

Original Article - Year 2012 - Volume 27 -
Pain assessment in patients undergoing cosmetic or reconstructive plastic surgery
Avaliação do nível de dor em pacientes submetidos a cirurgias plásticas estéticas ou reparadoras
ABSTRACT
BACKGROUND: Quantifying aesthetic and reconstructive plastic surgery and assessing postoperative pain caused by these procedures would aid the creation of protocols to humanize nursing care for hospitalized patients, thus possibly making professionals who interact with such patients on a daily basis more compassionate. This study assessed the levels of pain in patients who underwent reconstructive or aesthetic plastic surgery.
METHODS: The medical records of 200 patients operated at São Rafael Hospital were reviewed. The reasons for undergoing surgery and pain due to the procedure were also evaluated.
RESULTS: The number of patients who reported strong or severe pain following the procedure was significantly lower; all patients who reported strong or severe pain following the procedure had undergone liposuction with or without breast prosthesis.
CONCLUSIONS: Pre-, intra-, and postoperative protocols regarding liposuction should be reassessed in order to decrease the severe pain reported by patients undergoing this procedure.
Keywords: Plastic surgery. Pain. Pain measurement.
RESUMO
INTRODUÇÃO: Estudos que quantificassem as cirurgias plásticas estéticas e reparadoras e avaliassem a dor pós-cirúrgica decorrente de tais procedimentos permitiriam a criação de protocolos de humanização do atendimento a esses pacientes, possivelmente sensibilizando os profissionais que com eles convivem diariamente. O objetivo deste estudo é avaliar o nível de dor em pacientes submetidos a cirurgias plásticas estéticas ou reparadoras.
MÉTODO: Avaliação de 200 prontuários de pacientes operados no Hospital São Rafael (São Paulo, SP, Brasil), observando motivo de realização da cirurgia e quadro de dor.
RESULTADOS: O número de pacientes que relatou dor forte ou intensa foi bastante reduzido. Dentre esses pacientes, todos foram submetidos a lipoaspiração, associada ou não à colocação de prótese de mama.
CONCLUSÕES: Os protocolos pré, intra e pós-cirúrgicos relacionados aos procedimentos de lipoaspiração devem ser reavaliados, visando à redução da forte dor relatada pelos pacientes submetidos a esse tipo de procedimento.
Palavras-chave: Cirurgia plástica. Dor. Medição da dor.
Trauma, injury, and surgical pathology have always existed. In particular, the number of wartime injuries has increased considerably due the constant development of arms used for large-scale assaults1.
The medical techniques recommended for the treatment of deformities, trauma, and internal and external diseases, which are performed with the help of manual invasive and instrumental procedures, are called as operations or surgical intervention2-5. Cooperation between surgeons, anesthesiologists, and nurses among others is necessary to perform surgical interventions. Moreover, specialized materials and instruments are used for diagnostic purposes, elective treatment, symptomatic relief, organic reconstruction, and to cure patients6.
Plastic surgery includes surgical procedures aiming to improve patients' self-esteem and self-image. Plastic surgery aims to restore body form and function, thus not only improving aesthetics, but also quality of life. In addition, plastic surgery repairs and corrects abnormalities, striving to reach cultural norms of standard appearance or beauty7,8. Most plastic surgeries are clean surgeries or possibly contaminated procedures. This categorization is derived from the standard classification of surgical wounds and depends on the different measures that may or may not have been taken to prevent infection pre-, intra-, and postoperatively. Among these procedures, adequate antisepsis and asepsis, surgical skills, surgical time, and correct tissue handling should be highlighted9. Besides improving the physical appearance of patient, plastic surgery also directly affects psychological aspects related to self-perception. Thus, plastic surgeons not only create physical changes in their patients, but psychological changes as well10,11.
Plastic surgery is divided in 2 main branches: aesthetic and reconstructive. Reconstructive plastic surgery involves restoring the function and/or appearance of body parts affected by trauma, disease, congenital anomalies, or deformities. By improving the function of these structures, the patient feels closer to what he/she considers normal - a concept directly related to health and disease8,12. On the other hand, aesthetic plastic surgery aims to correct imperfections, alter specific regions of the body, and reshape theoretically normal structures. However, its main aims are to improve physical appearance, enhance beauty, and repair bothersome marks that are not considered diseases but psychologically affect the individual, such as anatomical changes associated with aging or pregnancy. Moreover, exceptionally large or small organs such as the breasts can be altered to meet the standards of beauty of the patient10,12,13. It should be emphasized that both patients and healthcare professionals can consider any surgical procedure stressful. Therefore, humanized nursing care protocols in the preoperative period can improve the quality of the services offered to patients14.
Pain is an unpleasant sensory and emotional experience associated with tissue injury. The characteristics of pain differ among individuals. The following characteristics of pain should be evaluated: pain onset, location, irradiation, type of pain, duration, and pain-related behavioral responses (e.g., facial expression, restlessness, anxiety, insomnia, irritability, and pallor)15.
Pain tends to be frequent in the postoperative period. Its intensity is influenced by physiological factors such as the extent of trauma during the procedure, the surgeon's technical skills, prior disease, the location and type of incision, and psychological and cultural factors. Unsatisfactory pain relief after surgery is mostly due to a lack of knowledge about pain assessment16-18.
Pain can be measured on a uni-or multi-dimensional scale. The scales commonly used to evaluate pain in surgical procedures are one-dimensional, in which only the dimension of pain is evaluated. The most commonly used scales are visual numerical scales, scored from 0 to 10, where 0 means the absence of pain and 10 the worst imaginable pain. In addition, the visual analog scale, which enables a continuous analysis of pain, consists of a straight unnumbered line indicating the absence of pain and worst imaginable pain at either end of the scale. Lastly, in scales of verbal and visual categories, patients describe their pain using a facial pain scale by selecting drawn faces that match the intensity of their pain15-17.
Although rare in the literature, surveys regarding the number of surgeries performed for purely aesthetic purposes or recommended for the correction of late post-traumatic conditions are important for elucidating and understanding the profiles of the patients. Research assessing post-surgical pain in patients undergoing different plastic surgery procedures for aesthetic or reconstructive purposes is still scarce in the literature. Such data would allow hospitals and clinics to create models and protocols to humanize nursing care for hospitalized patients in addition to increasing the sensitivity of the professionals who interact with them on a daily basis.
Therefore, in this study, we quantified the numbers of plastic surgeries performed for aesthetic and reconstructive purposes, and assessed the levels of pain in patients undergoing these surgeries. These data will allow the development of nursing care protocols specifically designed for individual patients.
METHOD
This is a descriptive prospective study based on a quantitative approach conducted from December 2010 to December 2011. The cohort of this study consisted of patients who underwent plastic surgery for either aesthetic purposes or the correction of late post-traumatic conditions during the study period, at São Rafael Hospital.
Patients under 18 years old were excluded.
The patients' medical records were evaluated, including the type of surgery, average surgery duration, hospitalization time, gender, age, occupation, marital status, reasons for performing the surgery, and occurrence of possible pre-, intra-, and postoperative complications.
The grade of pain was mapped on scales of visual and verbal categories, in which the patients described their pain by means of drawn faces. The scores of this scale for pain assessment were as follows: 0, no pain; 2, mild pain; 4, moderate pain; 6, strong pain; 8, severe pain; and 10, unbearable pain.
Finally, weight and height were measured to calculate body mass index (BMI) using the following formula: BMI = weight/height2. BMI values were classified as follows: <18.5, underweight; 18.5-24.9, normal weight; 25-29.9, overweight; 30-34.9, obesity grade I; 35-39.9, obesity grade II; and >40, obesity grade III.
The data obtained were entered into worksheets and evaluated considering the cohort as a whole.
Patient age is expressed as mean ± standard deviation. All other variables are expressed as absolute values and relative percentages. No specific statistical tests were applied.
This study is registered at the National Council of Ethics in Research (CONEP; #453544/2011) and approved by the Ethics and Research Committee of the institution in which it was performed.
RESULTS
This study included 200 patients: 5 (2.5%) males and 195 (97.5%) females with an average age of 33 ± 11 years. Regarding the marital status, 17 (8.5%) patients were divorced, 83 (41.5%) married, and 100 (50%) single.
Regarding the surgery performed, 50 (25%) patients underwent liposuction, 35 (17.5%) dermolipectomy, and 57 (28.5%) breast prosthesis implantation. Evaluation of combined surgeries revealed that 51 (25.5%) patients underwent liposuction associated with breast prosthesis implantation and 5 (2.5%) dermolipectomy combined with liposuction. Only 2 (1%) patients underwent simultaneous dermolipectomy, liposuction, and breast prosthesis implantation.
Regarding BMI, 7 (3.5%), 126 (63%), 50 (25%), 16 (8%), and 1 (0.5%) patients were classified as underweight, normal weight, overweight, obesity grade I, and obesity grade II, respectively.
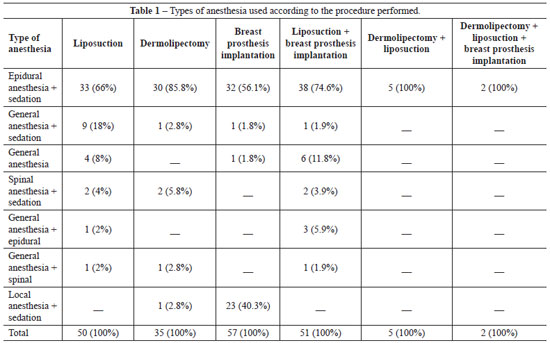
Table 1 shows the type of anesthesia used with respect to the procedure performed.
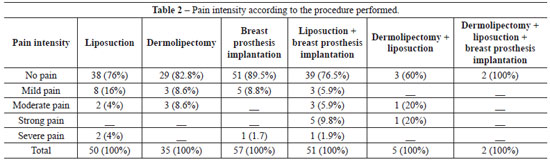
The intensity of pain according to the experimental procedure is presented in Table 2.
DISCUSSION
The effects of aesthetic plastic surgery are not limited to the physical appearance of the individual; psychological aspects linked to body self-image, which are related to the standards of beauty of the individual's culture, are also affected7,8.
In this study, most of the patients underwent breast prosthesis implantation. The most common types of anesthesia used for this procedure were local combined with sedation and epidural combined with sedation. The present results are consistent with the data published by Fachinelli and Fachinelli19, who conducted a similar survey in Caxias do Sul (RS, Brazil); they emphasize that medical anesthetists prefer the type of anesthesia mentioned above, which is considered safe with fewer side effects. Although fewer men undergo plastic surgery than women at present, Castro20 found a clear increasing demand by men, mainly for aesthetic purposes. This indicates that it is necessary to reformulate care protocols to better match the requirements of the male population.
It is interesting to note that more than half of the patients evaluated in this study had a BMI within the normal range. These findings are corroborated by those of Martinez et al.21, who found that the main reason people seek plastic surgery is to obtain a body that is as close as possible to the standard of beauty. This indicates that, at present, more aesthetic surgeries are performed than reconstructive surgeries.
The present data regarding liposuction, in which patients were anesthetized with epidural anesthesia combined with sedation, are similar to those published by Martins et al.22; based on a survey conducted in Tubarão (SC, Brazil), the authors recommend this type of anesthesia for liposuction because of its relatively few side effects and safety. André23 reports that in abdominoplasty procedures, the most appropriate anesthesia is epidural, which is supported by the present results.
Approximately one-fifth of the patients in this study reported pain. Among them, the vast majority underwent liposuction combined or not with breast prosthesis implantation. Silva and Moraes24 report a similar proportion in a survey conducted in São Paulo (SP, Brazil). In their study, liposuction was the procedure mostly strongly associated with postoperative pain. These findings highlight the necessity for reassessing all operative phases associated with this procedure; this might involve the improvement of anesthetic and surgical techniques as well as nursing procedures in order to maintain the wellbeing and comfort of patients and lower their levels of pain. However, it is noteworthy that few patients reported strong or severe pain; patients who underwent liposuction more than once, combined or not with breast prosthesis implantation, reported the highest levels of pain. The fact that only patients undergoing breast prosthesis implantation did not complain of pain indicates that it is necessary to focus more on liposuction in order to reduce the discomfort and suffering of those patients. According to Pimentel25, the highest levels of pain reported by patients who underwent liposuction are due to the use of drains. This can be avoided easily by administering analgesics during hospitalization. In that study25, no complaints of pain were reported after drain removal, emphasizing the importance of analgesia. Patients reported local pain only in the sectioned area when it was compressed.
Finally, it is extremely important to re-emphasize that considerably more surgeries are performed for aesthetic purposes than for reconstructive purposes. The present data, which are similar to those of Barros26 and Castro20, also highlight the fact that the demand for cosmetic surgery is increasing continually, justifying the continuous improvement and training of all staff involved.
The limitations of this study include the small cohort, low number of variables, and short follow-up period. Therefore, additional multicenter and controlled studies that include more patients and longer follow-up periods are required to confirm the findings of the present study.
CONCLUSIONS
Most patients undergoing cosmetic surgery do not report pain during the immediate postoperative period. However, the vast majority of patients undergoing liposuction, combined with other surgical procedures or not, report pain after surgery, including severe pain. Thus, anesthetic, surgical, and nursing procedures should be improved to maintain the wellbeing and comfort of patients and reduce pain levels.
REFERENCES
1. Martire Júnior L. Alcance atual da cirurgia plástica. Rio de Janeiro: Astúrias; 2005.
2. Marques RG. Cirurgia: arte e ciência. Rev Col Bras Cir. 2008;35(4):214-5.
3. Rezende JM. Cirurgia e patologia. Acta Cir Bras. 2005;20(5):346.
4. Leal VCLV, Catrib AMF, Amorim RF, Montagner MA. O corpo, a cirurgia estética e a saúde coletiva: um estudo de caso. Ciênc Saúde Coletiva. 2010;15(1):77-86.
5. Goldenberg S. Cirurgia como sinônimo de operação. Acta Cir Bras. 2001;16(4):275.
6. Cavalcante JB, Pagliuca LMF, Almeida PC. Cancelamento de cirurgias programadas em um hospital-escola: um estudo exploratório. Rev Latinoam Enferm. 2000;8(4):59-65.
7. Ferreira LM, Schor N. Guia de cirurgia plástica. Barueri: Manole; 2007.
8. Mélega JM. Cirurgia plástica: fundamentos e arte: princípios gerais. Rio de Janeiro: Guanabara Koogan; 2009.
9. Franco D, Cardoso FLL, Franco T. Uso de antibióticos em cirurgia plástica. Rev Soc Bras Cir Plást. 2006;21(2):112-5.
10. Ferreira MC. Cirurgia plástica estética: avaliação dos resultados. Rev Soc Bras Cir Plást. 2000;15(1):55-66.
11. Dini GM, Quaresma MR, Ferreira LM. Adaptação cultural e validação da versão brasileira da escala de auto-estima de Rosenberg. Rev Soc Bras Cir Plást. 2004;19(1):41-52.
12. Medeiros MSF. Imagens, percepções e significados do corpo nas classes populares. Soc Estado. 2004;19(2):409-39.
13. Auricchio AM, Massarollo MCKB. Procedimentos estéticos: percepção do cliente quanto ao esclarecimento para a tomada de decisão. Rev Esc Enferm USP. 2007;41(1):13-20.
14. Galvão MC, Sawada NO, Rossi LA. A prática baseada em evidências: considerações teóricas para sua implementação na enfermagem perioperatória. Rev Latinoam Enferm. 2002;10(5):690-5.
15. Pedroso RA, Celich KLS. Dor: quinto sinal vital, um desafio para o cuidar em enfermagem. Texto Contexto Enferm. 2006;15(2):270-6.
16. Pereira LV, Sousa FAEF. Estimação em categorias dos descritores da dor pós-operatória. Rev Latinoam Enferm. 1998;6(4):41-8.
17. Scopel E, Alencar M, Cruz RM. Medidas de avaliação de dor. Rev Digital. 2007. Disponível em: http://www.efdeportes.com/efd105/medidas-de-avaliacao-da-dor.htm Acesso em 28/2/2012.
18. Pereira LV, Sousa FAEF. Mensuração e avaliação da dor pós-operatória: uma breve revisão. Rev Latinoam Enferm. 1998;6(3):77-84.
19. Fachinelli A, Fachinelli FA. Anestesia local em mamoplastia de aumento. ACM Arq Catarin Med. 2007;36(Supl.1):20-2.
20. Castro AL. Saúde e estética: a medicalização da beleza. Rev Eletr Com Inf Inov Saúde. 2011;5(4):14-23.
21. Martinez MAR, Okajima RMO, Proto RS, Lourenço LM, Machado Filho CDS. Estudo de 543 pacientes submetidos à lipoaspiração tumescente. Surg Cosmet Dermatol. 2010;2(3):155-8.
22. Martins EA, Miranda LFD, Sakae TM, Valle LFC, Ely JB. Avaliação de uma série de 38 casos de pacientes submetidos à cirurgia de lipoaspiração em Tubarão - SC entre outubro de 2004 e fevereiro de 2005. ACM Arq Catarin Med. 2007;36(1):113-8.
23. André FS. Abdominoplastia e lifting do púbis. Rev Bras Cir Plást. 2009;24(3):345-50.
24. Silva AP, Moraes MW. Incidência de dor no pós-operatório de cirurgia plástica estética. Rev Dor. 2010;11(2):136-9.
25. Pimentel LAS. Hidrolipoaspiração: 22 anos de experiência com lipoplastia intumescente. Rev Soc Bras Cir Plást. 2004;19(1):53-74.
26. Barros RR. Cirurgia plástica na adolescência. Adolesc Saude. 2007;4(1):45-7.
1. Technical Nurse at Hospital São Rafael (São Rafael Hospital), student of Nurse Graduation Course at the Universidade Nove de Julho (Nove de Julho
University - UNINOVE), São Paulo, SP, Brazil.
2. Doctorate and master degree in Public Health from Universidade de São Paulo (São Paulo University), Professor at the Health Department of the
UNINOVE, São Paulo, SP, Brazil.
3. Master in Pharmacology from Universidade Federal de São Paulo (Federal University of Sao Paulo - UNIFESP), Professor at the Health Department of
the UNINOVE, São Paulo, SP, Brazil.
4. Doctorate and master degree in Sciences from UNIFESP, Professor at the Health Department of the UNINOVE, São Paulo, SP, Brazil.
Correspondence to:
Renato Ribeiro Nogueira Ferraz
Av. Pedro Mendes, 872 - Selecta
São Bernardo do Campo, SP, Brazil - CEP 09791-530
E-mail: renato@nefro.epm.br
Article submitted to SGP (Sistema de Gestão de Publicações/ Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: March 2, 2012
Article accepted: May 13, 2012
This study was performed at the Universidade Nove de Julho (Nove de Julho University - UNINOVE) and Hospital São Rafael (São Rafael Hospital), São Paulo, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter