

Original Article - Year 2012 - Volume 27 -
A rhytidoplasty technique without resultant periauricular scarring
Ritidoplastia sem cicatriz periauricular
ABSTRACT
BACKGROUND: Surgical skin incisions in rhytidoplasty are very diverse compared to their original form approximately 100 years ago, when the operation was first performed. Many strategies have been proposed to improve this procedure so as to reduce scarring, anatomic distortion of the external ear, and hair loss. To diminish the inconveniences of periauricular scars and hair loss and in order to apply the technique to patients of different age groups, rhytidoplasty without preauricular and retroauricular incisions were performed using 2 surgical access points: the hairline on the temporal region and the submental region. The aim of this study is to report the results obtained using this rhytidoplasty technique which avoided periauricular scarring.
METHODS: From October 2008 to February 2012, 228 patients (80% female) underwent rhytidoplasty performed by means of a short incision instead of a coronal incision. Patients received cervical treatment through a submental access, which facilitated an extensive selective dissection linked to the midface plane for platysma treatment and, when necessary, resection of excess skin. SMAS-plasty, liposuction, fat graft, and laser treatment, in addition to other non-surgical procedures, were selectively combined in the same procedure or an additional procedure. The procedure is contraindicated in patients who present after extensive weight loss and with excessive flaccidity of facial and cervical skin.
RESULTS: Overall, the aesthetic results obtained with rhytidoplasty without periauricular scarring were considered satisfactory both by the patients and the surgical team and provided good mid-and long-term results. Few complications were observed after surgery; these included asymmetry in the temporal region and non-aesthetic scars, which were detected in 2.6% and 2.2% of the patients, respectively.
CONCLUSIONS: Rhytidoplasties without periauricular scarring that were performed through submental and precapillary incisions in the temporal region provided good mid-to long-term results. This justified their use, particularly if we consider that treatment of the midface plane and cervical region might prevent the development of possible complications described in the literature.
Keywords: Face/surgery. Rhytidoplasty. Plastic surgery/methods.
RESUMO
INTRODUÇÃO: As incisões cutâneas de acesso nas ritidoplastias têm apresentado grande diversidade desde os seus primórdios, nas duas primeiras décadas do século passado, até a atualidade. Numerosas também têm sido as táticas cirúrgicas em busca de refinamentos que pudessem reduzir estigmas cicatriciais, distorções anatômicas da orelha externa e perda de cabelo. No sentido de reduzir as inconveniências das cicatrizes periauriculares e das alterações pilosas ainda frequentes, com aplicabilidade numa ampla gama de pacientes de diferentes faixas etárias, foi proposta a realização da ritidoplastia sem incisão pré e retroauricular, mediante duas vias de acesso: uma no limite piloso da região temporal e outra, submentoniana. Este estudo tem por objetivo apresentar os resultados obtidos com o emprego dessa técnica de ritidoplastia sem cicatriz periauricular.
MÉTODO: No período de outubro de 2008 a fevereiro 2012, 228 pacientes, sendo 80% do sexo feminino, foram submetidos a ritidoplastia mediante uma incisão curta e sem incisão coronal, no Centro Médico Imbanaco (Cali, Colômbia). Todos os pacientes receberam tratamento cervical mediante via de acesso submentoniana com ampla dissecção seletiva e interligada com o andar médio da face, para tratamento do platisma, quando necessário, e ressecção dos excessos cutâneos. Smasplastia, lipoaspiração, enxerto de gordura e laser, além de outros procedimentos não-cirúrgicos, foram utilizados concomitante e seletivamente, no mesmo ato ou em atos operatórios distintos. A técnica foi contraindicada a pacientes após grandes perdas ponderais e excessiva flacidez de pele tanto facial como cervical.
RESULTADOS: Os resultados estéticos obtidos com a técnica de ritidoplastia sem cicatriz periauricular foram considerados satisfatórios pelos pacientes e pela equipe cirúrgica na totalidade dos pacientes, com manutenção a médio e longo prazos. A incidência de complicações pós-operatórias foi pequena, sendo mais comum a presença de assimetria da região temporal e de cicatrizes não-estéticas em 2,6% e 2,2% dos pacientes, respectivamente.
CONCLUSÕES: As ritidoplastias com vias de acesso submentoniana e pré-capilar na região temporal, sem cicatrizes periauriculares, têm oferecido resultados a médio e longo prazos que justificam sua indicação, pelo fato de permitirem tratamento do andar médio da face e da região cervical, evitando-se as possíveis complicações descritas na literatura.
Palavras-chave: Face/cirurgia. Ritidoplastia. Cirurgia plástica/métodos.
Human aging is caused by biological factors related to our species that involve different types of tissue atrophy and absorption whose effects act on the skin. In the face, these effects begin to appear in the fourth decade of life, a period in which genetics, quality of life, body mass changes, skin type, hormones, nutrition, smoking, and even gravity, may be considered to be the causes1,2.
Facial rhytidoplasty was introduced as a plastic surgery technique in the first 2 decades of the past century. Technical improvements, strategies, and refinements are being continually developed as surgeons assess results in both male and female patients. In the past decades, rhytidoplasty stopped being considered a "state secret," and patients no longer deny having undergone this surgery. At present, the results obtained with this procedure, and the comparison between scars, events, and complications are well known and openly discussed.
There is constant improvement in strategies and techniques in the ongoing effort to obtain satisfactory long-term results. The incisions that provide surgical access to rhytidoplasty have always been made on the scalp and around the ears. The length of the dissections varied according to the need of the patient. Minor inconveniences included hair loss, scars that are often considered unsightly, and other problems that required surgical repair (Figure 1).
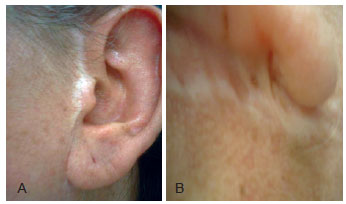
Figure 1 - Types of scar ruptures frequently found in late postoperative rhytidoplasties, which already evolve into complications when they are noted. In A, preauricular scar. In B, retroauricular scar.
Platysma3 and superficial musculo-aponeurotic system (SMAS)4 treatment, use of endoscopy in different dissection planes5, new procedures, strategies, and techniques that are currently used (and should continue to be used in the future) always involve the area around the ear as a surgical access point. Recently, it was proposed that rhytidoplasty without periauricular scarring performed with simultaneous SMAS treatment can be performed through preauricular and temporal incisions alone6.
To diminish the inconveniences of periauricular scars and frequent hair loss and in order to apply the technique to patients of different age groups, rhytidoplasty without preauricular and retroauricular incisions was performed using 2 surgical access points: the hairline on the temporal region and the submental region. The aim of this study is to report the results obtained using the rhytidoplasty procedure with and without resulting periauricular scarring.
METHOD
From October 2008 to February 2012, 228 patients, 80% of whom were female, underwent rhytidoplasty performed by means of a short incision instead of a coronal incision. Patients received cervical treatment through the submental access, which can lead to an extensive selective dissection linked to the midface plane for platysma treatment and, when necessary, to resection of excess skin. SMAS-plasty, liposuction, fat graft, and laser treatment, in addition to other non-surgical procedures, were selectively combined in the same operation or another procedure. The procedure was considered to be contraindicated in patients who presented after extensive weight loss and with excessive flaccidity of the facial and cervical skin.
Surgical Procedure
A first demarcation of the area of skin to be dissected was performed on the face and neck. The dissection was performed in the temporal region starting from the root of the helix on the hairline. The length of the incision varied from 5 cm to 7 cm. Starting from the opposite site of the helix, the demarcation was extended up to the orbital rim, going from the outer corners of the nasolabial folds and caudal to the mandibular margin. On the border of the root of the helix, the incision circumvented the tragus and proceeded until the earlobe and the mandibular line.
With regard to the neck, demarcations were performed by a transverse line on the borders of the hyoid bone or even 3 cm below and by a vertical line starting from the earlobe and proceeding bilaterally (Figure 2).

Figure 2 - Patient profile, with skin demarcation, delimited in the area of dissection of the temporal region, on the entire face, going from the anterior ear line up to 1 cm from the outer eyelid corner, to then move down to the outer corners of the nasolabial fold, mandibular line, and neck until reaching - and even up to 1.5 cm below - the hyoid bone.
All patients underwent surgery under sedation and local anesthesia with lidocaine 0.5% and epinephrine 1:200,000. The total volume that was injected varied between 200 mL and 300 mL.
A submental transverse incision, with an average length of 3 cm, was also made and was followed by a cervical cutaneous dissection within the area previously demarcated. A cutaneous linear or zigzag incision with a length of 5 cm to 7 cm was then made using an inclined scalpel in the cranial region. This incision, on the hairline of the temporal region, started on the root of the helix7. Then, subcutaneous dissection of the midface plane, selectively combined (or not) with cervical dissection, was finally performed (Figure 3).

Figure 3 - In A, surgical incision on the temporal region of the root of the helix and along the hairline with a length of 5 cm to 7 cm, performed with cranial inclined scalpel to better preserve the hair follicles. In B, large skin dissection through the incision on the area previously marked, to the mandibular line and combined or not with dissection of the cervical region.
The treatment of platysma bands in the cervical midline was performed8-12 using 3 to 5 single stitches or a continuous suture in a cephalic direction with 4-0 absorbable thread and SMAS-plasty13-15. Upon traction of the dissected skin of the face in the cranial direction, an incision of 3 cm to 4 cm was performed to remove the excess skin in the temporal region. Suturing in 2 planes of the dissected area was then performed applying 2 to 4 dermis stitches using 4-0 absorbable thread and single stitches with 5-0 nylon thread in linear and zigzag incisions, respectively (Figures 4 and 5). With regard to the submental region, in patients who had excess skin even after resection, the area dissected was sutured with subdermal single stitches using 4-0 absorbable thread.

Figure 4 - In A, final suture with single stitches performed with 4-0 non-absorbable thread. In B, six months after surgery.

Figure 5 - In A and B, zigzag pattern incision and suture with single dermal stitches performed with 4-0 absorbable thread. In C, final suture with single stitches performed with 4-0 non-absorbable thread. Skin fold that disappears 3 weeks after surgery.
Liposuction, fat graft, laser treatment, chemical peeling, forehead treatment, and blepharoplasty, in addition to other non-surgical procedures, were selectively combined in the same or separate surgeries.
Postoperative Care
The surgery was performed under sedation and the patients were discharged as soon as they could walk.
No drains were placed. A semi-compressed dressing was maintained for 24 hours, and the sutures were removed 5 days after surgery.
The severity of edema and ecchymosis that developed following this procedure was similar to that following rhytidoplasty with larger dissections and incisions.
RESULTS
Overall, the aesthetic results obtained with rhytidoplasty without periauricular scarring were considered satisfactory by both the patients and the surgical team and provided good mid-and long-term results.
Few complications were observed after surgery. Asymmetry in the temporal region and non-aesthetic scars were detected in 2.6% and 2.2% of the patients, respectively (Table 1).
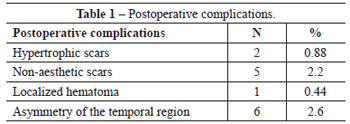
In this cohort, no infections, suture dehiscence, skin necrosis, seroma, permanent asymmetry, prolonged swelling, or nerve damage were observed.
Figures 6 to 10 illustrate some patients of this series.

Figure 6 - In A and B, preoperative and 7 days postoperative profile view, respectively, of a 53-year-old patient who underwent the described rhytidoplasty procedure with temporal and submental hairline incisions. In C, suture with single stitches performed with 4-0 non-absorbable thread and skin fold edema that disappears 3 weeks after surgery.

Figure 7 - In A, a 52-year-old patient who had previously undergone rhytidoplasty 5 years before and who underwent a new surgical procedure without preauricular or retroauricular incisions with the method described. In B and C, one year postoperative aspect.

Figure 8 - In A and B, profile views of a 50-year-old patient, preoperatively and 3 years postoperatively, who underwent rhytidoplasty with the method described. In C, close-up image without evidence of scarring in the temporal and sideburn region.
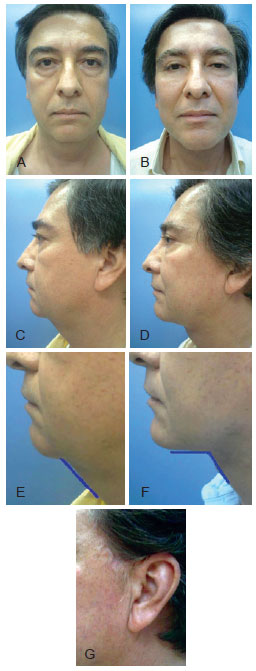
Figure 9 - In A and B, preoperative and 6 months postoperative frontal views, respectively, of a 62-year-old patient, who underwent blepharo-cervicofacial rhytidoplasty with platysma treatment and cervical liposuction, all performed in the same surgery. In C and D, preoperative and 6 months postoperative profile views, respectively. In E and F, preoperative and 6 months postoperative closed views, respectively, showing a clear improvement of the cervicomandibular angle. In G, the scar along the sideburns is not visible except at a short distance.

Figure 10 - In A and B, preoperative and 2 years postoperative frontal views, respectively, of a 70-year-old patient who underwent blepharo-cervicofacial rhytidoplasty without platysma treatment. In C and D, preoperative and 2 years postoperative profile views, respectively. In E, image of the incisional scar concealment performed for the procedure.
DISCUSSION
Skin dissection of the face and neck through 2 short and distant incisions, although more difficult from a technical point of view, may be easily performed with blunt-tip scissors, direct vision, and front light. Hemostasis is routinely achieved with no special equipment.
Because of the type of cranial traction sutures that are applied, the temporal surgical access used for the SMAS-plasty procedure does not present any limitation. The cranial traction provided by the skin flap raises the cranial excess skin on the ear and forms small folds that return to normality after 3 weeks (Figure 11).
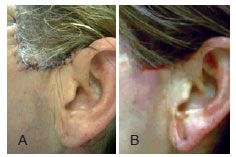
Figure 11 - In A, immediate postoperative image of small skin folds in the preauricular region because of the procedure employed. In B, disappearance of the skin folds 3 weeks after surgery.
Liposuction performed before platysma band treatment allows for the removal of their excess in the entire anterolateral region of the neck, as well as removal of their medial suture, which also may be performed with direct vision. Skin dissection of large face and neck regions is selectively performed according to the excess skin that needs to be removed in the neck. This leads to a better release of the cranial traction and rejuvenation of the mandibular line.
The absence of periauricular scars is an important achievement obtained with this procedure. It avoids secondary deformations, which are otherwise frequently observed, as well as aesthetic impairments of the tragus, earlobe, and sideburns. When already adherent before surgery and if surgically manipulated, the earlobe has the tendency to undergo more traction in the late postoperative period. If it is not dissected, the cranial traction of the skin in this region inhibits its semirotation and retains a more natural appearance.
Male patients with short hair or with total parietal alopecia might also benefit from the position of the scar.
Ancillary procedures of the dissected areas with laser treatment and peeling performed in the same surgery become safer when performed in dissected areas because of the extensive dermal circulation from the auricular region and midface side.
CONCLUSIONS
Rhytidoplasty performed through temporal and submental incisions preserves the integrity of the skin and allows extensive dissection and realization of SMAS-plasty procedures, such as fills, liposuction, laser treatment, or chemical peeling, which are specifically indicated to be performed in a single surgery to reduce the surgical risks.
When rhytidoplasty is performed through a submental and precapillary access in the temporal region and without periauricular scarring, it provides mid-and long-term results that justify its indication, as it facilitates easy midface plane and cervical region treatment and avoids the possible complications described in the literature.
REFERENCES
1. Gonzalez-Ulloa M, Flores ES. Senility of the face: basic study to understand its causes and effects. Plast Reconstr Surg. 1965;36:239-46.
2. Gilchrest BA. Clinics in geriatric medicine. Vol. 5. Philadelphia: W.B. Saunders; 1989. p. 161-70.
3. Skoog T. Plastic surgery: new methods and refinements. Philadelphia: WB Saunders; 1974. p. 393-410.
4. Mitz V, Peyronie M. The superficial musculo-aponeurotic system (SMAS) in the parotid and cheek area. Plast Reconstr Surg. 1976;58(1):80-8.
5. Ramirez OM, Maillard GF, Musolas A. The extended subperiosteal face lift: a definitive soft-tissue remodeling for facial rejuvenation. Plast Reconstr Surg. 1991;88(2):227-38.
6. Baker DC. Minimal incision rhytidectomy (short scar face lift) with lateral SMASectomy: evolution and application. Aesthet Surg J. 2001;21(1):14-26.
7. Camirand A, Doucet J. A comparison between parallel hairline incisions and perpendicular incisions when performing a face lift. Plast Reconstr Surg. 1997;99(1):10-5.
8. Giampapa VC, Di Bernardo BE. Neck recontouring with suture suspension and liposuction: an alternative for the early rhytidectomy candidate. Aesthetic Plast Surg. 1995;19(3):217-23.
9. Giampapa V, Bitzos I, Ramirez O, Granick M. Suture suspension platysmaplasty for neck rejuvenation revisited: technical fine points for improving outcomes. Aesthetic Plast Surg. 2005;29(5):341-52.
10. Fuente del Campo A. Midline platysma muscular overlap for neck restoration. Plast Reconstr Surg. 1998;102(5):1710-5.
11. Ramirez OM, Robertson KM. Comprehensive approach to rejuvenation of the neck. Facial Plast Surg. 2001;17(2):129-40.
12. Guerrerosantos J. Managing platysma bands in the aging neck. Aesthet Surg J. 2008;28(2):211-6.
13. Feldman JJ. Corset platysmaplasty. Plast Reconstr Surg. 1990;85(3):333-43.
14. Stuzin JM, Baker TJ, Gordon HL, Baker TM. Extended SMAS dissection as an approach to midface rejuvenation. Clin Plast Surg. 1995;22(2):295-311.
15. Matarasso A, Elkwood A, Rankin M, Elkowitz M, Godek CP. National plastic surgery survey: face lift techniques and complications. Plast Reconstr Surg. 2001;106(5):1185-96.
1. Plastic surgeon, full member of the Colombian Society of Plastic Surgery, Cali, Colombia.
2. Plastic surgeon, full member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery), São Paulo, SP, Brazil.
Correspondence to:
Alfonso Riascos
Imbanaco Medical Center
Carrera 38A, 5A 100B - San Fernando
Cali, Cauca Valley, Colombia
E-mail: alfonso.riascos@imbanaco.com.co
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: March 6, 2012
Article accepted: May 11, 2012
This study was performed at the Centro Médico Imbanaco (Imbanaco Medical Center), Cali, Cauca Valley, Colombia.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter