (University Hospital Clementino Fraga Filho), Rio de Janeiro, RJ, Brazil; e Hospital Central da Polícia Militar do Estado do Rio de Janeiro (Central Hospital of the Military Police of Rio de Janeiro), Rio de Janeiro, RJ, Brazil.
Article submitted to SGP (Sistema de Gestão de Publicações/ Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: March 2nd, 2012
Article accepted: May 6, 2012


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter