

Original Article - Year 2012 - Volume 27 -
Reconstruction of large scalp and forehead defects following tumor resection: personal strategy and experience - analysis of 25 cases
Reconstrução de grandes defeitos de couro cabeludo e fronte em oncologia: tática pessoal e experiência - análise de 25 casos
ABSTRACT
BACKGROUND: The anatomical peculiarities of extensive malignant neoplasms of the scalp and forehead remain a challenge for plastic surgeons. Although several procedures for repair of these defects have been described, the ideal reconstruction relies on careful assessment of each clinical case and aims to achieve the best functional and aesthetic outcome with minimal morbidity of the donor area. The aim of this study is to evaluate a series of patients who underwent immediate reconstruction following scalp and forehead tumor resection, in order to demonstrate the personal technique and experience of the author.
METHODS: This is a retrospective analysis of 25 patients who underwent scalp and forehead reconstruction between June 2009 and June 2011 following treatment for advanced skin cancer. The following parameters were studied: gender, age, diagnosis, clinical staging, location and size of the defect, repair strategy, complications, and current clinical status.
RESULTS: Of the 25 patients, 60% were men; the average age was 64.8 years. Patients most frequently presented in clinical stage III (88%). Squamous cell carcinoma was the most common tumor (84%) and the biparietal region was the most commonly affected area (20%). The size of the defects varied from 3.8 cm × 3.5 cm to 22.9 cm × 15 cm. The reconstructive procedure used most often (80%) relies on the production of a local flap. Two (8%) cases of partial flap necrosis and 1 case (4%) of partial graft loss were noted. All patients are still alive and only one shows signs of proliferative malignant neoplasm (tumor recurrence without treatment options). With regard to functional and aesthetic aspects, both the author and the patients considered the results obtained to be satisfactory.
CONCLUSIONS: In the literature, a variety of procedures for scalp reconstruction have already been described. In patients with extensive loss of soft tissues, microsurgical flaps are the most commonly used option. Reconstruction with a local advancement flap is a safe technique, provides satisfactory results, and is performed with a simple technical procedure. It therefore may be ideal for borderline-operable patients.
Keywords: Surgical flaps. Plastic surgery. Scalp/surgery. Head and neck neoplasms. Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: Neoplasias malignas extensas em couro cabeludo e fronte tornam-se um desafio para o cirurgião plástico, em decorrência das particularidades anatômicas da região. Apesar da existência de muitas técnicas para o reparo dos defeitos, a reconstrução ideal depende da avaliação criteriosa de cada caso clínico e tem por finalidade alcançar o melhor resultado, tanto funcional como estético, com mínima morbidade no sítio doador. O objetivo deste estudo é avaliar uma série de pacientes submetidos a reconstrução imediata após ressecção oncológica em couro cabeludo e fronte, demonstrando tática pessoal e experiência do autor.
MÉTODO: Trata-se de análise retrospectiva de 25 pacientes operados no período de junho de 2009 a junho de 2011, submetidos a reconstrução de couro cabeludo e da fronte após tratamento de câncer de pele avançado dessa região. Foram estudados os seguintes parâmetros: sexo, idade, diagnóstico, estadiamento clínico, localização e dimensão do defeito, tática de reparo, complicações e estado clínico atual.
RESULTADOS: Amostra composta de 25 pacientes, sendo 60% homens, com média de idade de 64,8 anos. O estádio clínico III foi o mais frequente (88%), o diagnóstico de maior incidência foi o de carcinoma espinocelular (84%) e a região biparietal foi a localização mais atingida (20%). O tamanho dos defeitos variou de 3,8 cm x 3,5 cm a 22,9 cm x 15 cm. A técnica de reparo mais utilizada (80%) foi a confecção de retalho local. Ocorreram 2 (8%) casos de necrose parcial do retalho e 1 (4%) caso de perda parcial do enxerto. Todos os pacientes estão vivos, dos quais apenas um apresenta sinais de neoplasia maligna em atividade (recidiva tumoral e fora de possibilidade terapêutica). Quanto aos aspectos funcional e estético, tanto o autor como os pacientes consideram o resultado bom.
CONCLUSÕES: Na literatura internacional, são descritas várias técnicas de reconstrução do couro cabeludo. Na maioria dos casos com grande perda de tecidos moles, os retalhos microcirúrgicos são as opções mais aceitas. A reconstrução com retalhos locais de avanço constitui opção bastante segura e apresenta resultados favoráveis, com realização técnica mais simples e taticamente ideal para aqueles casos limítrofes de operabilidade.
Palavras-chave: Retalhos cirúrgicos. Cirurgia plástica. Couro cabeludo/cirurgia. Neoplasias de cabeça e pescoço. Procedimentos cirúrgicos reconstrutivos.
Reconstructive plastic surgery of the cephalic segment deals continually with defects of variable size and location. Therefore, several techniques with different degrees of complexity might be applied to a given defect. Grafts or local flaps efficiently repair minor defects that do not involve exposure of vital structures. However, extensive losses following tumor resections and involving the exposure of anatomical structures such as muscles, bones, dura mater, and blood vessels require a more complex coverage, which may be performed with local or distant flaps1.
The advent of microsurgery unequivocally improved reconstructive plastic surgery. Multiple surgical procedures involving rotation of neighboring, pedicled, or random flaps - always time consuming and expensive - were replaced by reconstruction in a single surgical procedure involving the transfer of multiple tissues.
The repair of large defects, which usually involves the scalp and occurs after tumor resection, remains a surgical and aesthetic challenge. These reconstructions aim to achieve the best functional result, ensuring the protection of the central nervous system, as well as a good aesthetic outcome, with minimal donor site morbidity.
Knowledge of the anatomy of the scalp and skull is essential to understand the pathophysiology of lesions in this region and to plan their reconstruction. Moreover, factors such as the efficiency of tumor resection and its extent might contribute to the final aesthetic result and influence the quality of life of the patient. Adjuvant radiotherapy can also influence the outcome of the surgery. Alteration in wound healing, shrinkage, fibrosis, prolonged swelling, hyperpigmentation, and radiodermatitis are the side effects most commonly observed after radiotherapy.
However, few studies on this subject take into account the patients' quality of life. Psychological and social well-being should be considered. Therefore, it is essential in oncologic, and particularly, in plastic surgery to study the quality of life of patients whose survival improved following the indicated cancer treatment, as adding "years to life" does not necessarily mean adding "life to years". In plastic surgery, several advantages are provided by an immediate reconstruction, which ensures better results when compared to a single tumor resection performed without reconstructive planning.
Advanced tumors of the head and neck are a serious problem if we consider the precarious conditions of the Unified Health System as well as the socioeconomic situation of the Brazilian population. Most of these tumors are derived from the skin and are mainly occur because of a combination of tropical climate and ethnic variability of the Brazilian population.
Anatomical Aspects of Scalp and Forehead
The brain is protected by defined and distinct anatomical structures that can be divided into soft tissues, which include the scalp (hairy area) and forehead (glabrous area) with their respective layers, and the bony tissues, that is, the cranial vault. Soft tissues are responsible for covering and protecting bony structures and are divided into 5 distinct anatomical layers: skin, subcutaneous tissue, galea aponeurotica, loose areolar tissue, and pericranium2.
The forehead is the anterior region of the vertebrate skull and extends, in man, from the hair bulb to the eyebrow.
The skin is formed by the epidermis, dermis, and skin appendages such as hair follicles and sebaceous glands, similar to other body areas. The scalp is characterized by the highest presence of hair follicles and by increased dermis thickness compared to other parts of the body.
The subcutaneous tissue is formed by dense connective tissue and fat, and links the skin to the deepest layer, that is, the galea aponeurotica. This layer is composed of several fibrous septa that form inelastic structures. These divide the subcutaneous tissue into compartments, whose anatomic peculiarity allows localization of infections to specific regions, thus avoiding their dissemination in the scalp and central nervous system. The main arteries and veins responsible for irrigation and venous drainage of the scalp are located in this layer. A complex anastomotic network maintains the connection between the main vascular pedicles. Among the most important vessels, we can highlight the superficial temporal, supraorbital, supratrochlear, posterior auricular, and occipital arteries3. This network allows for safe use of multiple vascular flaps. In the temporal region, the superficial temporal artery and vein are the main vessels and have the largest vascular pedicle caliber of vessels in the scalp. The superficial temporal artery is a branch of the external carotid artery. It is located more superficially at the site of the tragus, emerging from the parotid gland and above the zygomatic arch. Its 2 main branches are the frontal (anterior) and parietal (posterior) arteries. In the anterior region, the supraorbital and supratrochlear vessels cross the frontalis muscle at the site of the eyebrow and then run more superficially. The occipital vessels cross the region of the base of the skull below the occipital muscle and reach the subcutaneous layer near the superior nuchal line region, to then split into medial and lateral branches. The galea aponeurotica is formed by fibrous tissue and connects 2 major muscles: the frontalis muscle, located in the anterior region, and the occipital muscle, in the posterior region. In the posterolateral region, the galea aponeurotica is connected to the auricular muscles, whereas in the inferior region it connects to the superficial muscular aponeurotic system of the face. The superficial temporal fascia is next to the temporal region, above the temporal muscle. This area appears as a layer of dense connective tissue; it is highly vascularized and is different from the aponeurotic structure in the parietal regions.
The loose areolar tissue or subaponeurotic tissue is between the galea and pericranium. The structural characteristics of this layer confer mobility to the scalp and present an easy plane for dissection that facilitates surgical access and elevation of the flaps. In this layer, small arteries supplying the pericranium and small emissary veins connecting the intracranial venous sinus with the superficial venous system can be observed.
The pericranium covers the bony structure of the skull and is formed by a layer of highly vascularized cells. During the neonatal period, the fontanelles are protected only by the external layer of cells previously described.
The skull is formed by the frontal, parietal, temporal, and occipital bones, which together protect the brain. The skull is composed of 3 different bone layers, which are essential to its protective capability; they are the outer table, the diploe, and the inner table, which, depending on the area, show distinct thickness and conformation. This may necessitate modification of the surgical procedure according to the location of the defect. The outer table is formed by compact and dense bone and is in direct contact with the pericranium. The diploe, located between the outer and inner tables, has a cancellous bone structure, whereas the inner table is formed by compact bone and is in direct contact with the brain through its outermost meningeal layer, the dura mater3.
This study aims to evaluate a series of patients who underwent immediate reconstruction following scalp and forehead tumor resection. Moreover, the purpose of this study is to provide details of the procedure, with special focus on the strategy used for each patient; that is, the resources and the personal technique employed to achieve a positive outcome. Finally, this study aims to promote plastic surgery as part of the overall treatment of cancer, thus demonstrating its importance during rehabilitation. Multidisciplinary approaches, preoperative strategies, individualization, and appropriate indications for each procedure are essential for the success of reconstructive surgery and to obtain satisfactory results.
METHOD
This is a retrospective analysis of 25 patients operated upon between June 2009 and June 2011, who underwent scalp and forehead reconstruction following treatment of advanced skin cancer in this region. All reconstructions were immediate and followed rules for cancer surgery; that is, detecting free margins by frozen section.
The criteria for inclusion in the study were: patients with scalp defect caused by tumor resection, patient consent for the reconstruction procedure after having obtained clarification regarding the therapeutic strategy, and satisfactory clinical condition for surgery as determined by a clinical and laboratory evaluation of the surgical risk.
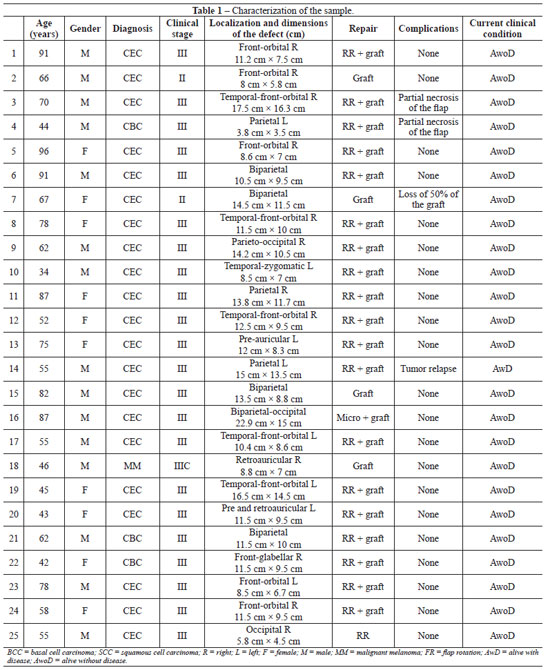
The following parameters were studied: age, gender, diagnosis, cancer stage according to pretreatment clinical classification, location and size of the defect, reconstruction procedure employed, complications, and current status (Table 1).
RESULTS
A cohort of 25 patients, 15 (60%) men and 10 (40%) women, with an average age of 64.8 years (range 34-96 years), was analyzed.
A histopathologic diagnosis of squamous cell carcinoma was most common, with 21 cases (84%), followed by basal cell carcinoma with 3 cases (12%) and malignant melanoma with 1 case (4%). Clinical stage III was the most frequent (88%).
In this series, the most common areas affected by the tumors, in descending order, were biparietal (n = 5), temporo-fronto-orbital (n = 5) and fronto-orbital (n = 5), followed by the parietal (n = 3), temporal (n = 2), retroauricular (n = 2), fronto-glabellar (n = 1), parieto-occipital (n = 1), and occipital (n = 1) regions.
The size of the defects ranged from 3.8 cm × 3.5 cm to 22.9 cm × 15 cm. The most frequently used reconstruction procedures included production of local flaps (n = 20; 80%), partial skin graft (n = 4; 16%), and microsurgical flaps (n = 1; 4%). The flap was chosen according to the need for coverage in each patient, taking into account the tumor resection (extent, location, and etiology of the defect), the possibility of tissue reconstruction, and the operability of each patient.
The microsurgical reconstruction used a latissimus dorsi myocutaneous flap with end-to-end facial vessel anastomosis. It was necessary to maintain the patient in the fasting state in the immediate postoperative period for a possible flap reexploration; antiplatelet therapy (aspirin, 100 mg/day) was continued for 3 weeks.
The follow-up for flap reconstruction was based on clinical monitoring of color, temperature, and bleeding of the flap assessed every 3 hours during the first 72 postoperative hours by members of the surgical team in alternation. These parameters were then evaluated daily until the patient was discharged.
Possible complications were divided into immediate (intraoperative), early (to 21 days postoperative), and late (after 21 days). No immediate complications were observed. Among early complications, we found 2 cases (8%) of partial flap necrosis and 1 (4%) of partial skin graft loss, both of which were treated with débridement and skin graft. One (4%) patient presented with late complications and exhibited tumor recurrence.
It is worth to mention that no complications such as hematomas, cerebrospinal fluid fistulas, infection, and - especially considering the microsurgical transplant - thrombosis, or indications for microsurgical reexploration were detected.
All the patients were alive at the end of the study period.
Patients and authors considered the aesthetic and functional results achieved to be satisfactory, taking into account the full coverage of the initial defect. As a disadvantage, a large increase of the glabrous area (the donor area for local neighboring flaps subjected to skin grafting) was observed.
Twenty-four (96%) patients are alive and disease-free to date, whereas 1 (4%) patient developed tumor recurrence and is currently under palliative care.
Figures 1 to 9 illustrate patients of this cohort; they were randomly selected from photographic archives and are identified as patients 3, 7, 11, 14, 16, 19, 21, 24, and 25.

Figure 1 - Case 3. In A, squamous cell carcinoma in the right fronto-orbital region. In B, defects due to tumor resection. In C, tissue obtained by monoblock resection. In D, production of scalp flap based on superficial temporal and retroauricular vessels. In E, immediate postoperative period, showing the reconstructed area and skin graft in the donor region of the flap. In F, late postoperative appearance, profile view. In G, late postoperative appearance, anterior view. In H, late postoperative appearance, posterior view.
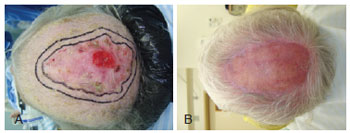
Figure 2 - Case 7. In A, squamous cell carcinoma in the biparietal region. In B, late postoperative appearance after reconstructive surgery with partial skin graft.

Figure 3 - Case 11. In A, squamous cell carcinoma in the right parietal region. In B, intraoperative appearance showing defect due to tumor resection. In C, production of the scalp flap based on the occipital vessels. In D, late postoperative appearance of the donor area (skin graft). In E, late postoperative appearance.

Figure 4 - Case 14. In A, squamous cell carcinoma in the left parietal region. In B, panoramic view of ulcerative-infiltrative lesions. In C, anatomopathologic part and defect due to tumor resection. In D, panoramic view of the defect, with exposure of the dura mater. In E, production of the scalp flap based on occipital vessels. In F, detail of the reconstruction of the defect and skin graft in the donor area of the flap. In G, late postoperative appearance, panoramic view of the flap. In H, late postoperative appearance, showing the donor area with an excellent skin graft result.

Figure 5 - Case 16. In A, squamous cell carcinoma in the right biparieto-occipital region. In B, panoramic view of the lesion. In C, defect due to tumor resection, with exposure of the dura mater. In D, dissection of the microsurgical latissimus dorsi myocutaneous flap, shaped as a lily flower. In E, reconstruction of the defect with microsurgical latissimus dorsi myocutaneous flap. In F, image showing the access to facial vessels for end-to-end microsurgical anastomosis. In G, late postoperative appearance, profile view. In H, posterior view of the microsurgical latissimus dorsi myocutaneous flap.

Figure 6 - Case 19. In A, squamous cell carcinoma in the left fronto-orbital region. In B, panoramic view of the lesion and demarcation of surgical margins. In C, demarcation of frontal craniotomy (neoplasia with bone invasion). In D, defect with exposure of the dura mater and production of the scalp flap based on temporal vessels. In E, late postoperative appearance, anterior view. In F, late postoperative appearance, panoramic view.

Figure 7 - Case 21. In A, recurrent squamous cell carcinoma in the biparietal region. In B, appearance of the defect due to tumor resection. In C, production of pinwheel scalp flap (or "S" italic). In D, synthesis of the pinwheel scalp flap in advance-rotation, showing the skin graft layers in the donor area that was not primarily closed. In E, late postoperative appearance, panoramic view. In F, late postoperative appearance, lateral view.

Figure 8 - Case 24. In A, squamous cell carcinoma in the right fronto-orbital region. In B, image of the surgical specimen upon monoblock resection. In C, appearance of the defect due to tumor resection. In D, production of the scalp flap based on temporal vessels. In E, late postoperative appearance, anterior view. In F, panoramic view, showing good appearance of the skin graft on the flap donor area.

Figure 9 - Case 25. In A, squamous cell carcinoma in the right occipital region. In B, appearance of the resulting defect, with demarcation of the rhomboid triple flap. In C, synthesis of the rhomboid triple flap. In D, late postoperative appearance.
DISCUSSION
It is essential that an exchange of information and procedures between plastic surgeons and other oncology professionals occur within a multidisciplinary context to achieve a final positive outcome and to improve the quality of life of patients with cancer. Therefore it is also essential to assess the results obtained and to continually question the validity of the procedures in current usage and their impact on the level of satisfaction of the patient undergoing reconstruction.
The involvement of some of the 5 layers forming the scalp is observed in partial-thickness lesions; these are common situations that may or may not involve tissue loss, but in which there is no exposure of the bone structure of the skull and the pericranium is preserved. In these cases, it is possible to resect the impaired region and either close it by approximating the edges of the lesion or let it heal by secondary intention. To allow for construction of flaps in the presence of major defects, a detachment in the subgaleal plane is required. The characteristics of these flaps should be the same as the area that must be reconstructed, particularly in terms of thickness, color, and presence of hair follicles.
Due to the anatomy of the scalp and its high vascularity, with anastomoses between the main vascular pedicles, different types of flaps may be used with satisfactory results. The most commonly employed are the random flap, which does not have a defined pedicle, and the axial flap, which is used in situations in which a defined vascular pedicle is present.
The rotation flap is among the most commonly used local flaps for this region; this involves the rotation of a semicircular segment of skin, subcutaneous tissue, and galea from a pivot point until they reach the area of the defect that needs repair4. In this reconstructive procedure and depending on the size of the defect, the donor area of the flap may be closed primarily, or a second flap or even a partial skin graft may be required.
Another type of flap that is also very effective in scalp reconstruction is the advancement flap, in which the skin segment with the characteristics previously described advances straight to the region to be repaired, without rotation or translation movement. Depending on the location and, in particular, the extent of the defect, complex and larger flaps may be used, with consideration of the high vascularity of the scalp. Among these, we include the transposition flap, in which a flap of rectangular shape is immediately rotated on a pivot point to the adjacent region to be repaired, and the donor area is primarily sutured or grafted (partial skin graft). When local flaps cannot be used, partial extensive losses can be repaired with skin grafts in partial thickness layers. If the vascularized layers, such as the pericranium and/or the subcutaneous tissue are preserved, integration of the graft in the recipient area will occur as long as no local infection develops. However, the quality of the reconstruction obtained with this procedure is much lower when compared to local or free flaps.
Microsurgical flaps present several advantages. However, reconstructive microsurgery is demanding as it requires the involvement of professionals in different fields, the commitment of managers who assume responsibility for procedures of high complexity and hospital cost, and the establishment of adequate hospital support. Taking this into account, satisfactory results are essential for recognition of this procedure5. In the cohort analyzed in this study, out of all patients who presented with large scalp defects, a microsurgical flap was used in only one repair. A latissimus dorsi myocutaneous free flap offered good skin coverage, with different tissue composition, versatility in the production, and satisfactory results, and with low morbidity at the donor and recipient sites. This allowed these flaps to become an important option for the reconstruction of defects due to cancer6. In the presence of small defects, grafts or local flaps are usually indicated7.
In the literature, squamous cell carcinoma is the second most common type of skin cancer. However, in the cohort analyzed, it was the tumor with the highest incidence. The tumor develops initially as a papule or nodule, with varying degrees of hyperkeratosis and ulceration observed in photoexposed areas of elderly patients. The disease has been associated with immunosuppression, exposure to arsenical agents, radiation, chronic ulcer, and human papillomavirus. Despite being easily treatable, it may recur in advanced cases, promoting metastasis and leading to high morbidity and mortality rates8.
In the international literature, several procedures are already described for scalp reconstruction. In cases with extensive loss of soft tissue, microsurgical flaps are the commonly accepted option. Scalp reconstructions with advancement flaps represent a safe option as they are simple procedures that can provide satisfactory results.
It is also possible to transfer other local flaps, which cause lower morbidity of the donor area. This is achieved not only by continual technical improvement, but also by better anatomical knowledge and skills gained by plastic surgeons. The concept of a vascularized flap for perforating branches has now been introduced among the conservative surgical procedures. It is also important to maintain a multidisciplinary approach between the related specialties, with the aim of improving care for cancer patients. In this study, we reported the experience of the author in the repair of different cancer-related defects of the scalp. These may represent a challenge for young plastic surgeons, who need to adapt the fundamentals of applied plastic surgery to produce local flaps and, when necessary, to use microsurgical procedures and distant tissues9-12.
CONCLUSIONS
Scalp lesions remain a challenge for reconstructive surgery, because of the poor skin mobility of the region that, among other reasons, hinders the suturing of moderateand large-sized injuries. Interaction with the neurosurgery team, the head and neck surgeons, and the intensive care staff is essential for a stable postoperative recovery with the good peripheral perfusion that allows the nutrition of delicate grafts and flaps and leads to a positive outcome for the patient.
It is important for all plastic surgeons performing various therapeutic procedures to remember the basic principles of plastic surgery, which were efficiently described by Sir Harold Gillies. In our field, we epitomize the words of Ivo Pitanguy: "Plastic surgery, representing much of art, has its major limitation in the vascular pedicle. This puts our aspirations well short of those of sculptors, painters, and poets, who seek beauty as a source of freedom without limits." Humbly, I would add that when one reads "seek beauty," one should remember that plastic surgery in oncology is, in real life, a challenge for the surgeon to repair what is defective and reconstruct what is missing, always taking into account the aesthetic aspect.
In plastic surgery, studies on surgical procedures to repair large scalp defects resulting from cancer resection are important for their innovative aspect, thus less dependent on sample size, or for the consolidation of established procedures, requiring large samples with long-term follow-up.
REFERENCES
1. Torres ALG, Milcheski DA, Nakamoto HA, Tuma Junior P, Ferreira MC. Aplicação da microcirurgia no reparo de lesões complexas. Rev Soc Bras Cir Plást. 2009;24(2):131-7.
2. Marchac D. Deformities of the forehead, scalp and cranial vault. In: McCarthy JG, ed. Plastic surgery. Philadelphia: WB Saunders; 1990. p. 538-73.
3. Lin SJ, Hanasono MM, Skoracki RJ. Scalp and calvarial reconstruction. Semin Plast Surg. 2008;22(4):281-93.
4. Converse JM. Surgical closure of scalp defects. In: Kahn EA, Basset RC, Schneider RC, Crosby EC, eds. Correlative neurosurgery. Illinois: Charles Thomas; 1955.
5. Hurvitz KA, Kobayashi M, Evans GR. Current options in head and neck reconstruction. Plast Reconstr Surg. 2006;118(5):122e-33e.
6. Hussussian CJ, Reece GP. Microsurgical scalp reconstruction in the patient with cancer. Plast Reconstr Surg. 2002;109(6):1828-34.
7. Chun YS, Verma K. Single-stage full-thickness scalp reconstruction using acellular dermal matrix and skin graft. Eplasty. 2011;11:e4.
8. Rinker MH, Fenske NA, Scalf LA, Glass LF. Histologic variants of squamous cell carcinoma of the skin. Cancer Control. 2001;8(4):354-63.
9. Baker SR, Swanson NA. Local flaps in facial reconstruction. St Louis: Mosby; 1995.
10. Alpert BS, Buncke Jr HJ, Mathes SJ. Surgical treatment of the totally avulsed scalp. Clin Plast Surg. 1982;9(2):145-59.
11. Miller GD, Anstee EJ, Snell JA. Successful replantation of an avulsed scalp by microvascular anastomoses. Plast Reconstr Surg. 1976;58(2):133-6.
12. Orticochea M. Four flap scalp reconstruction technique. Br J Plast Surg. 1967;20(2):159-71.
Plastic surgeon performing microsurgical tumor resection at the Fundação Pio XII do Hospital de Câncer de Barretos (Pio XII Foundation of the Cancer Hospital of Barretos), full member of the Brazilian Society of Plastic Surgery, Barretos, SP, Brazil.
Correspondence to:
Cleyton Dias Souza
Alameda Holanda, 165 - City Barretos
Barretos, SP, Brazil - CEP 14784-001
E-mail: drcleytondias@gmail.com
Article submitted to SGP (Sistema de Gestão de Publicações/ Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: January 11, 2012
Article accepted: February 17, 2012
This study received the honorable mention for the Nemer Chidid 2011 prize.
This study was performed at the Fundação Pio XII do Hospital de Câncer de Barretos (Pio XII Foundation of the Cancer Hospital of Barretos), Barretos, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter