

Original Article - Year 2012 - Volume 27 -
Breast augmentation through abdominoplasty
Mastoplastia de aumento através da abdominoplastia
ABSTRACT
BACKGROUND: This study establishes a technique for dissection of the retroglandular space through abdominoplasty by using a lighted retractor for the introduction of silicone gel breast implants.
METHODS: A retrospective study was carried out for 44 patients with abdominal flaccidity and hypomastia who underwent breast augmentation through a single-stage abdominoplasty between September 2001 and April 2012.
RESULTS: This method enabled improvement of the abdominal contour and breast augmentation through the same incision. The complications observed affected the abdominal area (hematoma, seroma, dehiscence, and hypertrophic scarring) and the breast (capsular contracture and infection).
CONCLUSIONS: Breast augmentation through abdominoplasty does not cause scars on the breast or armpit and is a safe and reproducible procedure with a short learning curve. Moreover, it provides satisfactory and long-lasting results.
Keywords: Abdomen/surgery. Plastic surgery/methods. Breast implantation. Breast implants. Mammaplasty.
RESUMO
INTRODUÇÃO: Este trabalho demonstra a técnica de dissecção de espaço retroglandular através da abdominoplastia, com visualização de fibra óptica para inclusão de implantes mamários de silicone gel.
MÉTODO: Foram avaliadas, retrospectivamente, 44 pacientes portadoras de flacidez abdominal e hipomastia, submetidas a mastoplastia de aumento através da abdominoplastia em um só estágio, durante o período de setembro de 2001 a abril de 2012.
RESULTADOS: A técnica utilizada possibilitou melhora do contorno abdominal e aumento do volume mamário pela mesma incisão. As complicações ocorreram na área abdominal (hematoma, seroma, deiscência e cicatriz hipertrófica) e na região mamária (contratura capsular e infecção).
CONCLUSÕES: A técnica de mastoplastia de aumento por via abdominal evita cicatrizes nas mamas ou axilas, é segura, reprodutível, com curva de aprendizado curta, e resultados satisfatórios e duradouros.
Palavras-chave: Abdome/cirurgia. Cirurgia plástica/métodos. Implante mamário. Implantes de mama. Mamoplastia.
Few studies have been published on breast augmentation through abdominoplasty. By manual dilation, Hinderer1, Planas2, Barrett & Kelly3, and Paoliello4 created routes for the introduction of breast implants using the incision made for abdominal dermolipectomy. Wallach5 and Rinker & Jack6 used lighted retractors to create subcutaneous routes and allow detachment of the subglandular and retromuscular layers, in order to introduce silicone implants through the abdomen and avoid scars on the breast or armpit.
Because of diversities in terms of form, quality, and quantity of the glandular tissue and skin of the breast as well as the presence of a flaccid abdomen, there is a frequent demand for combined plastic surgeries. Candidates for breast augmentation through the abdomen are, in particular, women diagnosed with hypomastia and abdominal flaccidity.
Patients opting for plastic surgery request larger breasts that are well positioned and symmetrical with a natural shape as well as a good aesthetic appearance of the abdomen.
Single-stage combined surgery enables the surgeon to obtain proper shape, symmetry, and breast volume with localized abdominal scars in patients showing breast hypertrophy without ptosis or with pseudoptosis and a flaccid abdomen. This is achieved by the introduction of implants through the abdominoplasty incision without causing scars in the thoracic region and involves an increase in the operative time.
METHODS
Between September 2001 and April 2012, 44 patients were selected for breast augmentation through abdominoplasty. The patients were previously diagnosed with hypomastia, without ptosis or with pseudoptosis (Regnault classification7), and type V abdomen (classification of Bozola & Psillakis8).
The age of the patients varied from 20 to 56 years, with an average age of 35.7 years. The mean body mass index was 23.4 kg/m2.
Before undergoing surgery, most of the women had experienced 2 or more pregnancies and presented a physical status of ASA I (91%) or ASA II (9%) according to the classification of the American Society of Anesthesiologists. Five patients were smokers, 2 were hypertensive, and 1 was diagnosed with diabetes mellitus.
Surgical Marking
With the patient in a sitting position, a curved line was drawn towards the abdominal skin fold. Then, with the patient in the supine position and depending on the skin excess in the pubic area, a transversal line was drawn 7 cm above the vulvar commissure in the direction of the inguinal fossa, almost until the iliac spines.
Breasts and mammary fold contours were defined, and starting from the ribs, 2 routes of 6 cm in width were created towards the areolas (Figure 1).

Figure 1 - Preoperative marking.
Surgical Procedure
With the patient anesthetized and in dorsal horizontal decubitus, antisepsis of the previously marked surgical fields was performed with chlorhexidine detergent solution followed by alcoholic chlorhexidine. A low transversal incision was carried out based on the marks previously defined. The subcutaneous fat layer was detached in the direction of the xiphoid process and ribs with the aid of an electrical scalpel. The umbilicus was preserved.
A route of approximately 6 cm width was extended towards the central breast, in the supra-aponeurotic plane. The retroglandular space was detached with an electric scalpel connected to a protractor; the procedure was performed under direct vision using a long lighted retractor (Figure 2). This enabled good visualization of the area and efficient dissection (Figure 3).
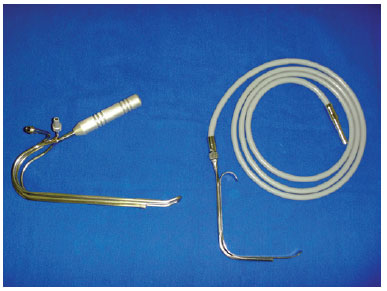
Figure 2 - Long retractor and universal lighted retractor.
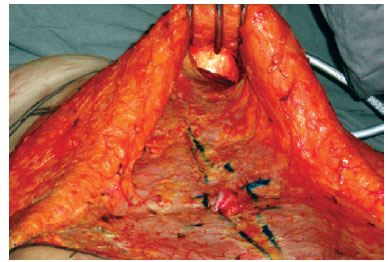
Figure 3 - Subcutaneous route and dissection of the retroglandular space.
After creation of the anatomical space and once hemostasis was achieved, the breast implant was introduced and properly positioned. The same procedure was performed for the contralateral breast.
The routes were closed with single 2.0 nylon or 2.0 polyglactin sutures, by moving the flap near the aponeurosis of the rectus abdominis, on average 1 cm below the inframammary fold (Figure 4).
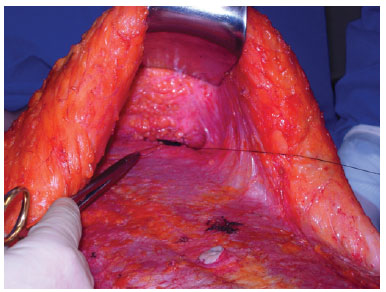
Figure 4 - Suture of the subcutaneous route.
Diastasis recti was corrected with longitudinal plication of the aponeurosis between the xiphoid process and the umbilicus until the pubis by using 2.0 nylon thread or 2.0 polyglactin suture. The next step was to fix the umbilicus in the aponeurosis with 3.0 nylon thread or 3.0 poliglecaprone sutures.
With the patient in a bent position, we pulled the flap and resected the excess skin. After hemostasis, the flap was sutured in the aponeurosis with 2.0 polyglactin or 2.0 nylon thread.
Omphaloplasty was performed through a small "V"-shaped incision in the middle of the flap, in an area that corresponded to the iliac crests. The fat was then drained and the umbilicus sutured with 3.0 and 4.0 poliglecaprone thread.
Finally, a 4.2-mm drainage tube with suction was introduced in the abdomen and fixed to the pubic skin with 3.0 nylon thread. To close the abdomen, 3.0 poliglecaprone or 3.0 nylon thread was used, whereas for the subcutaneous tissue and skin preparation, 4.0 poliglecaprone thread was employed.
RESULTS
Over the 11 years of our study period, breast augmentations through abdominoplasty were performed for 44 patients who were diagnosed with hypomastia, without ptosis or with pseudoptosis, and a flaccid type V abdomen.
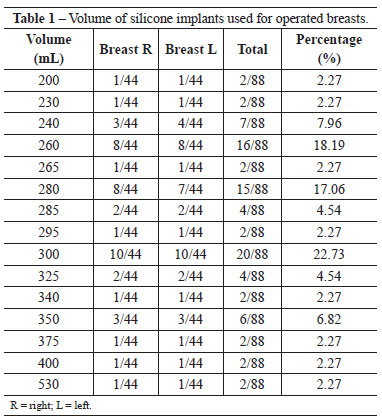
The breast implants introduced were round and had a textured surface. They were of high or ultra-high profile and contained cohesive gel silicone. The minimum volume of gel silicone was 200 mL, and the maximum volume was 530 mL, with an average of 290 mL (Table 1). The dry weight of the abdominal insert varied from 290 g to 2160 g (average, 680 g).
General anesthesia was used in 36% of patients, and spinal anesthesia was used in 64% of patients. Combined liposuction was performed in 15 patients. The average operative time was 3 hours and 22 minutes. However, surgery combined with liposuction was excluded from this value.
After surgery, breasts were properly and symmetrically positioned. They presented a natural shape, had appropriate consistency, and there were no scars on the breast or armpit (Figures 5 to 8).
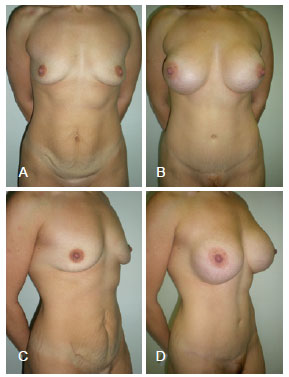
Figure 5 - A 30-year-old patient. In A and C, the preoperative aspect is shown in the frontal and lateral profiles, respectively. In B and D, the results 2 years after breast augmentation through abdominoplasty with breast implants of 350 mL are shown in the frontal and lateral profiles, respectively.

Figure 6 - A 34-year-old patient. In A and C, the preoperative aspect is shown in the frontal and lateral profiles, respectively. In B and D, the results 2 months after breast augmentation through abdominoplasty with breast implants of 350 mL are shown in the frontal and lateral profiles, respectively.

Figure 7 - A 20-year-old patient. In A and C, the preoperative aspect is shown in the frontal and lateral profiles, respectively. In B and D, the results 4 years after breast augmentation through abdominoplasty with breast implants of 240 mL are shown in the frontal and lateral profiles, respectively.
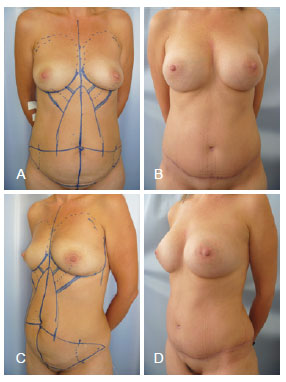
Figure 8 - A 46-year-old patient. In A and C, the preoperative aspect is shown in the frontal and lateral profiles, respectively. In B and D, the results 4 years after breast augmentation through abdominoplasty with breasts implants of 265 mL are shown in the frontal and lateral profiles, respectively.
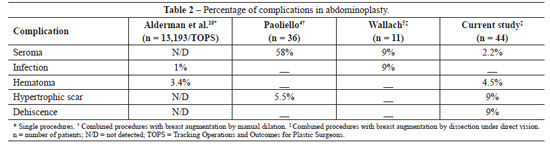
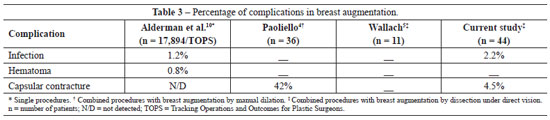
Fourteen complications were observed in 44 patients (Tables 2 and 3). In the abdomen, we detected 1 case of seroma, 2 cases of hematomas (which did not require any surgical revision), 4 cases of small dehiscences, and 4 cases of hypertrophic scars. Two women developed Baker II unilateral capsular contracture9, and 1 case of breast infection was detected.
A small surgical wound dehiscence in the suprapubic region was detected in 2 patients who were smokers and in 1 patient diagnosed with diabetes mellitus. These lesions were treated by debridement and resutured under local anesthesia.
Therapeutic treatment against infection was prescribed for the patient with unilateral breast infection. However, it was necessary to introduce a new silicone implant with a second surgery in this patient.
The hospitalization time was 24 hours.
DISCUSSION
Breast augmentation increases hypotrophic breast tissue and confers an aesthetic shape. A long lighted retractor is required to introduce breast implants through abdominoplasty. This instrument facilitates the creation of access routes, increases the retroglandular space, and enables proper hemostasis under direct vision. The routes created are similar to those generated for breast reconstruction with an abdominal rectus muscle flap.
The use of silicone gel implants to increase breast size through the abdomen is highly recommended in patients who have already been pregnant and are without ptosis or with hypertrophic breast and pseudoptosis, as indicated for classical abdominoplasty.
This procedure is contraindicated for patients with breast ptosis (Regnault grade I, II, and III7) who require mastopexy. This surgery can also be performed in lean women, although in this case, it is very important to use a long lighted retractor. The correct selection of patients is crucial for good outcomes in plastic surgery.
In 2004, Wallach5 reported a study carried out with 11 patients in whom breast implants were introduced through the abdomen via the creation of routes and anatomical spaces necessary to insert the prostheses. This procedure was carried out using a lighted retractor. After surgery, seroma and infection of the abdominal surgical wound was observed in 1 patient.
In 2006, Paoliello4 described his experience with the introduction of breast implants through the abdomen in 36 patients using manual dilation of the subcutaneous route and retroglandular space. He reported 21 cases of seroma, 7 women with capsular contracture, and 2 cases of hypertrophic scarring.
In 2009, a study published by Alderman et al.10 and included in the Tracking Operations and Outcomes for Plastic Surgeons (TOPS) database of the United States described patients who underwent abdominoplasty and breast augmentation. This confirmed the complication rates of combined procedures. No patients with deep vein thrombosis or pulmonary embolism were detected. The complication rate we observed was in agreement with the medical literature (Tables 2 and 3).
Implants of different sizes are used for asymmetry and breast hypotrophy. Classical abdominoplasty is performed according to the experience of the surgeon. Combined with liposuction, this procedure might be indicated depending on the clinical history of the patient, her needs, and the judgment of the physician.
CONCLUSIONS
Introduction of silicone gel implants through abdominoplasty is a safe and reproducible procedure with a short learning curve. It provides satisfactory and long-lasting results without causing scars on the breast or armpit, thus representing another option for the plastic surgeon.
REFERENCES
1. Hinderer UT. The dermolipectomy approach for augmentation mammaplasty. Clin Plast Surg. 1975;2(3):359-69.
2. Planas J. Introduction of breast implants through the abdominal route. Plast Reconstr Surg. 1976;57(4):434-7.
3. Barrett BM Jr, Kelly MV 2nd. Combined abdominoplasty and augmentation mammaplasty through a transverse suprapubic incision. Ann Plast Surg. 1980;4(4):286-91.
4. Paoliello HR Jr. Inclusão mamária por via abdominal. In: Stocchero IN, Tournieux AAB, eds. Atualização em cirurgia plástica estética e reconstrutiva. São Paulo: Robe; 2006. p. 703-6.
5. Wallach SG. Transabdominoplasty breast augmentation. Aesthet Surg J. 2004;24(4):373-8.
6. Rinker B, Jack JM. Subpectoral breast augmentation through the abdominoplasty incision. Ann Plast Surg. 2007;58(3):241-5.
7. Regnault P. Breast ptosis: definition and treatment. Clin Plast Surg. 1976;3(2):193-203.
8. Bozola AR, Psillakis JN. Abdominoplasty: a new concept and classification for treatment. Plast Reconstr Surg. 1988;82(6):983-93.
9. Little G, Baker JL Jr. Results of closed compression capsulotomy for treatment of contracted breast implant capsules. Plast Reconstr Surg. 1980;65(1):30-3.
10. Alderman AK, Collins ED, Streu R, Grotting JC, Sulkin AL, Neligan P, et al. Benchmarking outcomes in plastic surgery: national complication rates for abdominoplasty and breast augmentation. Plast Reconstr Surg. 2009;124(6):2127-33.
1. Plastic surgeon at the Hospital Servidor Público Municipal de São Paulo, full member of the Brazilian Society of Plastic Surgery (SBCP), São Paulo, SP, Brazil.
2. Regent of the Plastic Surgery Service of the Hospital Servidor Público Municipal de São Paulo, plastic surgeon, full member of SBCP, São Paulo, SP, Brazil.
3. Plastic surgeon at the Hospital Servidor Público Municipal de São Paulo, associate member of SBCP, São Paulo, SP, Brazil.
4. Plastic surgery resident at the Hospital Servidor Público Municipal de São Paulo, aspirant member of SBCP, São Paulo, SP, Brazil.
Correspondence to:
Roberto Sodré
Rua Antonio Alves Barril, 355 - ap. 191 - Jd. Anália Franco
São Paulo, SP, Brazil - CEP 03338-000
E-mail: roberto.sodre@uol.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: May 17, 2012
Article accepted: August 7, 2012
This study was performed at the private clinic of the principal author and Hospital Servidor Público Municipal de São Paulo, São Paulo, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter