

Original Article - Year 2012 - Volume 27 -
Supplementary implants in breast reconstruction
Implantes complementares na reconstrução mamária
ABSTRACT
BACKGROUND: Depression in the anterior wall of the axilla following mastectomy is distressing to patients when they wear summer clothing and may also cause difficulty in raising the arm if there are adhesions and retractions in the region. In these patients, we use supplementary implants that reconstitute the local anatomy in a satisfactory manner and which offer functional benefits by removing cicatricial adhesions. These implants are available in several sizes and volumes, and it is possible to use more than one prosthesis in the same location, if needed. The aim of this study is to report the experience of the Plastic Surgery Unit of the Federal University of Rio de Janeiro (Rio de Janeiro, RJ, Brazil) with the use of supplementary implants in breast reconstruction after mastectomy to improve the aesthetic appearance and function of the axillary region.
METHODS: Supplementary silicone implants were inserted for breast reconstruction following mastectomy in 6 female patients, aged 34 to 75 years. The volume of the implants ranged from 20 mL to 120 mL. The width, length, and depth of the axillary region were measured to define the volume and dimensions, as well as the number of implants to be used. The implants were inserted through the scar from the prior breast reconstruction.
RESULTS: The follow-up period ranged from 6 months to 8 years, and no capsular contracture was observed. All patients reported functional improvement in arm movement, as well as satisfaction with the aesthetic result, which allowed them to wear more revealing clothing.
CONCLUSIONS: The inclusion of semilunar silicone implants as a refinement in breast reconstruction is easy to perform, has predictable results, and requires only one surgical procedure. The implants may be replaced, augmented, or removed, as required.
Keywords: Breast implantation. Breast implants. Prostheses and implants. Mammaplasty.
RESUMO
INTRODUÇÃO: A depressão na parede anterior da axila pós-mastectomia gera insatisfação das pacientes ao vestirem roupas mais decotadas; além disso, pode haver dificuldade na elevação do braço quando há aderências e retrações nessa região. Nessas pacientes, utilizamos implantes complementares, que reconstituem a anatomia local de forma satisfatória, oferecendo benefícios funcionais ao remover bridas cicatriciais. Esses implantes estão disponíveis em variados tamanhos e volumes, podendo ser empregada mais de uma prótese no mesmo local, se necessário. O objetivo deste estudo é demonstrar a experiência da Disciplina de Cirurgia Plástica da Universidade Federal do Rio de Janeiro (Rio de Janeiro, RJ, Brasil) com o emprego de implantes complementares na reconstrução mamária pós-mastectomia, buscando melhorar os aspectos estético e funcional da região axilar.
MÉTODO: A inclusão de implantes de silicone complementares para reconstrução mamária pós-mastectomia foi realizada em 6 pacientes do sexo feminino, com idade entre 34 anos e 75 anos. O volume dos implantes variou de 20 ml a 120 ml. Largura, comprimento e profundidade da área da axila a ser preenchida foram mensurados, para definir volume, dimensões e número de implantes que seriam utilizados. A via de acesso utilizada para inserção dos implantes foi a cicatriz da reconstrução mamária.
RESULTADOS: O seguimento pós-operatório variou de 6 meses a 8 anos, não sendo observada contratura capsular em nenhum caso. Todas as pacientes referiram melhora funcional na movimentação do braço, bem como satisfação com o resultado estético pela possibilidade de uso de roupas mais decotadas.
CONCLUSÕES: A inclusão de implantes de silicone de formato semilunar no refinamento da reconstrução mamária é um método simples e de fácil realização, com resultados bastante previsíveis, necessitando apenas de uma cirurgia. Os implantes podem ser substituídos, aumentados ou removidos, se necessário.
Palavras-chave: Implante mamário. Implantes de mama. Próteses e implantes. Mamoplastia.
Surgeons who perform breast reconstructions are motivated to develop solutions to patients' requests for better results, within the limitations imposed by the mastectomy. The main focus is modeling the new breast to suit the body of the patient, and it often happens that the infraclavicular depression and/or the absence of the anterior axillary crease, which occur in many cases, are not considered.
Depression in the anterior wall of the axilla is often a complaint from patients, both because it becomes visible with the use of lighter clothing and because it may cause difficulties when raising the arm if there are adhesions and retractions in the region.
At present, adipose tissue flaps are the most commonly used method of repairing the infraclavicular depression1,2. In axillary wall deformities, repair with adipose tissue flaps is hindered because of cicatricial adhesions and extensive depression; this may lead to unsatisfactory results. In these cases, premade semilunar-shaped implants may be used3,4. Also called supplementary implants, they reconstitute the local anatomy and provide additional functional benefit of eliminating adhesions between the skin and the deeper plane, thus improving the extension of the arm. These supplementary implants are available in several sizes and volumes, and more than one implant may be used in the same place.
The aim of this study is to report the experience of the Plastic Surgery Unit of the Federal University of Rio de Janeiro (Rio de Janeiro, RJ, Brazil) with the use of supplementary implants in breast reconstruction after mastectomy to improve the aesthetic appearance and function of the axillary region.
METHOD
Insertion of semilunar-shaped supplementary breast implants (Silimed, Rio de Janeiro, RJ, Brazil) was performed in 6 female patients aged 34 to 75 years undergoing postmastectomy breast reconstruction using a myocutaneous flap from either the rectus abdominis muscle (2 cases) or the latissimus dorsi (4 cases).
Seven implants were used; one patient received 2 implants. The volume of the implants ranged from 20 mL to 120 mL.
Surgical Procedure
The width, length, and depth of the axillary area to be filled were measured to define the volume, the dimensions, and the number of implants to be used.
As the procedure may be performed under local anesthesia, the area was marked and was then infiltrated with saline solution, epinephrine, and xylocaine.
The implants were inserted through the scar from the breast reconstruction, superimposing the dissection plane on the remaining chest muscles or on the rib cage, with the aim being to have the thickest possible layer of subcutaneous tissue over the implant.
The subcutaneous detachment was 0.5 cm to 1 cm larger than the size of the implant.
The volume of the implant was determined intraoperatively, using casts or expanders.
Sutures were placed in 2 or 3 planes, and a drain was placed for 24 to 48 hours.
RESULTS
In the immediate postoperative period, one patient developed a hematoma, which resolved after needle aspiration.
The postoperative follow-up period ranged from 6 months to 8 years; there were no complaints of capsular contracture (Figure 1).
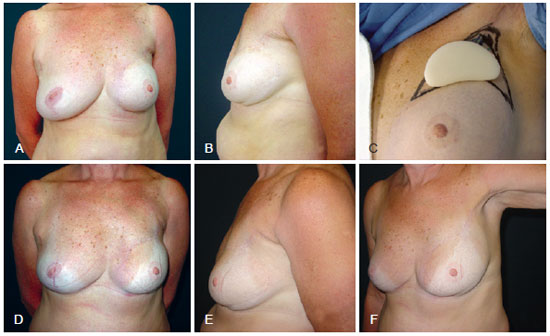
Figure 1 - In A and B, preoperative appearance of semilunar silicone supplementary implants. In C, preoperative planning and measurements. In D, E, and F, postoperative appearance, 3 years after placement of a 60-mL semilunar silicone supplementary implant.
All patients noted functional improvement when raising the arm and expressed satisfaction with the possibility of wearing lighter, more revealing clothing.
One implant was able to fill a 2 cm depression.
In the patient for whom 2 implants were used, the second one served as a complement of the projection and was inserted 3 months after the first implant, using the same technical principles.
DISCUSSION
Although the results of well-performed breast reconstructions bring great satisfaction to patients, many complain of the loss of the anterior axillary wall and of the depression in the infraclavicular region, which become visible in lighter clothing. This region should also be corrected as part of reconstruction procedures.
Adipose flaps have frequently been used, particularly for the correction of infraclavicular depression5. However, this procedure requires a donor area with sufficient adipose tissue, and several procedures may be needed to complete the filling of the depression when it is impossible to predict the percentage of integration of the flaps. Moreover, liponecrosis may occur and may have a suspicious appearance during routine mammography1,2,6.
Placement of the AlloDerm membrane or Sculptra (poly- L-lactic acid) has been suggested7-12, but these products do not allow for large volumes (they average 2 to 3 mm) and they can be expensive8,10.
The depression is usually pronounced in the anterior axillary wall deformity, requiring a larger filling volume. Local adhesions may hinder or prevent adipose tissue injection.
Repair of these deformities by using a semilunar-shaped silicone gel implant facilitates immediate reconstruction that is predictable in its final volume because it is possible to use casts both preoperatively and intraoperatively. In cases where a larger projection is needed, more than one implant may be used in the same place, during the same surgical procedure or at different times.
In the infraclavicular position, the implants may be noticeable because of the limited subcutaneous tissue left by the mastectomy13. However, in the anterior axillary wall, the result is satisfactory because the subcutaneous tissue is thicker and the localization of the implant is deeper, usually over the pectoralis minor muscle or the rib cage.
This procedure may be performed under local or general anesthesia, and does not interfere with management of the breast disease.
Moreover, this procedure offers aesthetic, social, and functional advantages because it improves the appearance, enables patients to wear clothing that is more appropriate in warm weather, and allows for better movement of the arms.
CONCLUSIONS
Insertion of semilunar silicone supplementary implants in breast reconstruction is a simple method, easy to execute, and of predictable outcome, that may be performed in a single surgical procedure. The volume may be evaluated preoperatively or intraoperatively. The implants may be exchanged, added, or removed as needed.
The aesthetical and functional benefits provided by semilunar silicone supplementary implants make them an important part of breast reconstructions after mastectomy.
REFERENCES
1. Chan CW, McCulley SJ, Macmillan RD. Autologous fat transfer: a review of the literature with a focus on breast cancer surgery. J Plast Reconstr Aesthet Surg. 2008;61(12):1438-48.
2. Spear SL, Wilson HB, Lockwood MD. Fat injection to correct contour deformities in the reconstructed breast. Plast Reconstr Surg. 2005;116(5):1300-5.
3. Hodgkinson DJ. The management of anterior chest wall deformity in patients presenting for breast augmentation. Plast Reconstr Surg. 2002;109(5):1714-23.
4. Gatti JE. Poland's deformity reconstruction with a customized, extrasoft silicone prosthesis. Ann Plast Surg. 1997;39(2):122-30.
5. Rigotti G, Marchi A, Stringhini P, Baroni G, Galiè M, Molino AM, et al. Determining the oncological risk of autologous lipoaspirate grafting for post-mastectomy breast reconstruction. Aesthetic Plast Surg. 2010;34(4):475-80.
6. Hyakusoku H, Ogawa R, Ono S, Ishii N, Hirakawa K. Complications after autologous fat injection to the breast. Plast Reconstr Surg. 2009;123(1):360-70.
7. Newman MI, Samson MC, Berho M. AlloDerm in breast reconstruction: 2 years later. Plast Reconstr Surg. 2009;123(6):205e-6e.
8. Uflacker AB, Janis JE. The use of acellular dermal matrix in the correction of visible parasternal deformities after breast reconstruction. Plast Reconstr Surg. 2010;126(1):34e-6e.
9. Losken A. Early results using sterilized acellular human dermis (Neoform) in post-mastectomy tissue expander breast reconstruction. Plast Reconstr Surg. 2009;123(6):1654-8.
10. Bindingnavele V, Gaon M, Ota KS, Kulber DA, Lee DJ. Use of acellular cadaveric dermis and tissue expansion in postmastectomy breast reconstruction. J Plast Reconstr Aesthet Surg. 2007;60(11):1214-8.
11. Maxwell GP, Gabriel A. Use of the acellular dermal matrix in revisionary aesthetic breast surgery. Aesthet Surg J. 2009;29(6):485-93.
12. Schulman MR, Lipper J, Skolnik RA. Correction of chest wall deformity after implant-based breast reconstruction using poly-L-lactic acid (Sculptra). Breast J. 2008;14(1):92-6.
13. Marks MW, Argenta LC, Izenberg PH, Mes LG. Management of the chest-wall deformity in male patients with Poland's syndrome. Plast Reconstr Surg. 1991;87(4):674-81.
1. Doctor and Master in Plastic Surgery at the Universidade Federal do Rio de Janeiro (Federal University of Rio de Janeiro) - UFRJ, full member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery) - SBCP, Rio de Janeiro, RJ, Brazil.
2. Plastic Surgeon, full member of SBCP, Rio de Janeiro, RJ, Brazil.
3. Doctor, Adjunct Professor of Plastic Surgery at UFRJ, full member of SBCP, Rio de Janeiro, RJ, Brazil.
4. Resident in Plastic Surgery at UFRJ, associate member of the SBCP, Rio de Janeiro, RJ, Brazil.
5. Resident Physician in Plastic Surgery at UFRJ, member in training of the SBCP, Rio de Janeiro, RJ, Brazil.
6. Doctor, Full Professor in Plastic Surgery at UFRJ, full member of SBCP, Rio de Janeiro, RJ, Brazil.
Correspondence to:
João Medeiros Tavares Filho
Rua Buenos Aires, 255 - Centro
Petrópolis, RJ, Brazil - CEP 22438-033
E-mail: jmedeiro@compuland.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: December 2, 2011
Article accepted: April 11, 2012
Study conducted at the Hospital Universitário da Universidade Federal do Rio de Janeiro (University Hospital of the Federal University of Rio de Janeiro), Rio de Janeiro, RJ, Brazil.
Study awarded with the Georges Ariê prize during the 48th Brazilian Congress of Plastic Surgery, in Goiânia, GO, Brazil, from 11 to 15 November 2011.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter