

Original Article - Year 2012 - Volume 27 -
The best plane for breast implantation in patients with hypomastia: submuscular or subglandular?
Subpeitoral ou subglandular: qual é a melhor localização do implante para pacientes com hipomastia?
ABSTRACT
BACKGROUND: Breast augmentation is one of the most common plastic surgery procedures in Brazil and worldwide. There are 2 main locations for the implant: the subpectoral or submuscular plane and subglandular plane. The objective of the current study was to indicate the efficacy of the use of the subpectoral plane in cases of hypomastia.
METHODS: Sixteen patients underwent breast augmentation between 2008 and 2011; the submuscular and subglandular planes were used in 9 and 7 patients, respectively. Myotomy of the pectoralis major muscle was performed in all cases where the submuscular plane was used.
RESULTS: The pre- and postoperative aspects of 5 cases of patients undergoing breast augmentation are presented. Better results were obtained using the submuscular plane for patients with severe hypomastia. Myotomy of the pectoralis proved critical to the success of the surgery, because it provided the submuscular pocket required to house the breast implant without subjecting it to the pressure caused by muscle contraction.
CONCLUSIONS: The proper use of the submuscular plane in patients with hypomastia is safe, facilitates cancer screening, does not alter muscle function, protects the breast parenchyma, and ensures more natural and long-term results.
Keywords: Mammaplasty. Breast/surgery. Breast implantation.
RESUMO
INTRODUÇÃO: A mamoplastia de aumento é um dos procedimentos mais realizados em cirurgia plástica no Brasil e no mundo. Existem duas localizações principais para o implante: o plano subpeitoral ou submuscular e o plano subglandular. O objetivo deste trabalho é defender o uso do plano subpeitoral em casos de hipomastia.
MÉTODO: Dezesseis pacientes foram submetidas a aumento da mama entre 2008 e 2011. Utilizou-se o plano submuscular em 9 pacientes e o plano subglandular em 7. Miotomia do músculo grande peitoral foi realizada em todos os casos de localização submuscular.
RESULTADOS: Foram selecionados 5 casos de pré e pós-operatório de pacientes submetidas a mamoplastia de aumento. Verificaram-se melhores resultados utilizando-se o plano submuscular para as pacientes com hipomastia acentuada. A miotomia do músculo peitoral provou ser fundamental para o sucesso da cirurgia, pois conferiu à loja submuscular o espaço necessário para abrigar o implante mamário, sem submetê-lo à pressão causada pela contração do músculo.
CONCLUSÕES: O uso adequado do plano submuscular em pacientes com hipomastia é seguro, facilita o rastreamento de câncer de mama, não altera a função muscular, protege o parênquima mamário e garante resultados mais naturais e duradouros.
Palavras-chave: Mamoplastia. Mama/cirurgia. Implante mamário.
The creation of silicone implants in 1961 by Cronin & Gerow1 in association with the Dow Corning Corporation and the first such surgery performed in 1962 led to breast augmentation being one of the most frequently performed and studied procedures by plastic surgeons in Brazil and worldwide.
There are basically 2 main planes for the location of the breast implant: the submuscular and subglandular planes. The use of submuscular space was first described in 1967 by Griffiths2. Other authors such as Dempsey & Latham3 in 1968, Regnault4 in 1977, and Mahler et al.5, and Mahler & Hauben6 in 1982 were also pioneers of this technique. The works of Mahler et al.5 and Mahler & Hauben6 were important in establishing the myotomy technique of the pectoralis major muscle - a fundamental procedure for successful operations using the submuscular plane.
Although submuscular augmentation mammoplasty with myotomy of the pectoralis major muscle was described more than 30 years ago, knowledge on the procedure remains somewhat poorly disseminated because of the lack of published literature and absence of a detailed description of the technique.
In the present study, we aimed to demonstrate the benefits of using the submuscular plane in patients with hypomastia, including the technical details of this access route and myotomy of the pectoralis major muscle as well as the positive and negative aspects of both implantation locations.
METHODS
This study retrospectively analyzed the medical records of 16 female patients who underwent breast implantation between February 2008 and February 2011. High-profile round polyurethane implants were used, and volume ranged between 175 and 325 cm3. Of these, 10 patients had hypomastia. The submuscular and subglandular planes were used in 9 and 7 patients, respectively. The average age of the patients at the time of surgery was 27.5 years.
Submuscular Breast Augmentation Technique
Before making the surgical markings (Figure 1), the breasts, chest, and spine were inspected to identify asymmetries, different heights of the mammary groove, and protruding ribs7,8. The sternal midline and probable area of detachment were highlighted. Inferior dissection was performed just below the mammary fold to better accommodate the implant. The incision was located 1 cm below the groove, and was extended by 4.5 cm-2.0 cm medially and 2.5 cm laterally - with the projection of the nipple as the center. A periareolar incision was possible in patients with an areola diameter greater than 4.5 cm. However, access to the submuscular space was accomplished via the lateral side of the pectoralis major muscle. The upper limit of the myotomy was a horizontal line passing through the nipple, forming a right angle with the sternum. The lower limit was the insertion end of the pectoralis major on the fifth rib or, less frequently, the sixth rib, depending on the relative positioning of the breast to the thorax (Figure 1).
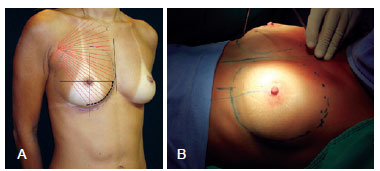
Figure 1 - In A and B, marking of the breast, with emphasis on the edge of the myotomy of the pectoralis major muscle.
After incision, dissection was performed under the gland, while attempting to locate the side and bottom edge of the pectoralis major muscle (Figure 2).

Figure 2 - Incision and early dissection.
The boundaries of the pectoralis major muscle were visualized, and submuscular dissection was initiated after opening the lower insertion of the muscle on the fifth rib. It is important that this opening is made at this location and avoids the intercostal space. The pectoralis major muscle was carefully lifted by means of digital maneuvering (Figure 3).
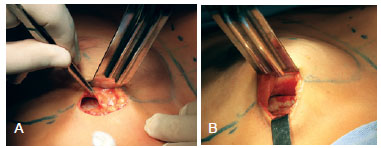
Figure 3 - In A and B, lower insertion opening of the pectoralis major and early submuscular detachment.
A spacer with optical fiber was then introduced to better visualize the plane. Myotomy of the pectoralis major was initiated with an electric scalpel, followed by its insertion on top of the rib to the sternum (Figure 4).
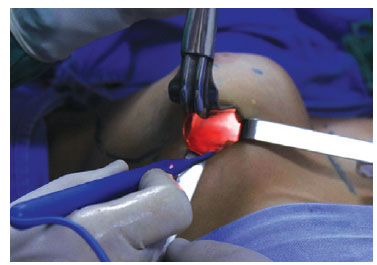
Figure 4 - Main surgical time: myotomy of the pectoralis major muscle.
The pectoralis major muscle fibers were sectioned up to where subcutaneous fat was located adjacent to the muscle. The contrast between the red and yellow colors facilitated the demarcation of the end of the myotomy (Figure 5).
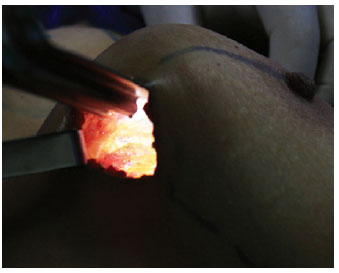
Figure 5 - End of myotomy of the pectoralis major muscle, allowing visualization of the inferomedial insertion of the fully released muscle.
Moreover, the placement of molds and observation of the breast made it possible to check if there were still fibers or beams that would affect the shape of the breast. A digital maneuver can be performed to search for such fiber remnants (Figure 6).

Figure 6 - Placing of molds and digital verification of myotomy of the pectoralis major muscle.
With the mold of the desired size, the last detachment adjustments were performed, attempting to inferiorly overcome the mammary fold to better accommodate the implant (Figure 7).

Figure 7 - Final displacement settings.
Vacuum drainage of the implant pocket is required in order to avoid the occurrence of seroma and other complications9,10 (Figure 8).

Figure 8 - Drainage by suction, closed system.
Dressing was performed with Tensorplast® elastic bandages.
The patients were discharged the day after surgery and were administered analgesics and antibiotics for 6 days.
Usually, on the 4th day after surgery, the patient returned to the clinic for the removal of the surgical tube and elastic bandage. A surgical bra is indicated thereafter.
RESULTS
Five cases of pre- and postoperative patients undergoing breast augmentation were selected and are described below.
Case 1 - A 21-year-old patient presenting with hypomastia underwent breast augmentation performed via the mammary groove through the submuscular plane with highprofile round polyurethane 215 cm3 implants (Figure 9).
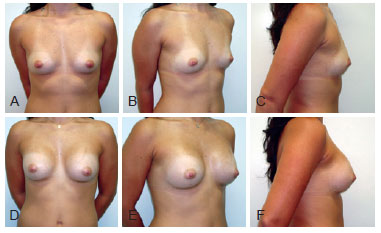
Figure 9 - Case 1. In A, B, and C, preoperative aspects in frontal, right oblique, and right profile views, respectively. In D, E, and F, 6-month postoperative aspects in frontal, right oblique, and right profile views, respectively.
Case 2 - A 29-year-old patient presenting with hypomastia underwent breast augmentation via the mammary groove through the submuscular plane, with high-profile round polyurethane 285 cm3 implants (Figure 10).
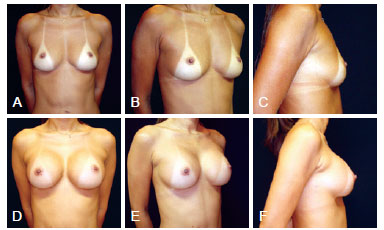
Figure 10 - Case 2. In A, B, and C, preoperative aspects in frontal, right oblique, and right profile views, respectively. In D, E, and F, 2-month postoperative aspects in frontal, right oblique, and right profile views, respectively.
Case 3 - A 22-year-old patient presenting with hypomastia underwent breast augmentation via the mammary groove through the submuscular plane with high-profile round polyurethane 255 cm3 implants (Figure 11).
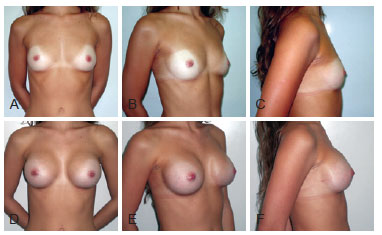
Figure 11 - Case 3. In A, B, and C, preoperative aspects in frontal, right oblique, and right profile views, respectively. In D, E, and F, 10-month postoperative aspects in frontal, right oblique, and right profile views, respectively.
Case 4 - A 33-year-old patient presenting with hypomastia underwent breast augmentation via the submuscular plane and liposuction of the anterior axillary region. Figure 12 shows the limit of myotomy of the pectoralis major muscle. High-profile round polyurethane 235 cm3 implants were used (Figure 13).

Figure 12 - Marking of the breast and the end of the myotomy of the pectoralis major muscle.
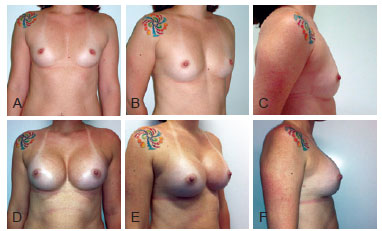
Figure 13 - Case 4. In A, B, and C, preoperative aspects in frontal, right oblique, and right profile views, respectively. In D, E, and F, 3-month postoperative aspects in frontal, right oblique, and right profile views, respectively.
Case 5 - A 49-year-old nulliparous patient presenting with mild hypomastia and hypertrophy of the nipples underwent breast augmentation via the subglandular plane. High-profile round polyurethane 255 cm3 implants were placed, and nipple reduction was performed (Figure 14).
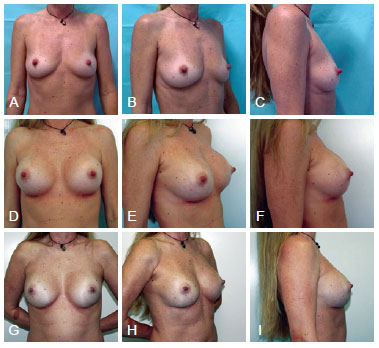
Figure 14 - Case 5. In A, B, and C, preoperative aspects in frontal, right oblique, and right profile views, respectively. In D, E, and F, 6-week postoperative aspects in frontal, right oblique, and right profile views, respectively. In G, H, and I, 2-year 9-month postoperative aspects in frontal, right oblique, and right profile views, respectively.
DISCUSSION
The breasts are mainly vascularized by the internal thoracic artery and branches of the axillary artery. The penetrating branches that cross the first 4 intercostal spaces leave the thoracic artery and continue penetrating the pectoralis major to reach the posterior surface of the breasts. The axillary artery branches into the lateral thoracic artery, which runs along the lateral border of the pectoralis minor muscle, which in turn, issues new branches called the lateral mammary branches. Therefore, studying the anatomy of the retropectoral region and vasculature of the breasts reveal that the submuscular plane is a less aggressive approach because it promotes less devascularization of the mammary gland. This is because the penetrating vessels are preserved when performing the detachment under the pectoralis major muscle, thereby reducing the atrophy that occurs in the mammary parenchyma over time. When using the subglandular plane, the implant directly compresses the breast, which - coupled with the effect of devascularization - further contributes to this atrophy11 (Figure 15).
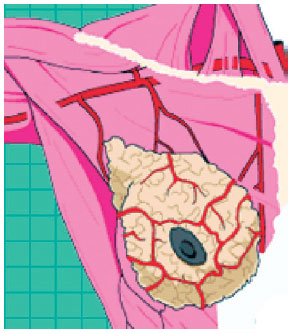
Figure 15 - Vasculature of the breast.
The use of the submuscular plane in patients with hypomastia yields good results and provides extra protection for the implant. This minimizes the risk of visible and palpable irregularities and promotes a smooth transition of the chest with the upper pole of the breast. The pectoralis major should be sectioned at its inferomedial portion whenever the submuscular plane is used (Figure 16). This myotomy is critical for preventing the implant from moving or sustaining pressure at the time of muscle contraction.
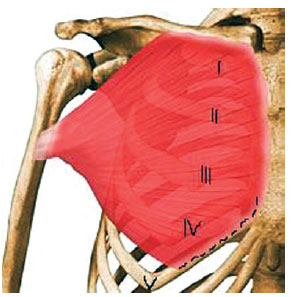
Figure 16 - Anatomy of the pectoralis major and its insertions on the clavicle, sternum, ribs, and humerus. The location of the myotomy is indicated by a dotted line. I to V: ribs.
A prospective study in 2004 with 37 patients subjected to submuscular augmentation examined breast sensitivity, the contraction force of the pectoralis major muscle, and self-esteem at 3 and 6 months postoperatively12. Sensitivity to pressure and vibration changed at 3 months with normalization occurring at the 6-month postoperative follow-up. The flexion, extension, and adduction of the pectoralis major muscle did not change at 3 or 6 months. Similarly, no change in muscle function was noted when implants larger or smaller than 325 cm3 were compared. Finally, self-esteem increased significantly postoperatively. Therefore, it can be concluded that myotomy of the pectoral muscle to the extent shown does not alter the muscle function or impair the quality of life of the patient.
Another important point directly related to the anatomy of the breast and strongly supported in the medical literature is the issue of screening for the detection of breast cancer. Several studies found that the placement of the implant under the pectoralis major allows better visualization and a larger amount of mammary parenchyma to be examined compared to placement of the implant at the subglandular location, regardless of breast size and type of implant13-15. Therefore, in patients with a strong family history of breast cancer, it is prudent to avoid using the subglandular plane.
Interestingly, subglandularly positioned implants appear aesthetically better in the first weeks after surgery, specifically due to the presence of surgical edema. When the edema resolves and the breast parenchyma decreases in volume, problems such as rippling and breast deformities may appear in the late postoperative period. These complications are more frequent with larger implants and when hypomastia is more pronounced. However, when using the submuscular position, the result becomes increasingly satisfactory and natural over time; this effect is best visualized 3 months postoperatively when the muscle edema has already abated.
It is possible to compare the positive evolution of the shape of the breasts in the early and late postoperative periods in cases 3 and 4.
Another positive aspect of the submuscular plane is the lower incidence of capsular contracture11. This is an important complication of breast augmentation in which there is a change in the shape of the breast that is associated with pain. Treatment of patients exhibiting capsular contracture, visible and palpable implants, or thin mammary parenchyma is a substantial challenge. In these cases, secondary mastopexy, switching from the subglandular plane to the submuscular plane associated with capsulotomy, is perhaps the only alternative16. These patients may be deprived of more favorable results if the submuscular plane is used for the initial surgery.
In case 5 presented above, the subglandular plane was chosen despite the desire to use the submuscular plane. The decision was based on the inability of the patient to comply with the requested period of rest due to work activities. Since this was a nulliparous patient with mild hypomastia with firm and good-quality skin, the subglandular plane could be used without causing problems. Two years and 9 months postoperatively, there was minimal loss in the quality of results obtained compared to that observed in the early postoperative period of 45 days. Poorer skin quality and more pronounced hypomastia result in more substantial losses in the quality of results obtained.
In the period after submuscular mammoplasty augmentation, it is important to rest the arms for 30 days; lifting the arms, lifting weights, driving, and sleeping in lateral and ventral positions should be avoided. After 1 month, these activities are allowed, but more intense exercise such as weight lifting and gymnastics can be resumed only after 3 months.
In cases presenting with hypomastia, ptosis, and moderate hypertrophy of the pectoralis major, the choice of the location of the implant is a challenge for the plastic surgeon. This type of breast is common in patients with muscle dysmorphia and those who use anabolic steroids, which explains the breast atrophy and muscle hypertrophy. Choosing the submuscular plane may produce an unaesthetic result with a double breast contour strongly marked by the edge of the hypertrophied pectoralis major17. On the other hand, if the subglandular plane is chosen, a favorable outcome would be obtained in the first months. However, large problems could subsequently manifest, including the possibility of capsular contracture and deformity of the breast implant due to the large correction of ptosis associated with very thin mammary coverage. Tebbets8,18,19 describes a stratagem for such cases that he terms the "dual plane." In particular, this dual plane involves a small displacement of the lower part of the breast over the muscle, causing it to retract slightly further upwards, leaving the implant having better coverage by the breast to fill the lower pole, and thus, better treat ptosis. This does not involve a new location for the implant, but is a maneuver that enables better adaptation of the implant to the classic submuscular plane. However, a double plane remains since the implant is not fully covered by the muscle, because of the myotomy of the pectoral major. Of course, in cases of severe ptosis, mastopexy to lift the areolas should be considered, and the submuscular plane is recommended as it results in less interference with the vasculature of the areolas.
The use of the full submuscular plane, which involves the detachment of even the serratus muscle such that the implant is completely covered by the musculature, is limited in post-mastectomy reconstruction. Using this plane in cases of hypomastia is anti-anatomical and produces disastrous results because of greater displacement of the implant.
In 2003, Graf et al.20 described the use of the subfascial plane. This technique may have advantages over the use of the subglandular plane but is unable to produce the benefits that the submuscular plane offers to patients with hypomastia.
The plastic surgeon should choose the location of the implant taking into account technical criteria proven by the medical literature and associating them with the patient's profile21. It is important to master the implant placement in both planes in order to have a complete surgical capability to optimally treat all cases.
CONCLUSIONS
The submuscular plane with myotomy of the pectoralis major should be the procedure of choice for most patients with hypomastia, because it produces more natural, aesthetic, and long-term results. Moreover, it produces fewer changes to the breast parenchyma, results in a lower incidence of capsular contracture, and facilitates the diagnosis of breast cancer.
REFERENCES
1. Cronin TD, Gerow RM. Augmentation mammaplasty: a new "natural feel" prosthesis. In: Translations of the Third International Congress of Plastic Surgery. Amsterdam: Excerpta Medica; 1964. p. 41-9.
2. Griffiths CO. The submuscular implant in augmentation mammaplasty. In: Translations of the Fourth International Congress of Plastic Surgery. Amsterdam: Excerpta Medica; 1967. p. 1009.
3. Dempsey WC, Latham WD. Subpectoral implants in augmentation mammaplasty. Preliminary report. Plast Reconstr Surg. 1968;42(6):515-21.
4. Regnault P. Partially submuscular breast augmentation. Plast Reconstr Surg. 1977;59(1):72-6.
5. Mahler D, Ben-Yakar J, Hauben DJ. The retropectoral route for breast augmentation. Aesthetic Plast Surg. 1982;6(4):237-42.
6. Mahler D, Hauben DJ. Retromammary versus retropectoral breast augmentation: a comparative study. Ann Plast Surg. 1982;8(5):370-4.
7. Rohrich RJ, Hartley W, Brown S. Incidence of breast and chest wall asymmetry in breast augmentation: a retrospective analysis of 100 patients. Plast Reconstr Surg. 2006;118(7 Suppl):7S-13S.
8. Tebbetts JB. Dual plane breast augmentation: optimizing implant-softtissue relationships in a wide range of breast types. Plast Reconstr Surg. 2006;118(7 Suppl):81S-98S.
9. Schreml S, Heine N, Eisenmann-Klein M, Prantl L. Bacterial colonization is of major relevance for high-grade capsular contracture after augmentation mammaplasty. Ann Plast Surg. 2007;59(2):126-30.
10. Handel N, Cordray T, Gutierrez J, Jensen JA. A long-term study of outcomes, complications, and patient satisfaction with breast implants. Plast Reconstr Surg. 2006;117(3):757-67.
11. Spear SL, Bulan EJ, Venturi ML. Breast augmentation. Plast Reconstr Surg. 2004;114(5):73E-81E.
12. Banbury J, Yetman R, Lucas A, Papay F, Graves K, Zins JE. Prospective analysis of the outcome of subpectoral breast augmentation: sensory changes, muscle function, and body image. Plast Reconstr Surg. 2004;113(2):701-7.
13. McCarthy CM, Pusic AL, Disa JJ, Cordeiro PG, Cody HS 3rd, Mehrara B. Breast cancer in the previously augmented breast. Plast Reconstr Surg. 2007;119(1):49-58.
14. Jakubietz MG, Janis JE, Jakubietz RG, Rohrich RJ. Breast augmentation: cancer concerns and mammography - a literature review. Plast Reconstr Surg. 2004;113(7):117-22.
15. Deapen DM, Hirsch EM, Brody GS. Cancer risk among Los Angeles women with cosmetic breast implants. Plast Reconstr Surg. 2007;119(7):1987-92.
16. Handel N. Secondary mastopexy in the augmented patient: a recipe for disaster. Plast Reconstr Surg. 2006;118(7 Suppl):152S-63S.
17. Médard de Chardon V, Balaguer T, Chignon-Sicard B, Lebreton E. Double breast contour in primary aesthetic breast augmentation: incidence, prevention and treatment. Ann Plast Surg. 2010;64(4):390-6.
18. Tebbetts JB. Dual plane breast augmentation: optimizing implant-softtissue relationships in a wide range of breast types. Plast Reconstr Surg. 2001;107(5):1255-72.
19. Tebbetts JB, Adams WP. Five critical decisions in breast augmentation using five measurements in 5 minutes: the high five decision support process. Plast Reconstr Surg. 2006;118(7 Suppl):35S-45S.
20. Graf RM, Bernardes A, Rippel R, Araujo LR, Damasio RC, Auersvald A. Subfascial breast implant: a new procedure. Plast Reconstr Surg. 2003;111(2):904-8.
21. Tebbetts JB. Does fascia provide additional, meaningful coverage over a breast implant? Plast Reconstr Surg. 2004;113(2):777-9.
Plastic Surgeon, member of the Brazilian Society of Plastic Surgery, Rio de Janeiro, RJ, Brazil.
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: November 7, 2011
Article accepted: August 7, 2012
Correspondence to:
Gabriel de Castro Zeitoune
Rua Barão da Torre, 313 - ap.103 - Ipanema
Rio de Janeiro, RJ, Brazil - CEP 22411-001
E-mail: dr.gabrielzeitoune@gmail.com
This study was performed at the private practice of the author, Rio de Janeiro, RJ, Brazil.
Work presented, and the author received promotion to Full Member of the Sociedade Brasileira de Cirurgia Plástica/Brazilian Society of Plastic Surgery, at the 48th Brazilian Congress of Plastic Surgery, Goiania, GO, Brazil, 2011.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter