

Original Article - Year 2012 - Volume 27 -
Popliteal pterygium syndrome: case report and literature review
Síndrome do pterígio poplíteo: relato de caso e revisão da literatura
ABSTRACT
Popliteal pterygium syndrome is a rare congenital condition involving craniofacial and genitourinary anomalies as well as malformation of the extremities. The most obvious characteristics of this syndrome are popliteal pterygium and a triangular crease of skin over the hallux. In this study, we present the case of a 1-month-old male patient with cleft upper and lower lips, cleft palate, bifid scrotum, syndactyly, popliteal pterygium, and a crease of skin over the hallux nail. The patient underwent several surgical interventions aimed at correcting these anomalies. Malformation of the lower limbs was the most difficult anomaly to correct; correction of this anomaly required further combined effort with an orthopedics team in order to avoid nerve grafts and functional deficits. When popliteal pterygium syndrome is treated in a timely and appropriate manner by a multidisciplinary team, a good prognosis is observed.
Keywords: Pterygim. Cleft lip. Cleft palate.
RESUMO
A síndrome do pterígio poplíteo é uma condição congênita rara, que envolve anomalias craniofaciais, geniturinárias e de extremidades. As características mais marcantes dessa síndrome são o pterígio poplíteo e uma dobra de pele triangular sobre a unha do hálux. Neste trabalho, é apresentado o caso de um paciente do sexo masculino, com um mês de idade, apresentando fendas labiais superiores e inferiores, fenda palatal, bolsa escrotal bífida, sindactilia de pododáctilos, pterígio poplíteo e dobra de pele sobre a unha do hálux. O paciente foi submetido a diversas intervenções cirúrgicas, visando à correção das anomalias. Dentre as malformações, a mais difícil de ser corrigida é a relacionada aos membros inferiores, sendo necessária abordagem conjunta com a equipe de ortopedia, na tentativa de evitar enxertos nervosos e déficits funcionais. A síndrome do pterígio poplíteo, quando tratada no momento apropriado e por equipe multidisciplinar, apresenta bom prognóstico.
Palavras-chave: Pterígio. Fenda labial. Fissura palatina.
Popliteal pterygium syndrome is a rare congenital condition involving craniofacial and genitourinary anomalies as well as malformation of the extremities. This syndrome was first described by Trélat in 1869 and received its current designation from Gorlin in 19691. Among the craniofacial anomalies involved in this syndrome, cleft lip and/or cleft palate are commonly found (Figure 1). In addition, small lower lip pits, which the salivary ducts flow into; syngnathia, represented by congenital bands of tissue between the maxilla and the mandible; and ankyloblepharon filiforme adnatum, which is fusion of the eyelid margins by small threads of abnormal tissue, can also be observed. The most striking characteristic of this syndrome is popliteal pterygium, which consists of a net of connective tissue spreading from the ischial tuberosity to the calcaneus. This pterygium may severely limit extension, abduction, and rotation of the leg (Figure 2). It may also be associated with the absence of lower limb muscles or abnormal insertion of these muscles and/or tendons2. Deformities in the digits of the hands and feet, such as syndactyly, digit hypoplasia, and brachydactyly, may also be observed. An almost pathognomonic characteristic of this syndrome is a crease of skin, usually triangular, starting from the base of the nail of the hallux; this is present in one-third of cases3 (Figure 3). Genitourinary alterations are present in both genders. In females, hypoplasia of the labia majora is the most common alteration, with hypoplasia of the vagina and womb as well as hypertrophy of the clitoris also being described. In males, uni- or bilateral cryptorchidism and absent or bifid scrotum may be present, with the penis usually being normal. No alterations have been observed in growth and intellect. Other deformities associated with popliteal pterygium syndrome include scoliosis, clubfoot, hidden spina bifida, a small sternum, and bifid rib.
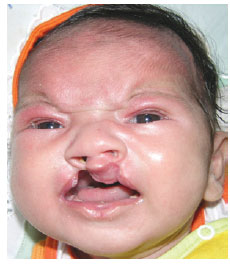
Figure 1 - Pre-operative appearance of the face.
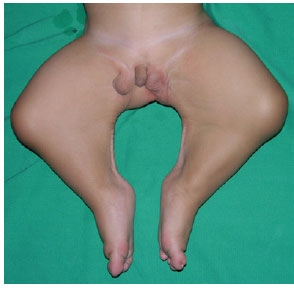
Figure 2 - Pre-operative appearance of the popliteal pterygium.

Figure 3 - Skin crease over the hallux.
In the absence of a positive family history, some authors have suggested minimal criteria for the diagnosis of popliteal pterygium syndrome that include at least 3 of the following characteristics: cleft palate and/or popliteal pterygium, genital anomalies, ectopic salivary ducts in the lower lip, and digit and nail anomalies.
Autosomal dominant transmission is usually the cause of familial cases, with decreased penetrance and large intrafamilial phenotypic variation being associated with the syndrome. The ratio of male:female patients is 1:12. The condition is usually diagnosed when typical manifestations of the syndrome are observed2,4. The variability in the expression of this syndrome may lead to a retrospective diagnosis in previous generations that showed less evident signs of popliteal pterygium syndrome3,5. However, most reported cases are sporadic, and the first-degree relatives of these patients must be carefully investigated to detect minimal anomalies that may be present, such as syngnathia or ankyloblepharon, in order to exclude hereditary transmission2.
A new spontaneous mutation could explain the sporadic nature of popliteal pterygium syndrome. An alternative explanation may be the lack of penetrance of the gene in a parent, justifying why some people can be mere carriers of the disease in familial cases5. The location of the responsible gene is still unknown5; however, Lees et al.4 showed that there is a consistent connection with the 1q32 locus (also known as the Van der Woude syndrome locus), although this still requires confirmation by further studies.
The pathogenesis of popliteal pterygium syndrome is partially understood, and several hypotheses have been raised, such as primary microvascular abnormalities associated with edema, leading to a disturbance of the epithelial tissues and resulting in the formation of secondary adhesions, excessive epithelial growth leading to fusion and secondary mesenchymal involvement, primary collagen defects, and loss of the apoptotic mechanism. Genetic and histopathological studies are required to further elucidate the nature of this syndrome4.
CASE REPORT
A 1-month-old patient, presenting with numerous congenital anatomical abnormalities, was referred to the outpatient plastic surgery service of the Hospital Pediátrico da Universidade Federal do Rio Grande do Norte.
Born by spontaneous delivery at full term and weighing 4.5 kg, the patient was the fourth son of a couple with 4 children, and none of the siblings showed evidence of malformations. The mother reported no occurrence of previous miscarriages. The pregnancy had been detected at 8 gestational weeks, and the mother had been taking an oral contraceptive pill (Norentindrona, 0.35 mg) until she realized that she was pregnant. The mother started taking folic acid and iron supplements in the fifth gestational month.
The main malformations found in the patient were as follows: bilateral cleft in the upper lip; middle lower lip cleft with ectopic salivary glands, similar to that found in Van der Woude syndrome; cleft palate; bifid scrotum with topical testicles (1 testicle in each chamber); and syndactyly. The patient also had a crease of skin, which was triangular in shape, starting from the base of the nail of the hallux. In addition to all these anomalies, the child also had popliteal pterygium, which constitutes the main characteristic of the syndrome in question.
Study of the patient's karyotype did not reveal any alterations. The neuropsychomotor development of the child was considered normal and appropriate for his age. The patient did not show any other malformations besides those already mentioned. We performed nuclear magnetic resonance imaging of the limbs, which showed topical muscles in the thighs and lower legs and vascular-nervous bundles running 1.5 cm below and parallel to the fibrous cord connecting the ischium to the calcaneus (the popliteal pterygium).
Surgical procedures were performed as follows. At the age of 4 months, cleft repair was performed on the right side using a combination of the techniques reported by Göteborg and McComb to correct the most open side of the cleft. At the age of 5 months, a second cleft repair was carried out, this time on the left side, using the same technique. At the age of 12 months, the child starting walking, a process that was tremendously hindered by the popliteal pterygium that prevented upright walking. At this point, we decided to correct the popliteal pterygium in 1 limb at a time and to observe further development of the clinical picture. Since the left limb was most shortened, it was operated on first, because the objective of the procedure was to increase limb extension. Several Z-plasties were performed on the skin that covered the pterygium, to dissect all of the path and the branches of the sciatic nerve and to resect the fibrous cord connecting the ischium to the calcaneus, as well as the fascia involving the entire pterygium (Figure 4). All nerve dissection was aided by the use of an intraoperative neurostimulator (Figure 5). At the end of the surgery, the limb had an extension of about 150 degrees; this was higher than the preoperative angle, which was 90 degrees. To further increase limb extension, the patient started physiotherapy 15 days postoperatively. At the age of 15 months, the patient underwent correction of the lower right limb, using the same technique. Finally, at 23 months, the patient underwent complete palatoplasty using the technique of intravelar veloplasty reported by Veau, lower cleft repair with excision of the ectopic salivary glands, and secondary upper cleft repair to correct the vermillion (Figure 6).
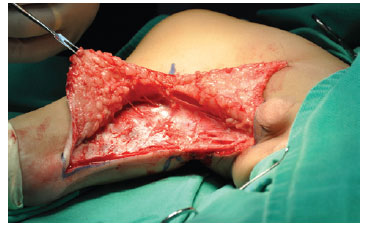
Figure 4 - Fascia involving the pterygium.

Figure 5 - Nerve dissection.

Figure 6 - Recent postoperative appearance of the face.
DISCUSSION
Popliteal pterygium syndrome is clinically diagnosed, and diagnosis involves detection of its identifiable phenotypic characteristics, particularly the popliteal pterygium. The patient described in the current report had all the minimal criteria for the diagnosis of this syndrome (cleft palate, popliteal pterygium, genital abnormalities, ectopic salivary ducts in the lower lip, and anomalies of the digits and nails). The patient did not have any positive family history; this is in agreement with findings of previous studies, where the sporadic form of this syndrome is the most commonly described2-9.
Since the patient described in this report had several malformations, follow-up by a multidisciplinary team consisting of specialists such as a plastic surgeon, a phonoaudiologist, and an orthodontist, was performed. Thus, the treatment was as complete as possible and was aimed at satisfactory recovery.
Surgical procedures were carried out in steps, respecting the physical limitations of the patient and his young age. We tried to tailor the chronology of the surgeries to the child's needs at each time. As described previously, the following sequence of surgeries was used: right cleft repair (4 months); left cleft repair (5 months); correction of the left popliteal pterygium (12 months); correction of the right popliteal pterygium (15 months); total palatoplasty, lower cleft repair with excision of the ectopic salivary glands, and secondary upper cleft repair (23 months).
The improvement in extension of the lower limbs, which increased from 90 degrees to 150 degrees, was considered good but not ideal (Figure 7). After surgery, the only limiting factor for extension of the limb was the decreased length of the nerve, since the fibrous bundle and the fascia involving the pterygium and restricting extension of the leg had been resected. Daily physical therapy was initiated 15 days postoperatively to improve extension of the limb and achieve an angle of 180 degrees. After 8 months of physiotherapy, an improvement of 10 degrees was observed in the right limb and an improvement of 5 degrees was observed in the left limb.

Figure 7 - Postoperative appearance of the lower limbs when resting.
Presently, cicatricial contraction has occurred in some Z-plasties and neuronal extension has reached its limit, since the patient exhibits clubfoot walking, only making full plantar contact with the ground when he is static and with discreet flexion of the knees (Figure 8). The case was discussed with the orthopedics team of our institution, and it was decided to perform bilateral oblique femoral osteotomy (in 2 surgeries) to shorten the limbs, with the aim of fitting the size of the limbs to the size of the nerve. This approach was chosen to avoid nerve grafts, which may cause motor and sensory deficits. We also plan to carry out further Z-plasties to repair the contractures.

Figure 8 - Clubfoot walk and cicatricial contractures.
CONCLUSIONS
Popliteal pterygium syndrome is a very rare condition and involves several malformations without well-defined genetic transmission, with the sporadic version being the most common. This syndrome must be treated by a multidisciplinary team and requires several surgical procedures in various different anatomical units, making it a challenge for plastic surgeons. The popliteal pterygium is the most difficult malformation to correct and occasionally requires femoral osteotomies to shorten the lower limbs while avoiding nerve grafts and possible neurological, motor, and/or sensory deficits. When treated in a timely and appropriate manner by a multidisciplinary team, popliteal pterygium syndrome has a good prognosis.
REFERENCES
1. Gorlin RJ, Sedano HO, Cervenka J. Popliteal pterygium syndrome. A syndrome comprising cleft lip-palate, popliteal and intercrural pterygia, digital and genital anomalies. Pediatrics. 1968;41(2):503-9.
2. Froster-Iskenius UG. Popliteal pterygium syndrome. J Med Genet. 1990;27(5):320-6.
3. Spauwen PH, Cobben JM, Gardeniers JW. The popliteal pterygium syndrome: an analysis of two families. J Craniomaxillofac Surg. 1994;22(5):276-80.
4. Lees MM, Winter RM, Malcolm S, Saal HM, Chitty L. Popliteal pterygium syndrome: a clinical study of three families and report of linkage to the Van der Woude syndrome locus on 1q32. J Med Genet. 1999;36(12):888-92.
5. Koch H, Grzonka M, Koch J. Popliteal pterygium syndrome with special consideration of the cleft malformation: case report. Cleft Palate Craniofac J. 1992;29(1):80-4.
6. Khan SN, Hufnagle KG, Pool R. Intrafamilial variability of popliteal pterygium syndrome: a family description. Cleft Palate J. 1986;23(3):233-6.
7. Gahm C, Kuylenstierna R, Papatziamos G. Popliteal pterygium syndrome (PPS) with intra-alveolar syngnathia: a discussion of anesthetic and surgical considerations. Int J Pediatr Otorhinolaryngol. 2007;71(10):1613-6.
8. Escobar V, Weave D. Popliteal pterygium syndrome: a phenotypic and genetic analysis. J Med Genet. 1978;15(1):35-42.
9. Ferreras JM, Pimentel de Castro R, Vásquez A, Rizeck J. Sindrome de pterigión popliteo: a propósito de un caso. Acta Méd Domin. 1992;14(1):20-2.
1. Associate member of the Sociedade Brasileira de Cirurgia Plástica/Brazilian Society of Plastic Surgery, member of the Associação Brasileira de Cirurgia Crânio-Maxilo-Facial/Brazilian Association of Skull-Maxillo-Facial Surgery, plastic surgeon of the cleft lip program of the Universidade Federal do Rio Grande do Norte (UFRN), Natal, RN, Brazil.
2. Medical student at UFRN, Natal, RN, Brazil.
Correspondence to:
Leonardo Santos de Barros Spencer
Rua Joaquim Fabrício, 270 - ap. 1001 - Petrópolis
Natal, RN, Brazil - CEP 59012-340
E-mail: plastica.spencer@hotmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: April 15, 2010
Article received: February 22, 2011
This study was performed at the Hospital de Pediatria (HOSPED) da Universidade Federal do Rio Grande do Norte, Natal, RN, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter