

Original Article - Year 2012 - Volume 27 -
Epidemiologic study of burn injuries in children admitted to the Burn Unit of the Hospital de Urgência de Sergipe
Estudo epidemiológico de crianças vítimas de queimaduras internadas na Unidade de Tratamento de Queimados do Hospital de Urgência de Sergipe
ABSTRACT
BACKGROUND: Burn wounds constitute one of the most serious types of trauma and are a major cause of unintentional death in children. The aim of this study was to determine the epidemiological profile of children experiencing burn wounds.
METHODS: We conducted a retrospective study of burn patients admitted to the Burn Care Unit of the Hospital de Urgência de Sergipe from January 2004 to December 2006.
RESULTS: Among the children admitted, there was a predominance for males (57.8%); most of the children (57.6%) were aged between 1 and 3 years. Heated liquid was the most common agent responsible for burns (71.6%), and second-degree burns were predominant (59.3%). The chest was the most commonly affected area (28.9%).
CONCLUSIONS: The majority of pediatric burn injuries result from domestic accidents. Children, particularly those younger than 4 years, are the main victims, and heated liquids are the most common agents.
Keywords: Burns. Child. Epidemiology. Accident prevention. Burn units.
RESUMO
INTRODUÇÃO: As queimaduras constituem-se em um dos tipos de trauma mais graves e uma das principais causas de morte não-intencional em crianças. O objetivo deste estudo foi traçar o perfil epidemiológico de crianças queimadas.
MÉTODO: Foi realizado um estudo retrospectivo de pacientes vítimas de queimaduras que deram entrada na Unidade de Tratamento de Queimados, no período de janeiro de 2004 a dezembro de 2006.
RESULTADOS: Observou-se predominância das internações em indivíduos do sexo masculino (57,8%), a maioria das crianças atendidas (57,6%) tinha idade entre 1 ano e 3 anos, o líquido aquecido foi o mais frequente agente responsável pelas queimaduras (71,6%), predominaram as queimaduras de segundo grau (59,3%), e o tórax foi o local mais atingido (28,9%).
CONCLUSÕES: A maioria das queimaduras constitui acidente doméstico, do qual as crianças são as principais vítimas, especialmente aquelas com menos de 4 anos de idade, e os líquidos aquecidos são os agentes mais comuns.
Palavras-chave: Queimaduras. Criança. Epidemiologia. Prevenção de acidentes. Unidades de queimados.
Burns are among the leading external causes of death in Brazil, second only to other violent causes such as traffic accidents and homicides1. The burn is considered one of the most devastating human injuries. This reputation stems not only from its high incidence and high mortality rate2, but also - more importantly - from its functional, aesthetic, and psychological sequelae.
Burns are among the most common childhood accidents; they are the fourth leading cause of death after traffic, drowning, and falls3, and are seventh in the reasons for hospital admission4. Data from the National Burn Repository revealed that among burns that occurred between 1995 and 2005, more than 6000 occurred in children younger than 2 years, 2987 occurred in children aged between 2 and 4 years, and more than 3000 occurred in children over 5 years of age5. In addition to their potential for serious sequelae, such accidents require several days of hospitalization and therapeutic monitoring of patients after hospital discharge6.
Data from the Brazilian Society of Burns show that there are approximately 1 million burn cases every year in Brazil, of which 200,000 are treated in emergency services; 40,000 of these require hospital admission1. In Brazil, burns are a major health problem, affecting people of all ages and both sexes. Several epidemiological studies have been unanimous in stating that most burn victims are children (on average, 80% of cases), both national and internationally; they also emphasize that, in Brazil, statistical data on these injuries are still scarce7,8.
Thus, alongside awareness campaigns and legal measures, the survey of epidemiological data can be an important tool for the prevention of such accidents in children.
This study aimed to delineate the epidemiology of children aged younger than 12 years who were treated at the Burn Care Unit at the Hospital de Urgência de Sergipe.
METHODS
We conducted a cross-sectional, retrospective study using data from medical chart records from the Medical Records and Statistics (SAME) of pediatric burn victims younger than 12 years who were admitted to the Burn Care Unit of the Hospital de Urgência de Sergipe from January 2004 to December 2006.
Information was collected regarding age, sex, body region affected by the burn, extent of body surface burned, etiological agent, length of stay, depth of the burn, and surgical intervention.
The study was approved by the Ethics Committee of the Universidade Tiradentes, Protocol 031206.
RESULTS
Among the 846 patient records surveyed, 479 (57%) were children under 12 years of age; 277 children were male (57.8%) and 202 were female (42.2%).
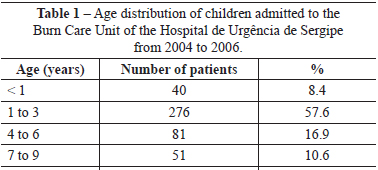
With regard to age, 276 (57.6%) children were in the range from 1 to 3 years; children aged 1 year were most common, with 172 (35.9%) cases. The lowest hospitalization rate was observed among children aged 10 to 12 years (Table 1).
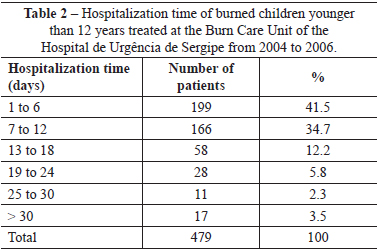
In most (n = 365; 76.2%) cases, the length of hospitalization ranged from 1 to 12 days (Table 2).
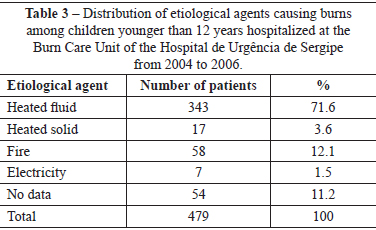
Thermal energy was responsible for burns in almost 90% of cases, especially heated liquids, which were the etiologic agent in 71.6% (n = 343) of accidents (Table 3).
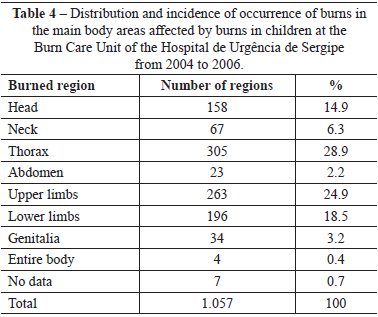
The distribution and incidence of burns in various body regions are shown in Table 4.
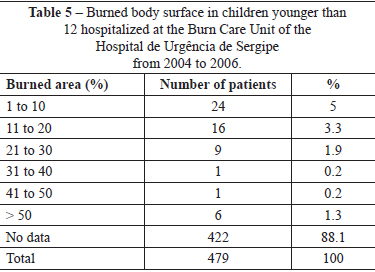
Estimates of the extent of the burn in terms of body surface area were found in only 57 records; these findings are shown in Table 5.
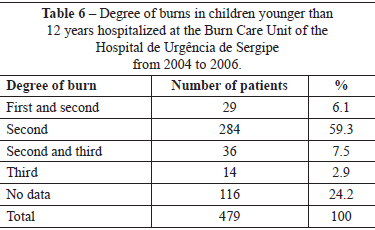
With regard to burn depth, second-degree burns were predominant (n = 284; 59.3%) (Table 6).
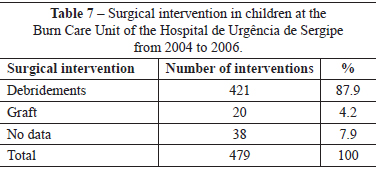
Among surgical procedures employed in treatment, débridement was predominant, having been performed in 87.9% of cases (Table 7).
DISCUSSION
Burns are considered a serious public health problem in Brazil. Knowledge of epidemiological data is of great importance in obtaining financial support for burn prevention and treatment programs and in helping to define the parallels between the experiences of national and international centers.
It was found that, of 479 patients admitted to the Burn Care Unit, 57.8% were male, a finding similar to that described by several authors9-13.
In this study, more than 76% of the patients were hospitalized for a mean period of 2 weeks. Similar results were also found by other Brazilian authors10,13,14; in the other studies, 61.9% to 76.8% of the patients studied had a mean hospitalization time of 2 weeks. In the present study, in 17 (3.5%) cases, hospitalization was more than 4 weeks. In the studies by Pereira Júnior et al.10 and Coutinho et al.13, 14.3% to 20.6% patients had an average length of stay of more than 4 weeks.
Thermal energy was the most common etiologic agent of burns in patients admitted to the Burn Care Unit, particularly heated liquids (water, oil, coffee, and milk), which are part of the syndrome known as "hot kettle". These findings corroborate those reported by Rossi et al.7, Costa et al.9, Harada et al.15, and Gaspar et al.16, who attributed this to the fact that children have easy access to high-risk environments such as kitchens.
Information on the body surface area burned was not gathered in 88.1% of cases due to missing information in the medical records. From the 57 complete records, it was found that burns with areas between 1% and 10% of total body surface were most common, corresponding to 24 (42.1%) cases. These findings differ from other studies, in which the rates of extent of burned body surface area ranged from 57% to 61.4%14,17,18.
There was a predominance of second-degree burns, which accounted for 59.3% of cases. Similar results were found by several authors7,12,19,20, who found the incidence of second-degree burns to range from 33% to 49.7% of all burns. In contrast, Pereira Júnior et al.10 found that third-degree burns were the most frequent (42.9%). Regarding the body region affected by burns, the distribution was very similar between the thorax and the upper limbs, with 28.9% and 24.9%, respectively. These findings are consistent with those reported in studies of Pereira Júnior et al.10 and Gimenes et al.11, according to whom the main targets were the trunk and upper limbs.
In our study, early débridement and grafting of the injuries occurred in 87.9% and 4.2% of cases, respectively, which is in agreement with other authors10,14 who pointed out that, despite technological advances, debridement, autograft, and flaps still yield the best aesthetic and functional results.
CONCLUSIONS
The results of this study revealed that, among pediatric burn victims in Burn Care Units, 1 to 3 years is the most common age of injury, and heated liquids are the main agent responsible for burns. The regions of the thorax and upper limbs were the most affected, predominantly by second-degree burns.
REFERENCES
1. Vale ECS. Primeiro atendimento em queimaduras: a abordagem do dermatologista. An Bras Dermatol. 2005;80(1):9-19.
2. Ferreira E, Lucas R, Rossi LA, Andrade D. Treatment of the burned patient: a review of the literature. Rev Esc Enferm USP. 2003;37(1):44-51.
3. Dalaneze MC. Queimaduras na infância. Pediatr Mod. 1996;32:259-72.
4. Willis A, Fowler B, Rea S, Wood F. Testing nurses burn injury knowledge. Aust Nurs J. 2007;14(8):30-1.
5. Ring LM. Kids and hot liquids: a burning reality. J Pediatr Health Care. 2007;21(3):192-4.
6. Kliemann JD, Lehugeur DS, Franche GLS, Seara SC. Acidentes por queimaduras em crianças: estudo epidemiológico. Rev HPS. 1990;36(1):36-41.
7. Rossi LA, Barruffini RCP, Garcia TR, Chianca TCM. Queimaduras: características dos casos tratados em um hospital escola em Ribeirão Preto (SP), Brasil. Rev Panam Salud Pública. 1998;4(6):401-4.
8. Rossi LA, Ferreira E, Costa ECFB, Bergamasco EC, Camargo C. Prevenção de queimaduras: percepção de pacientes e de seus familiares. Rev Latino-Am Enfermagem. 2003;11(1):36-42.
9. Costa DM, Abrantes NM, Lamounier JA, Lemos ATO. Estudo descritivo de queimaduras em crianças e adolescentes. J Pediatr. 1999;75(3):181-6.
10. Pereira Júnior S, Ely JB, Sakae TM, Nolla A, Mendes FD. Estudo de pacientes vítimas de queimaduras internados no Hospital Nossa Senhora da Conceição em Tubarão - SC. Arq Catarin Med. 2007;36(2):22-7.
11. Gimenes GA, Alferes FCBA, Dorsa PP, Barros ACP, Gonella HA. Estudo epidemiológico de pacientes internados no Centro de Tratamento de Queimados do Conjunto Hospitalar de Sorocaba. Rev Bras Queimaduras. 2009;8(1):14-7.
12. Silva GPF, Olegario NBC, Pinheiro AMRS, Bastos VPD. Estudo epidemiológico dos pacientes idosos queimados no centro de tratamento de queimados do Hospital Instituto Doutor José Frota do município de Fortaleza-CE, no período de 2004 a 2008. Rev Bras Queimaduras. 2010;9(1):7-10.
13. Coutinho BBA, Balbuena MB, Anbar RA, Anbar RA, Almeida KG, Almeida PYNG. Perfil epidemiológico de pacientes internados na enfermaria de queimados da Associação Beneficente de Campo Grande Santa Casa/MS. Rev Bras Queimaduras. 2010;9(2):50-3.
14. Lacerda LA, Carneiro AC, Oliveira AF, Gragnani A, Ferreira LM. Estudo epidemiológico da Unidade de Tratamento de Queimaduras da Universidade Federal de São Paulo. Rev Bras Queimaduras. 2010;9(3):82-8.
15. Harada MJCS, Botta MLG, Kobata CM, Szauter IH, Dutra G, Dias EC. Epidemiologia em crianças hospitalizadas por acidentes. Folha Med. 2000;119(1):43-7.
16. Gaspar VLV, Lamounier JA, Cunha FM, Gaspar JC. Fatores relacionados a hospitalizações por injúrias em crianças e adolescentes. J Pediatr. 2004;80(6):447-52.
17. Cavalcanti AL, Martins VM, Lucena RN, Granville-Garcia AF, Menezes VA. Morbidade por causas externas em crianças e adolescentes em Campina Grande, Paraíba. Arq Catarin Med. 2008;37(3):27-33.
18. Miranda RE, Pacannaro RC, Pinheiro LF, Calil JA, Gragnani A, Ferreira LM. Trauma elétrico: análise de 5 anos. Rev Bras Queimaduras. 2009;8(2):65-9.
19. Hoch HJS, Lira SVG, Abreu RNDC, Xavier EP, Vieira LJES. Perfil dos acidentes por líquidos aquecidos em crianças atendidas em centro de referência de Fortaleza. RBPS. 2007;20(2):86-91.
20. Mendes CA, Sá DM, Padovese SM, Cruvinel SS. Estudo epidemiológico de queimaduras atendidas nas Unidades de Atendimento Integrado de Uberlândia-MG entre 2000 a 2005. Rev Bras Queimaduras. 2009;8(1):18-22.
1. Physician, associate professor in the Department of Morphology of the Federal University of Sergipe and professor at the School of Medicine of the Universidade Tiradentes (UNIT), Aracaju, SE, Brazil.
2. Physician of the Serviço de Segurança e Medicina do Trabalho da Prefeitura Municipal de Aracaju, Aracaju, SE, Brazil.
3. Nurse at UNIT, Aracaju, SE, Brazil.
4. Nurse at Hospital Universitário Cajuru, Curitiba, PR, Brazil.
5. Physician, professor at the School of Medicine of the UNIT, Aracaju, SE, Brazil.
Correspondence to:
José Aderval Aragão
Rua Aloísio Campos, 500 - Atalaia
Aracaju, SE, Brazil - CEP 49035-020
E-mail: jaafelipe@infonet.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: April 5th, 2012
Article accepted: July 23, 2012
This study was performed at the Universidade Tiradentes (UNIT), Aracaju, SE, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter