

Original Article - Year 2012 - Volume 27 -
Eyelid repair using an autologous conchal cartilage graft
Reconstrução palpebral com enxerto de cartilagem autóloga de concha de orelha
ABSTRACT
BACKGROUND: In this study, we evaluated the results obtained with Matsuo's technique for eyelid reconstruction at the Clínica de Cirurgia Plástica do Hospital Felício Rocho (Plastic Surgery Clinic of the Hospital Felício Rocho) from December 1992 to May 2011. Furthermore, we performed a nonsystematic review of published articles reporting eyelid repair using conchal cartilage graft from the ear.
METHODS: We studied 13 patients who were subjected to eyelid reconstructions after resection of neoplasias.
RESULTS: We observed satisfactory results in all patients, with spontaneous epithelialization of the conchal cartilage. In the nonsystematic literature review, we found 10 articles, covering 111 patients, that reported the use of ear cartilage for eyelid repair with good results.
CONCLUSIONS: Thus, the Matsuo technique appears to be a good option for eyelid repair.
Keywords: Eyelids/surgery. Eyelid neoplasms. Transplantation, autologous. Ear auricle.
RESUMO
INTRODUÇÃO: Neste estudo, foram avaliados os resultados alcançados com a técnica de Matsuo para reconstrução palpebral na Clínica de Cirurgia Plástica do Hospital Felício Rocho, entre dezembro de 1992 e maio de 2011. Além disso, foi realizada revisão não-sistemática de artigos publicados sobre reconstrução palpebral com cartilagem de concha de orelha.
MÉTODO: Foram estudados 13 pacientes submetidos a reconstrução palpebral após ressecção de neoplasias.
RESULTADOS: Em todos os pacientes, os resultados observados foram satisfatórios, com epitelização espontânea da cartilagem de concha de orelha. Na revisão não-sistemática da literatura foram encontrados 10 trabalhos, totalizando 111 pacientes, que utilizaram cartilagem da orelha para reconstrução, com bons resultados.
CONCLUSÕES: A técnica de Matsuo mostra-se uma boa opção para a reconstrução palpebral.
Palavras-chave: Pálpebras/cirurgia. Neoplasias palpebrais. Transplante autólogo. Pavilhão auricular.
The eyelid protects the ocular globe. Its occlusion assures physical protection of the eye, and blinking aids in lubrication and cleaning by spreading tears.
Eyelid defects may be congenital or iatrogenic, or may be a result of neoplasia, trauma, or infection, any of which may affect eyelid function. Plastic surgery aims at recovering the protective function of the eyelid, while using techniques that will also lead to good aesthetic results1.
The eyelid repair techniques in current usage range from primary intention healing and cutaneous flaps to cartilage grafts associated with cutaneous, myocutaneous, and microsurgical flaps, depending on the extent of the anatomical defect.
Surgical anatomy divides the eyelid into 3 lamellae: anterior, intermediate, and posterior. The anterior lamella is composed of skin and the orbicular muscle of the eye. The medial lamella is defined by the combination of the orbital septum, orbital fat, and submuscular fibroadipose tissue. The posterior lamella includes the fascia of the lower eyelid, the tarsus, and the conjunctiva2. It is important to emphasize that the term "lamella", although widely used and well defined, is not a term used in the Terminologia Anatômica da Sociedade Brasileira de Anatomia (Anatomical Terminology of the Brazilian Society of Anatomy).
Eyelid defects are divided into 2 groups, according to the structures involved: partial, when the posterior lamella is preserved; and total, when all lamellae are compromised3. In full-thickness defects, it is necessary to repair the eyelid support; the tarsus, composed of cartilage-free, dense connective tissue, normally provides this support.
Eyelid lesions may be repaired by flaps composed of cartilage and mucosa from the nasal septum, mucoperiosteum of the hard palate4, palate mucosa, allogenic preserved sclera5, epiglottis6, fascia lata7, ear scapha8, or conchal cartilage9-17.
In 1987, Matsuo et al.17 published a technique of eyelid repair using a conchal cartilage graft, which simplified the prevalent processes by avoiding the need for mucosa flaps to repair the conjunctiva of the ocular bulb. The conchal cartilage graft epithelializes quickly and is easy to obtain.
In the present study, we aimed to report the results obtained from the use of the Matsuo technique at the Clínica de Cirurgia Plástica do Hospital Felício Rocho (Plastic Surgery Clinic of the Hospital Felício Rocho) (Belo Horizonte, MG, Brazil), as well as conduct a nonsystematic review of the relevant literature.
METHOD
Case Series
All patients subjected to eyelid repair at the Clínica de Cirurgia Plástica do Hospital Felício Rocho (Plastic Surgery Clinic of the Hospital Felício Rocho) from December 1992 to May 2011 were retrospectively evaluated by collecting data from photos and medical records. All patients who had their eyelids repaired with conchal cartilage were selected.
We collected data on gender, age, reason for repair, and outcome of the surgery.
The results were evaluated by the authors using the following parameters: (1) ability to occlude the eyelids; (2) signs of lagophthalmos or ectropion; (3) symmetry; (4) morbidity of the flap donor area; and (5) epithelialization of the cartilage.
The morbidity of the donor area was evaluated by the presence or absence of hypertrophic scar, infection, or local hematoma.
Epithelialization was clinically evaluated by the authors through visual inspection after eversion of the repaired eyelid (comparison of the macroscopic appearance of the tissue covering the flap and the adjacent mucosa, considering that there was epithelialization when the tissues were similar) and complaint of discomfort from the patient (the following symptoms were queried: foreign body sensation, pruritus, and pain).
The results were considered satisfactory when 4 of the 5 parameters were noted, and when eyelid occlusion was possible.
Nonsystematic Review of the Literature
Primary Internet research was conducted using MEDLINE using the search term "eyelid reconstruction and cartilage". The search spanned from 1987 (the year in which Matsuo's article was published) to 2011. Only articles published in English and Portuguese were included in this work.
The articles that were included as references in the articles found through the primary MEDLINE search were also included for review. All articles that fulfilled the established criteria were reviewed by the authors for future inclusion in the study.
Surgical Technique
Marking and resection of the lesions was performed through simple macroscopic evaluation in 10 cases, or through transoperative microscopic evaluation of cryosections (Mohs micrographic surgery) in 3 cases. Intravenous sedation and local or general anesthesia were used, depending on the case. After evaluation of the defect, the amount of cartilage required for correction was determined. There was no histopathological analysis on cryosections in any of the cases other than the 3 micrographic Mohs procedures, which were performed for the 3 patients with relapse of sclerodermiform basocellular carcinoma.
An incision was made in the skin of the anterior margin of the ear concha, in the region of transition between the concha and the antihelix, thereby hiding the scar in the natural irregularity of that area. The required piece of cartilage was removed, with perichondrium only on the side of the inward curvature. Flaws on the surface with the perichondrium were avoided. After hemostasis, the skin was sutured with 6-0 nylon or 5-0 Monocryl, with transfixed stitches in the donor area of the outer ear, to avoid the occurrence of an empty space.
After adjusting the graft size such that it was 1 mm smaller than the defect, the cartilage graft was placed with the curvature turned to the conjunctiva of the eye bulb and was fixed to the residual tarsus with Vicryl or Monocryl 5-0 sutures.
The cartilage graft was covered with local cutaneous or myocutaneous flaps or with local muscle and skin flaps. The local cutaneous or myocutaneous flaps were fixed to the conchal cartilage with 2 or 3 transfixed U stitches, with care taken not to involve the entire thickness of conchal cartilage that can potentially cause a corneal ulceration by rubbing with the thread.
RESULTS
Case Series
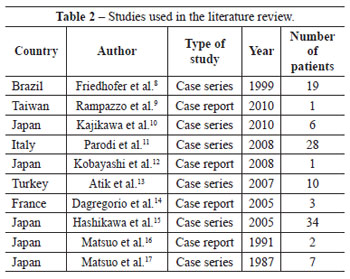
Thirteen patients were found who fulfilled the inclusion criteria for the study (Table 1). The patients were followed for variable periods of time, ranging from 2 to 216 months, with a mean of 49.8 months and a median of 24 months.
Most patients were female (8/13, 61.5%), and the mean age was 64.5 years.
Eyelid repair was needed in all patients as a consequence of loss of tissue caused by resection of cutaneous neoplasia. In 9 cases was reconstructed exclusively the lower eyelid and, in one patient, only the upper eyelid. In 3 patients, there was a need to approach more than one facial structure, and a case of association of the lower eyelid and the malar region, the second, both eyelids and the lateral commissure, and the third, the lower eyelid and lateral commissure. Basocellular carcinoma was responsible for most of the cases (69%)(Table 1).
All patients had satisfactory results according to the criteria established by the study. None of the patients had complications in the donor area. The macroscopic appearance of the tissue covering the flap was considered to be similar to the normal adjacent mucosa in all cases; it was thus considered that epithelialization of the flap had occurred. One patient complained of discomfort at the site of the flap.
One of the patients developed trichiasis and a subsequent ulcer of the cornea that was treated by a specialist. Another patient developed eyelid ptosis after a combined repair of the upper and lower eyelids, as well as the lateral commissure. This sequela was corrected at another operation, through lateral canthotomy and suspension of the eyelid to the frontal muscle with silicone. A third patient presented with partial necrosis of the myocutaneous flap over a 2-mm² area, which evolved satisfactorily after conservative treatment.
There were 2 cases of relapse of the primary disease during the postoperative follow-up period in patients with dermatofibrosarcoma and squamous cell carcinoma. A patient with a protruding dermatofibrosarcoma that simulated a keloid tumor had been subjected to 18 years of treatment with repeated injections of corticosteroids at another clinic prior to undergoing a wider resection with reconstruction of the right lower eyelid and malar region. However, the patient presented with relapse of the lesion 7 years after the first surgery and died after extensive surgery was performed to treat the relapse. The other case of relapse occurred in a patient with invasive squamous cell carcinoma, with locoregional metastases developing 5 months after removal of the lesion. The tumor evolved aggressively and was resistant to treatment, leading to the patient's death 12 months later.
The Figures 1 to 3 illustrate some cases in this series.

Figure 1 - In A, basocellular carcinoma affecting the left lower eyelid. In B, conchal cartilage graft from the left ear. In C, Mustardé flap and suture of the donor area. In D, 3 months postoperatively, with cicatricial retraction and scleral-show but good form of the repaired eyelid. In E, 3 months postoperatively, indicating good juxtaposition but irregularities in the margins of the repaired eyelid.
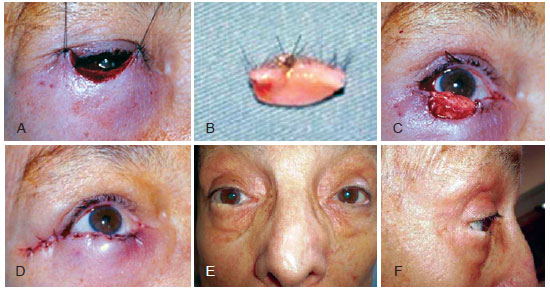
Figure 2 - In A, defect of the total thickness of the right lower eyelid, affecting approximately 75% of its extension, after resection of the basocellular carcinoma. In B, excised piece of eyelid. In C, conchal cartilage in place. In D, cover of the graft with McIndoe myocutaneous flap. In E, late postoperative result showing discrete irregularity in the margins of the repaired eyelid, but good conformation and juxtaposition to the ocular globe. In F, late postoperative result with discrete irregularity at the margin of the repaired eyelid, maintaining good conformation and juxtaposition to the ocular globe.

Figure 3 - In A, melanoma of the right upper eyelid, after excisional biopsy. In B, residual defect after amplification of the surgical margins. In C, conchal cartilage in place; marking of the myocutaneous flap of the lower eyelid. In D, healed myocutaneous flap in the lower eyelid covering the cartilage. In E, postoperative result after release of the pedunculus of the lower eyelid flap, with light ptosis. In F, postoperative result indicating preservation of both function and aesthetics.
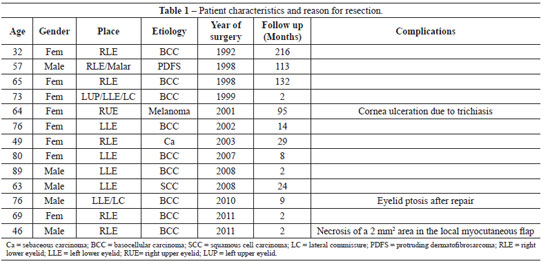
Literature Review
We found 10 articles that fulfilled the established inclusion criteria (Table 2). The studies were case reports or case series, covering 111 patients.
In 1987, Matsuo et al.17 were the first to describe the technique of eyelid repair with conchal cartilage graft. These authors emphasized the low morbidity in the donor area and shorter procedure time. It was also observed that removal of the cartilage graft is quick and that it leaves an imperceptible scar. There is no need to reconstruct the conjunctiva of the eyelid. The conchal cartilage spontaneously epithelializes when in contact with the conjunctiva of the bulb, besides being perfectly compatible anatomically with the contacting tissues16,17. Except for Friedhofer et al.8 and Hashikawa et al.15 who used the scapha cartilage to reconstruct the eyelid, all other studies we reviewed used the conchal cartilage and followed the Matsuo technique17.
Rampazzo et al.9 used palate mucosa to repair the eyelid conjunctiva, which is unnecessary when following the original technique. The other authors did not repair the eyelid conjunctiva, expecting epithelialization of the graft, as described by Matsuo et al.17.
Atik et al.13 reported complications in a patient who presented with conjunctival hyperemia and corneal abrasion. Hashikawa et al.15 needed to reoperate on 2 patients who had bad placing of the cartilage graft after rupture of the fixation point in the medial corner. The other authors did not report complications.
The results found in all articles were satisfactory, with restoration of function and eyelid aesthetics.
DISCUSSION
The eyelid is a peculiar structure that is functionally and aesthetically very important. Eyelid repair is a difficult task because of the specific anatomy of the region.
Two interesting points when attempting eyelid reconstruction are the tissue chosen for substitution of the posterior lamella and the need to graft for the conjunctiva. The series of cases and the literature reported here show that using conchal cartilage for the reconstruction offers an adequate solution for both questions.
Few tissues described in the literature have been shown to be as adequate a substitute for the posterior lamella (tarsus and conjunctiva) as the conchal cartilage with perichondrium16,17. Its shape fits perfectly in the ocular bulb, maintaining uniform and continuous contact with the conjunctiva. Its texture - that of elastic cartilage, which is delicate and not too rigid but firm nonetheless - is also responsible for the suitable coverage of the ocular bulb16,17. Conchal cartilage is used to repair eyelid defects caused by tumors11,13 and trauma9, and even the large defects that follow maxillectomies10. Reconstruction with free flaps associated with the conchal cartilage for eyelid repair has also been described10,12,14.
It is important to highlight that the cartilage of the scapha is also an excellent choice for eyelid repair, as shown by Friedhofer et al.8 and Hashikawa et al.15. At our institution, staff are not experienced in the use of the scapha; therefore, the original technique of Matsuo is used.
Saad and Falla18 reported treatment of tracheal stenosis in children, which was performed using a cartilage graft, with the perichondrium turned to the tracheal lumen. Spontaneous epithelialization occurred in the adjacent mucosa, without relapse of stenosis. Matsuo et al.17 published their initial article based on this work and observed that the cartilage spontaneously epithelializes in 3 to 4 weeks.
This capacity for spontaneous epithelialization was confirmed in the work of Nigro et al.19. This experimental study in rabbits showed that cartilage with perichondrium epithelializes faster and more uniformly than cartilage without perichondrium. In humans, this decreases surgical time, because it avoids the need for reconstruction of the posterior lamella, as was usually performed with the Matsuo technique.
Fernandes et al.20 indicated the morbidity associated with the use of mucosa from the palate to repair the posterior lamella. The disadvantages of this type of graft are as follows: (1) the surgeon may be unfamiliar with the donor region; (2) the graft may contain a minor salivary gland, leading to mucoid secretion that is difficult to treat; and (3) metaplasia of the epithelium occurs 3 to 6 months after surgery, making the technique unadvisable for upper eyelid repair because of the risk of corneal abrasion. Postoperative pain and discomfort were also reported with this type of graft. All these complications can be avoided with the Matsuo technique. The low morbidity of the donor area9,11,16,17 is another important factor in the choice of the technique. In 2008, Parodi et al.11 published a series of 28 cases of eyelid repair with the modified Matsuo technique; they observed that all the grafts integrated. None of the patients developed ectropion or lagophthalmos, or presented with complications in the donor area.
In this series of cases, we observed that all 13 patients evolved satisfactorily. The 3 cases with complications were treated without major difficulties.
CONCLUSIONS
The technique for eyelid repair originally described by Matsuo et al.17 is reproducible, has a low incidence of complications, and provides good results from both the functional and the aesthetic points of view.
REFERENCES
1. Mélega JM, Viterbo F, Mendes FH. Cirurgia plástica: os princípios e a atualidade. Rio de Janeiro: Guanabara Koogan; 2011. p. 573-4.
2. Kakizaki H, Malhotra R, Madge SN, Selva D. Lower eyelid anatomy: an update. Ann Plast Surg. 2009;63(3):344-51.
3. Newman MI, Spinelli HM. Reconstruction of the eyelids, correction of ptosis, and canthoplasty. In: Thorne CH, ed. Grabb and Smith's Plastic Surgery. 7th ed. Philadelphia: Lippincott Williams & Wilkins; 2007. p. 397-416.
4. Ito R, Fujiwara M, Nagasako R. Hard palate mucoperiosteal graft for posterior lamellar reconstruction of the upper eyelid: histologic rationale. J Craniofac Surg. 2007;18(3):684-90.
5. Kamiya H, Kitajima Y. Successful use of preserved sclera of eyelid reconstruction. Eur J Dermatol. 2003;13(3):267-71.
6. Adams JL, Olson NR, Siders DB. The use of the epiglottis as an autologous composite graft in eyelid reconstruction. Ophthal Plast Reconstr Surg. 1993;9(3):206-11.
7. Matsumoto K, Nakanishi H, Urano Y, Kubo Y, Nagae H. Lower eyelid reconstruction with a cheek flap supported by fascia lata. Plast Reconstr Surg. 1999;103(6):1650-4.
8. Friedhofer H, Salles AG, Jucá MCCR, Ferreira MC. Eyelid reconstruction using cartilage grafts from auricular scapha. Eur J Plast Surg. 1999;22(2-3):96-101.
9. Rampazzo A, Gharb BB, Chi Chen H. Total lower eyelid reconstruction with free posterior auricular chondrocutaneous flap. J Plast Reconstr Aesthet Surg. 2010;63(4):e384-6.
10. Kajikawa A, Ueda K, Katsuragi Y, Hirose T, Asai E. Three-step orbitofacial reconstruction after extended total maxillectomy using free RAM flap and expanded cervicofacial flap with cartilage grafts. J Plast Reconstr Aesthet Surg. 2010;63(10):1608-14.
11. Parodi PC, Faini G, De Biasio F, Rampino Cordaro E, Guarneri GF, Miani F. Full-thickness lower eyelid reconstruction with a conchal chondro-perichondral graft and local coverage with miocutaneous flaps: our divisional experience. J Oral Maxillofac Surg. 2008;66(9):1826-32.
12. Kobayashi K, Ishihara H, Murakami R, Kinoshita N, Tokunaga K. Total lower eyelid reconstruction with a prefabricated flap using auricular cartilage. J Craniomaxillofac Surg. 2008;36(2):59-65.
13. Atik B, Tan O, Bekerecioglu M, Cinal A, Tekes L. Reconstruction of lower eyelid defects using a cross upper eyelid flap composited with ear cartilage. Dermatol Surg. 2007;33(6):709-12.
14. Dagregorio G, Darsonval V. Post-ablative reconstruction of the medial canthus and medial orbital wall using conchal cartilage graft with three illustrative cases. Br J Plast Surg. 2005;58(8):1152-7.
15. Hashikawa K, Tahara S, Nakahara M, Sanno T, Hanagaki H, Tsuji Y, et al. Total lower lid support with auricular cartilage graft. Plast Reconstr Surg. 2005;115(3):880-4.
16. Matsuo K, Sakaguchi Y, Kiyono M, Hataya Y, Hirose T. Lid margin reconstruction with an orbicularis oculi musculocutaneous advancement flap and a conchal cartilage graft. Plast Reconstr Surg. 1991;87(1):142-5.
17. Matsuo K, Hirose T, Takahashi N, Iwasawa M, Satoh R. Lower eyelid reconstruction with a conchal cartilage graft. Plast Reconstr Surg. 1987; 80(4):547-52.
18. Saad SA, Falla A. Management of intractable and extensive tracheal stenosis by implantation of cartilage graft. J Pediatr Surg. 1983;18(4):472-4.
19. Nigro MV, Friedhofer H, Natalino RJ, Ferreira MC. Comparative analysis of the influence of perichondrium on conjunctival epithelialization on conchal cartilage grafts in eyelid reconstruction: experimental study in rabbits. Plast Reconstr Surg. 2009;123(1):55-63.
20. Fernandes JBVD, Nunes TP, Matayoshi S, Moura EM. Enxerto de mucosa do palato duro: complicações na área doadora. Relato de casos. Arq Bras Oftalmol. 2003;66(6):884-6.
1. Doctor in Surgery from the Universidade Federal de Minas Gerais (Federal University of Minas Gerais), full member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society for Plastic Surgery) - SBCP, Professor of Surgical and Anesthetic Techniques of the Faculdade de Medicina da Universidade de Itaúna (Faculty of Medicine of the University of Itaúna), staff of the Plastic Surgery Clinic of the Hospital Felício Rocho, staff of the Instituto de Cirurgia Plástica Avançada (Institute for Advanced Plastic Surgery), Belo Horizonte, MG, Brazil.
2. Aspiring member of the SBCP, postgraduate of the Plastic Surgery Service of the Hospital Felício Rocho, Belo Horizonte, MG, Brazil.
3. Full member of SBCP, member of the Serviço de Cirurgia Plástica do Hospital Felício Rocho (Plastic Surgery Clinic of the Hospital Felício Rocho), member of the Instituto de Cirurgia Plástica Avançada (Institute for Advanced Plastic Surgery), Belo Horizonte, MG, Brazil.
Correspondence to:
Rebeca Paohwa Liu
Rua Dionísio Cerqueira, 42 - ap. 301 - Gutierrez
Belo Horizonte, MG, Brazil - CEP 30430-140
E-mail: rebeca_liu@hotmail.com
Article submitted to SGP (Sistema de Gestão de Publicações/ Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: June 22, 2011
Article accepted: February 24, 2012
Study conducted at the Clínica de Cirurgia Plástica do Hospital Felício Rocho (Plastic Surgery Clinic of the Hospital Felício Rocho), Belo Horizonte, MG, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter