

Original Article - Year 2012 - Volume 27 - Issue 3
Intramuscular technique in augmentation gluteoplasty
Técnica intramuscular na gluteoplastia de aumento
ABSTRACT
BACKGROUND: A harmonious gluteal region is considered an essential element in the composition of body beauty and expression of femininity. Therefore, there is growing interest, from both men and women, in the aesthetical improvement of this region. The aim of this study is to present an alternative to the published augmented gluteoplasty techniques, as well as to demonstrate the viability of this alternative as a safe and reproducible technique. Based on intramuscular placement of the prosthesis, the technique uses simplified limits of dissection with reference to the fixed anatomical structures (bones) of the gluteal region in order to construct the implant pocket.
METHODS: From 2001 to 2011, 18 patients with ages ranging from 25 years to 50 years underwent augmentation gluteoplasty. Specific implants were used for the gluteal area, with implant volume ranging from 250 mL to 800 mL (mean, 367 mL).
RESULTS: There was a significant increase in the gluteal volume of patients along with achievement of natural and harmonious contours. Immediate and long-term satisfaction with the cosmetic results was obtained in 100% of patients.
CONCLUSIONS: The use of intramuscular gluteal prostheses is a safe and easily reproducible method of augmentation gluteoplasty with good results and a low complication rate. Determination of the limits of detachment using fixed bone structures simplifies the implementation of this technique, allowing the use of even larger implants than those reported in the literature.
Keywords: Buttocks. Prostheses and implants. Plastic surgery/methods.
RESUMO
INTRODUÇÃO: Região glútea harmoniosa é considerada elemento essencial na composição da beleza corporal e expressão maior de feminilidade, suscitando o crescente interesse de homens e mulheres na melhoria estética dessa região. O objetivo deste estudo é demonstrar uma alternativa às técnicas já publicadas acerca da gluteoplastia de aumento, baseada na colocação da prótese intramuscular, utilizando de forma simplificada os limites da dissecção, tendo como referência as estruturas anatômicas fixas (ósseas) da região glútea na confecção da loja do implante, assim como demonstrar sua viabilidade como técnica segura e reprodutível.
MÉTODO: No período de 2001 a 2011, foram operados 18 pacientes, com idade variando de 25 anos a 50 anos, sendo usados implantes específicos para a área glútea, com o volume variando de 250 ml a 800 ml (média de 367 ml).
RESULTADOS: Foi obtido aumento significativo do volume glúteo dos pacientes, acompanhado de contornos naturais e harmoniosos, havendo satisfação imediata e a longo prazo com os resultados estéticos obtidos em 100% dos pacientes.
CONCLUSÕES: O uso da prótese glútea intramuscular demonstrou ser uma alternativa segura e facilmente reprodutível na gluteoplastia de aumento, com bons resultados e baixo índice de complicações. A determinação dos limites do descolamento utilizando estruturas ósseas fixas proporcionou simplicidade na execução, permitindo o uso de implantes ainda maiores aos relatados na literatura.
Palavras-chave: Nádegas. Próteses e implantes. Cirurgia plástica/métodos.
The gluteal region or buttocks have long been regarded as an essential element in the composition of beauty and remain to this day the greatest expression of femininity. This has evoked a growing interest, from both men and women, in improving the aesthetics of this anatomical region.
Augmentation gluteoplasty has been performed since 1969. The original report by Bartels et al.1 described the use of breast implants in the buttocks. However, originally described techniques used subcutaneous prostheses and resulted in several complications such as dislocation, asymmetry, and capsular contracture2. Therefore, their use was discontinued.
In 1984, Robles et al.3 presented a technique that involved the insertion of implants deep into the gluteus maximus muscle, in the sub-gluteus space, through a median sacral incision. This technique prevented many of the complications that occur with subcutaneous implants and generated new interest in augmentation gluteoplasty.
Later, Vergara and Marcos4 reported the possibility of implants within the gluteus maximus muscle; however, they did not establish a method for this technique or detail the levels and limits of dissection involved.
In 2004, Gonzalez5 described the XYZ procedure for placing gluteal prostheses in an intramuscular position; this procedure involved determination of 3 reference points (X, Y, and Z) and a line (G) as a guide for placement inside the gluteus maximus.
The aim of this study is to present an alternative to the reported techniques on augmentation gluteoplasty. This technique is based on intramuscular placement of the prosthesis using simplified limits of dissection with reference to the fixed anatomical structures (bones) of the gluteal region during creation of the implant pocket. We also demonstrate its viability as a safe and reproducible technique.
METHODS
From 2001 to 2011, 18 patients underwent operation using the method described below. Patient ages ranged from 25 to 50 years (mean, 32 years), and only 2 patients were male.
In all cases, the indication for surgery was purely cosmetic correction for gluteal hypoplasia. Specific implants for the gluteal area were used. In 3 cases, we used round smooth prostheses. In 6 cases, textured oval prostheses were used, and Quartzo® prostheses (high profile oval models) were implanted in the 9 remaining cases. The volume of the implants ranged from 250 to 800 mL (mean, 367 mL).
Initially, the patient was marked preoperatively in 2 positions. In an orthostatic position, the upper limit of the intergluteal fold was marked with a small transverse line, indicating the start of the skin incision. Then, with the patient seated, a crossbar was drawn on each buttock at the ischial tuberosity, corresponding to where the patient supported his/her weight and representing the lower limit of intramuscular detachment (Figure 1).

Figure 1 - Marking of the upper skin incision and lower intramuscular detachment boundaries.
Next, the patient was positioned on the operating table in the prone position, with protective cushions under the hips and ankles, and skin preparation and placing of fields was performed.
The surgery began with a narrow spindle-shaped skin incision (6 cm long and 0.5 cm wide on average), strictly respecting the patient's intergluteal groove and with reference to the skin markings performed preoperatively. This was followed by de-epithelization of this zone in order to construct a central dermal island with preservation of the sacrocutaneous ligament, an element of fundamental importance to the reconstruction of the intergluteal fold. The incision was deepened with a slight lateral tilt, until the gluteal fascia was reached. Surgery continued with detachment in the subcutaneous tissue by imagining a semicircle originating in the midline with a radius of approximately 8 cm, in order to allow proper exposure of the gluteus maximus and its fascia. Then, starting from a point 2-3 cm lateral to the sacral edge, the gluteal fascia was incised with a 6-cm long cut in the direction of the muscle fibers, and the intramuscular plane was bluntly dissected with Duval forceps to approximately 3 cm deep (using the length of the distal phalanx of the index finger as a reference) in order to begin creation of the implant pocket. Subsequently, a hard triangular detacher was introduced in a lateral direction proximal to the femoral trochanter, which was the lateral limit of the implant pocket. Mid-cranial detachment was then performed proximally towards the iliac crest at a point approximately 6 cm lateral to the posterior superior iliac spine and caudal to the level of the uppermost portion of the ischial tuberosity, represented by the transverse skin markings performed preoperatively, in order to create an implant pocket of the size necessary to accommodate the implant (Figure 2).
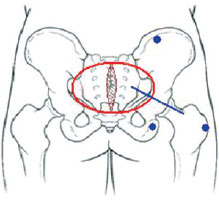
Figure 2 - Schematic diagram showing the fixed bone structures used for delimitation of intramuscular detachment (blue dots), namely: the lateral border of the femoral trochanter, the upper border of the ischial tuberosity, and the lower border of the iliac crest 6 cm lateral to the posterior superior iliac spine. Red circle: area of subcutaneous detachment for muscle exposure. Blue line: orientation of incision in the fascia for the creation of the implant pocket.
Importantly, care was taken to maintain uniform thickness of the muscle cover during all steps of detachment, as well as to respect the limits of the muscle itself, in order to avoid muscle tear and subsequent displacement of the prosthesis.
After review of hemostasis in the implant pocket using a Doyen retractor, tests were conducted using test prosthesis, followed by the inclusion of a prosthesis of the chosen size. The same steps were then reproduced on the contralateral side.
Sequential plane closure was performed with 3-0 nylon for interrupted simple stitches to the fascia and muscle, 3-0 vicryl for Baroudi6 sutures, and 4-0 monocryl for reverse sutures in the dermal plane.
Closed Portovac no. 4.8 drains were used in selected cases, depending on the occurrence of major intraoperative bleeding. The patient was instructed to switch position regularly during the first 5 postoperative days.
RESULTS
A significant increase was obtained in the buttock volume of patients, accompanied by natural and harmonious contours. Immediate and long-term satisfaction with the cosmetic results was achieved in 100% of patients (Figures 3 to 5).

Figure 3 - Thirty-two-year-old patient with implantation of smooth round 350-mL prostheses. In A and C, preoperative appearance. In B and D, postoperative appearance.
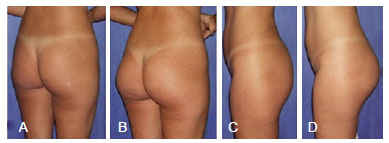
Figure 4 - Twenty-six-year-old patient with implantation of oval 350-mL Quartzo® prostheses. In A and C, preoperative appearance. In B and D, postoperative appearance.
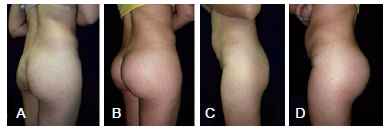
Figure 5 - Thirty-four-year-old patient with implantation of oval 350-mL Quartzo® prostheses. In A and C, preoperative appearance. In B and D, postoperative appearance.
It was not necessary to perform post-surgery complementary procedures such as fat grafting of sciatic skin depression or inferior dermotuberal gluteal lifting for any patient.
The postoperative recovery of all patients was uneventful with no complaints.
Among postoperative complications, 1 patient had a minor wound hematoma and 3 had minor seroma, which drained spontaneously under local care. Eight patients had wound dehiscence, which healed by second intention without intervention.
DISCUSSION
In the past, the use of prostheses in the subcutaneous plane has showed high rates of complications such as capsular contracture, asymmetry, fibrosis, extrusions, inferior migration of implants, and visible and palpable prostheses; these complications relegated this technique to a historical curiosity2,7,8. Additionally, the space between the gluteus maximus and medius originally described by Robles3 for use in the submuscular technique is somewhat limited. The pyramidal muscle cannot be surpassed in a caudal direction because of the potential compressive effect of the implant on the sciatic nerve exposed in the intergluteal space below this muscle. This results in the implant position being too high, with insufficient padding of the lower poles (double bubble sign) and evident damage to the aesthetic outcome.
In contrast, the intramuscular technique compensates for this disadvantage. When it is used for introducing gluteal implants, the intramuscular plane provides good coverage and protection of the prosthesis, flexibility in positioning the implant, excellent modeling of the buttocks, and the possibility of placing the prosthesis in a lower position, since detachment is not limited by the upper edge of the pyramidal muscle9.
In the technique employed in this study, the use of fixed structures for defining detachment in the intramuscular plane conferred benefits such as simplicity of technique, a faster learning curve for the trainee surgeon, and the possibility of using larger implants compared to those used in other intramuscular techniques reported in the literature (300 mL; 350 mL; 360 mL), with the use of prostheses up to 800 mL being possible without a large increase in technical difficulty.
CONCLUSIONS
The use of intramuscular gluteal prostheses proved to be a safe and easily reproducible method of augmentation gluteoplasty, with good results and a low complication rate. The determination of the limits of dissection using fixed bone structures provided simplicity in implementation, allowing the use of implants that were larger than those previously reported.
REFERENCES
1. Bartels RJ, O'Malley JE, Douglas WM, Wilson RG. An unusual use of the Cronin breast prosthesis. Case Report. Plast Reconstr Surg. 1969;44(5):500.
2. González-Ulloa M. Gluteoplasty: a ten-year report. Aesthetic Plast Surg. 1991;15(1):85-91.
3. Robles JM, Tagliapietra JL, Grandi MA. Gluteoplastia de aumento: implante submuscular. Cir Plast Iberolatinoam. 1984;X:4-9.
4. Vergara R, Marcos M. Intramuscular gluteal implants. Aesthetic Plast Surg. 1996;20(3):259-62.
5. Gonzalez R. Augmentation gluteoplasty: the XYZ method. Aesthetic Plast Surg. 2004;28(6):417-25.
6. Baroudi R, Ferreira CA. Seroma: how to avoid it and how to treat it. Aesthet Surg J. 1998;18(6):439-41.
7. Almeida Júnior GL, Castro WC, Almeida EG. Implante glúteo em posição intramuscular parcial: relato de caso. Rev Bras Cir Plást. 2009;24(2):242-5.
8. Dini GM, Ferreira LM. Capsular contracture in gluteal implant patients. Plast Reconstr Surg. 2006;117(3):1070-1.
9. Almeida Júnior GL, Almeida EG. Implante glúteo - técnica XYZ: estudo retrospectivo. Rev Bras Cir Plást. 2008;23(2):103-11.
1. Plastic surgeon, full member of the Brazilian Society of Plastic Surgery (SBCP), head of the Plastic Surgery Service of the Instituto Dr. José Frota (IJF), Fortaleza, CE, Brazil.
2. Aspiring member of the SBCP, resident physician of the Plastic Surgery Service of the IJF, Fortaleza, CE, Brazil.
3. Plastic surgeon and associate member of the SBCP, preceptor of the Plastic Surgery Service of the IJF, Fortaleza, CE, Brazil.
Correspondence to:
Francisco de Assis Montenegro Cido Carvalho
Rua Ana Bilhar, 44/202 - Meireles
Fortaleza, CE, Brazil - CEP 60160-110
E-mail: drcidocarvalho@yahoo.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: June 28, 2012
Article accepted: September 15, 2012
This study was performed at the Plastic Surgery Service of the Instituto Dr. José Frota (IJF), Fortaleza, CE, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter