

Original Article - Year 2012 - Volume 27 -
Plastic surgery for readjustment of body contours of patients who underwent bariatric surgery during adolescence
Cirurgias plásticas para readequação de contorno corporal de pacientes submetidos a cirurgia bariátrica durante a adolescência
ABSTRACT
BACKGROUND: Surgical treatments for obesity in adolescents were introduced in the 1990s, resulting in individuals undergoing bariatric surgery, and exhibiting weight loss and dysmorphic body features. This produced a demand for plastic surgery in order to readjust the body contour. The aim of this study was to identify factors associated with morbidity and mortality for these corrective body contouring plastic surgeries in patients who underwent bariatric surgery during adolescence.
METHODS: Between January 2008 and January 2011, 5 adolescent patients underwent gastric bypass surgery, with a consequent loss and stabilization of weight, and then underwent plastic surgery for correcting body contours. The average age of the patients at the time of plastic surgery was 19.7 years; 3 (60%) patients were female. Abdominoplasty was performed in all patients (100%), crural dermolipectomy in 4 (80%) patients, brachial dermolipectomy in 2 (40%) patients, thoracoplasty in 2 (40%) patients, torsoplasty in 2 (40%) patients, and a reverse abdominoplasty in 1 (20%) patient. In addition, mammoplasty with inclusion of silicone implants was performed in 2 (40%) female patients, whereas the other female patient (20%) underwent mastopexy. A male patient (20%) underwent correction of gynecomastia. An average of 3 surgical interventions were performed on each patient (range, 2-5), and the number of surgical sites was 20.
RESULTS: Dehiscence occurred in 3 (15% of the surgical sites) cases, and it was necessary to revise the resection because of residual skin laxity in 3 (15% of the surgical sites) patients.
CONCLUSIONS: Some factors associated with body contouring plastic surgeries in adolescents were identified and compared with the literature data.
Keywords: Adolescent. Plastic surgery. Bariatric surgery. Obesity. Morbid obesity. Skinfold thickness.
RESUMO
INTRODUÇÃO: A partir da década de 1990 foram iniciados os primeiros tratamentos cirúrgicos da obesidade em adolescentes, seguindo a sequência cirurgia bariátrica, perda ponderal e dismorfismo corporal, criando demanda por cirurgias plásticas para readequação do contorno corporal. O objetivo deste estudo foi identificar fatores associados a cirurgias plásticas de readequação de contorno corporal (morbidade e mortalidade), realizadas em pacientes submetidos a cirurgia bariátrica durante a adolescência.
MÉTODO: Entre janeiro de 2008 e janeiro de 2011, 5 pacientes submetidos a gastroplastia redutora durante a adolescência, com consequente perda e estabilização de peso, foram submetidos a cirurgias plásticas do contorno corporal. A média de idade no início das cirurgias plásticas foi de 19,7 anos, sendo 3 (60%) pacientes do sexo feminino. Foram realizadas dermolipectomias abdominais em todos (100%) os pacientes, dermolipectomias crurais em 4 (80%), dermolipectomias braquiais em 2 (40%), mamoplastia com inclusão de implantes de silicone em 2 (40%) pacientes do sexo feminino, mastopexia na terceira paciente do sexo feminino (20%) e correção de ginecomastia em 1 (20%), toracoplastia em 2 (40%), torsoplastia em 2 (40%) e torsoplastia reversa em 1 (20%). Foram realizadas, em média, 3 intervenções cirúrgicas por paciente, sendo operados 20 sítios cirúrgicos.
RESULTADOS: Ocorreram deiscências em 3 (15% dos sítios cirúrgicos) casos e foi necessário revisar a ressecção dermogordurosa por flacidez residual em 3 (15% dos sítios cirúrgicos) casos.
CONCLUSÕES: Foram identificados alguns fatores associados às cirurgias plásticas de readequação de contorno corporal na amostra de 5 pacientes submetidos a cirurgia bariátrica durante a adolescência, comparáveis aos da literatura específica.
Palavras-chave: Adolescente. Cirurgia plástica. Cirurgia bariátrica. Obesidade. Obesidade mórbida. Pregas cutâneas.
In a study published in December 2009, the World Health Organization revealed that the prevalence of being overweight or obese in adolescents aged 11 to 13 years ranged from 5% to 25% in the European countries studied1. Despite efforts by international organizations and national governments to promote awareness of the problem and develop preventive measures, the prevalence was found to continue to increase in more than half of the countries analyzed2.
In Brazil, the prevalence of male adolescents who are overweight and obese increased over the period from 1980 to 2005, to a prevalence rate of 3% for overweight and 6% for obesity3.
In this scenario, bariatric surgery has been recognized as the only effective treatment for morbid obesity in adolescents, and a considerable improvement was demonstrated in the quality of life of these patients during the immediate postoperative follow-up4,5. Among adolescent candidates for bariatric surgery, depression and aberrant eating behaviors are very common, demonstrating that early identification and control of these conditions can yield a successful outcome for this type of surgery6.
As a consequence of the loss and stabilization of weight, patients have excess skin folds and require plastic surgery procedures for body contour readjustment in order to improve their body dynamics, hygiene, posture, self-image, and quality of life7.
Despite the recent and abundant literature on bariatric surgery in adolescents, there is little awareness about body contouring plastic surgery in this population and its possible consequences.
The objective of this study was to identify factors associated with morbidity and mortality for body contouring operations in patients undergoing bariatric surgery during adolescence and to compare the results to those reported in the literature.
METHODS
Five adolescent patients with morbid obesity underwent bariatric surgery at the Children's Institute of the Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (Hospital das Clinicas, School of Medicine, Universidade de São Paulo - HCFMUSP) through a malabsorptive and restrictive technique; the operations were performed by a team of pediatric surgeons. The patients were aged between 13 years and 19 years (mean, 17.6 years) and their body mass index (BMI) ranged from 44 kg/m2 to 52 kg/m2 (mean, 47 kg/m2).
After a period of at least 1 year to account for weight loss and stabilization, the patients were considered to have attained nutritional and metabolic balance. The average duration between the start of bariatric surgery and the plastic surgery was 2 years.
The criteria considered for inclusion in the study were: undergoing bariatric surgery during adolescence; stable body weight for at least 1 year with metabolic and nutritional balance; weight loss exclusively through surgery (gastroplasty); and BMI between 20 kg/m2 and 30 kg/m2 after stabilization of body weight.
Exclusion criteria were: smoking, BMI after bariatric surgery < 20 kg/m2 or > 30 kg/m2; body weight stable for < 1 year; inappropriate psychological condition; and negative response to the invitation for participation in the study.
The operations for readjustment of body contours in this group of patients were performed between January 2008 and January 2011 in the Department of Plastic Surgery of HCFMUSP. The surgical procedures performed were defined according to the needs of each individual patient, while considering the extent and location of excess fat and sagging fat tissue, complaints by patients during consultations, and evaluation by the team of plastic surgeons.
The average age at the time of plastic surgery was 19.7 years, and ranged from 17 to 21 years. Three (60%) patients were female. The BMI ranged from 24.2 kg/m2 to 25.6 kg/m2, with a mean BMI of 24.7 kg/m2.
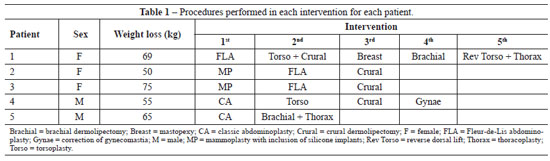
Abdominoplasty was performed in all patients (100%), crural dermolipectomy in 4 (80%) patients, brachial dermolipectomy in 2 (40%) patients, thoracoplasty in 2 (40%) patients, torsoplasty in 2 (40%) patients, and a reverse abdominoplasty in 1 (20%) patient. In addition, mammoplasty with inclusion of silicone implants was performed in 2 (40%) female patients, whereas the other female patient (20%) underwent mastopexy. In addition, a male patient (20%) underwent correction of gynecomastia (Figure 1).
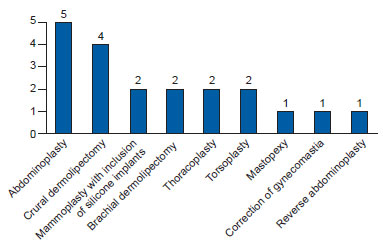
Figure 1 - Distribution of the 20 surgical sites operated on according to the procedure performed.
On average, 3 operations were performed on each patient (range, 2-5) (Table 1). Combined procedures were counted as a single surgical intervention. Twenty surgical sites were operated upon.
Preoperative photographic documentation and demarcation were performed for the approximate delimitation of the tissue to be resected. However, the area of tissue to be resected was determined by traction testing and by verifying the tension during the surgical procedure.
In all surgical interventions, mechanical methods were used for the prevention of deep venous thrombosis, including elastic stockings and intermittent pneumatic compression of the lower limbs (Kendall SCD Express Compression System®). The closing sutures used included 3-0 monofilament resorbable suture thread (poliglecaprone) for the deep layer, 4-0 monofilament resorbable thread (poliglecaprone) for the subdermal layer, and 4-0 monofilament resorbable thread (poliglecaprone) for the intradermal layer. In regions where the skin is delicate, such as the umbilicus and nipple-areolar complex, a 5-0 nylon suture was used.
After all interventions were completed, daily dressing changes were initiated on the third postoperative day, using ointments containing bacitracin and neomycin.
The patients received antibiotic prophylaxis with cefazolin (2 g) intravenously during induction of anesthesia, followed by the administration of cefazolin (1 g) every 4 hours during the surgery; maintenance therapy, involving cefazolin (1 g) administered every 8 hours, was initiated in the immediate postoperative period, until 24 hours from the start of antibiotic administration.
The administration of analgesics and anti-inflammatory drugs was continued postoperatively for 5 days. Mandatory rest was ensured during the first week after surgery and physical activity was avoided for 28 days.
Fleur-de-Lis abdominoplasties were performed in 3 patients and classical abdominoplasties (only horizontal) in the other 2 patients. In all 5 cases, a medial vertical plication was performed on the aponeurosis of the rectus abdominis muscles with 2-0 nylon thread, whereas 3-0 resorbable thread was used for the points of adhesion for tissue approximation. Moreover, in all 3 patients, vacuum drainage was performed for a period of 3-7 days, with the use of surgical compressive mesh, while maintaining the hip in a semi-flexible position.
Crural dermolipectomies were performed in 4 (80%) patients, with the resection extending from the medial aspect of the thigh to the medial aspect of the knee in 4 cases and resection in combination with the lateral aspect of the thigh in 3 cases. Vacuum drainage was performed on the medial aspect of the thigh in all 4 cases and was continued for 7-10 days. A compressive mesh was used in all these patients.
Brachial dermolipectomies were performed in 2 patients, with the resection extending from the medial aspect of the arms in the region of the elbows to the axillae, where small compensatory resections were performed. Drainage was not performed in these cases.
Two mammaplasties with inclusion of silicone implants were performed. The surgical technique was performed without rigid demarcation, with dissection in the lower pole of the breasts and subglandular detachment to expose the pectoralis major muscles, above which the silicone implants were placed. This was followed by the fixation of the breast tissue and repositioning and fixation of the inframammary fold with 2-0 nylon thread. Resection of excess skin in the lower pole of the breast was performed, resulting in scarring in an inverted "T" shape, with subsequent repositioning and suturing of the nipple-areolar complexes. The dressing was covered by a surgical bra, which was worn during the first month after surgery and removed only for dressing changes and bathing. Drainage was not performed in these cases.
Mastopexy was performed without rigid demarcation, with dissection of the lower pole of the breast, subglandular detachment and exposure of the pectoralis major muscles, bipartition and fixation of the breast tissue with fixation of the inframammary folds with 2-0 nylon thread, resection of excess skin, and repositioning and fixation of the nipple-areolar complexes. Closure was performed with the use of a surgical mesh, which was maintained for the first month after surgery.
Corrective gynecomastia was performed in a patient through an infra-areolar incision, resection of excess breast tissue, and closure, without the need for skin resection. Compression was sustained with an elastic band for 2 weeks.
Thoracoplasty was performed in 2 patients, with resection of excess skin folds in the lateral region of the thorax, extending vertically toward the axillae.
Two patients underwent torsoplasty with resection of excess skin folds in the upper buttocks/waist region, in the shape of "seagull wings." Closure was performed with use of surgical mesh that was maintained for the first month after surgery.
In 1 patient, it was necessary to perform a reverse dorsal lift, with resection of excess skin folds from the lateral and dorsal regions of the thorax near the level of the scapula, in the shape of "seagull wings." Closure was performed with use of surgical mesh that was maintained for 2 weeks.
The period of hospitalization ranged from 1 to 3 days, with an average of 1.5 days. The patients underwent immediate postoperative follow-up, with frequent return visits thereafter, on the third, seventh, fourteenth, and twenty-eighth days following surgery. The patients also underwent delayed follow-up at 2, 4, and 6 months postoperatively.
The minimum interval between the surgeries was 6 months and the maximum was 12 months.
RESULTS
Complications occurred on 6 occasions (30% of surgical sites), which were all related to and restricted to the surgical sites (Table 2). Among the complications, dehiscence occurred in 1 patient who underwent Fleur-de-Lis abdominoplasties and in 2 who underwent crural dermolipectomies (15% of surgical sites). The dehiscence was mild in all cases, and could be corrected with debridement and resuturing under local anesthesia.
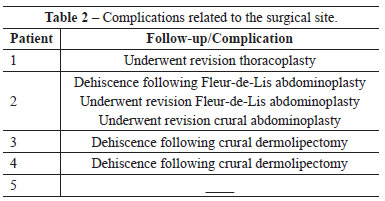
It was necessary to increase the extent of resection of skin folds due to residual flaccidity in 1 patient who underwent thoracoplasty, in 1 who underwent Fleur-de-Lis abdominoplasty, and in 1 who underwent a crural dermolipectomy. In these cases, the patients were rehospitalized, and the interventions were performed under general anesthesia, following the surgical protocol applied initially. No hematomas, seromas, or infections were observed, and no deaths or systemic complications related to the operations were noted.
Figures 2 to 4 illustrate some cases in this series of patients.

Figure 2 - Patient 1. In A, preoperative appearance of reverse torsoplasty. In B, postoperative appearance 6 months after reverse torsoplasty.
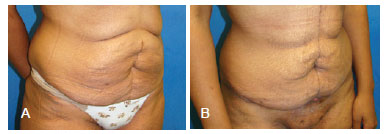
Figure 3 - Patient 2. In A, preoperative appearance of Fleur-de-Lis abdominoplasty. In B, postoperative appearance of Fleur-de-Lis abdominoplasty at 14 days, with dehiscence in the region where the scars meet ("T").
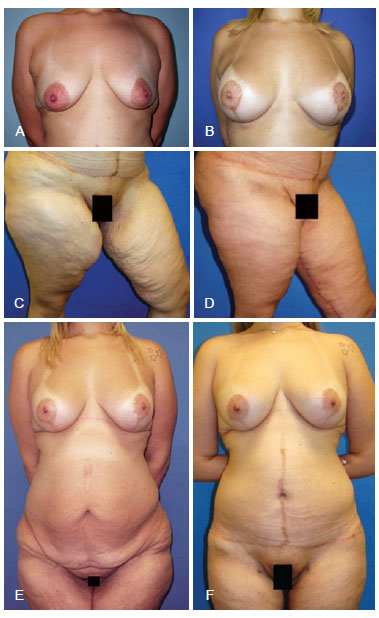
Figure 4 - Patient 3. In A, preoperative appearance of mammoplasty. In B, postoperative appearance at 1 year with mammoplasty with inclusion of 280 mL silicone implants. In C, preoperative appearance of crural dermolipectomy. In D, late postoperative appearance at 7 months after crural dermolipectomy. In E, postoperative appearance of mammoplasty with inclusion of silicone implants and preoperative Fleur-de-Lis abdominoplasty and cruroplasty. In F, late postoperative appearance following all operations (mammoplasty with inclusion of silicone implants, Fleur-de-Lis abdominoplasty, and cruroplasty).
DISCUSSION
Morbid obesity in adolescents is a very serious condition; moreover, its prevalence in the global population has increased13. Bariatric surgery appears to be the only treatment that has proven to be effective for morbid obesity4,5. Thus, bariatric surgery in this population requires a great amount of skill, and should be performed by experienced gastric surgeons or pediatric surgeons8. Moreover, the lack of a homogeneous group of patients who underwent bariatric surgery during their adolescence, with a prolonged follow-up, is a major limiting factors to performing a study with a larger sample size. Nevertheless, it is expected that the demand for plastic surgery for readjustment of body contours in patients who experience massive weight loss under these conditions will increase, resulting in the need for specific studies to analyze methods for obtaining better and long-term results.
Among the 5 patients studied, subjective criteria were used to decide the appropriate procedure for readjusting the body contour, taking into account the experience of the surgeon and the needs and desires of each patient.
Generic (sutures for closure, mechanical prophylaxis for deep venous thrombosis, prophylactic antibiotics, maintaining appropriate position and rest, and use of surgical meshes, among others) and specific (points of adhesion in areas with larger displacements and vacuum drainage, among others) systematizations were used in the surgical methodology in order to create a control strategy for local and systemic complications, based on the type of patient being treated.
We noted a 30% rate of local complications, which is consistent with that observed in the literature9-17. Among the complications, there were 3 (15%) cases of dehiscence; this constitutes the most frequent complication in some patient series, occurring in up to 30% of cases in some studies. Moreover, the need for secondary resection due to "residual" flaccid fatty-skin occurred in 3 (15%) surgical sites, which required rehospitalization and anesthesia.
We believe that the method of demarcation of tissue to be resected during surgery and retesting was effective in at least 70% of the sites operated on, considering that dehiscence occurred in only 15% of operated sites and residual flaccidity occurred in another 15% of operated sites, despite the possibility of interference from other factors in these types of complications, such as inadequate mobilization of the patient, histological factors inherent in the skin of ex-obese patients18,19.
Local complications such as seroma, hematoma, and infection were not observed in this study, probably due to the low number of patients. In the present study, it was not possible to obtain more comprehensive and significant values for morbidity and mortality associated with the procedures performed. Therefore, future studies should include a larger sample size.
CONCLUSIONS
Among the 5 patients included in this study who underwent bariatric surgery during their adolescence, we identified certain factors associated with body contouring plastic surgery, including index of dehiscence and residual flaccidity, which were comparable to those observed in the literature regarding the general population (i.e., not specific to a population that underwent bariatric surgery during adolescence). However, it was not possible to identify certain types of associated complications, possibly due to the small sample size.
REFERENCES
1. World Health Organization. European region: prevalence of overweight and obesity in children and adolescents. Fact Sheet 2.3, December 2009, Code: RPG2_Hous_E2. Disponível em: http://www.euro.who.int/_data/assets/pdf_file/0005/96980/2.3. Prevalence-of-overweightand-obesity-EDITED_layouted_V3.pdf Acesso em: 30/5/2012.
2. Mondini L, Levy RB, Saldiva SRDM, Venâncio SI, Aguiar JA, Stefanini MLR. Prevalência de sobrepeso e fatores associados em crianças ingressantes no ensino fundamental em um município da região metropolitana de São Paulo, Brasil. Cad Saúde Pública. 2007;23(8):1825-34.
3. Chaves VLV, Freese E, Lapa TM, Cesse EAP, Vasconcelos ALR. Evolução espaço-temporal do sobrepeso e da obesidade em adolescentes masculinos brasileiros, 1980 a 2005. Cad Saúde Pública. 2010;26(7):1303-13.
4. Capella JF, Capella RF. Bariatric surgery in adolescence: is this the best age to operate? Obes Surg. 2003;13(6):826-32.
5. Loux TJ, Haricharan RN, Clements RH, Kolotkin RL, Bledsoe SE, Haynes B, et al. Health-related quality of life before and after bariatric surgery in adolescents. J Pediatr Surg. 2008;43(7):1275-9.
6. Kim RJ, Langer JM, Baker AW, Filter DE, Williams NN, Sarwer DB. Psychosocial status in adolescents undergoing bariatric surgery. Obes Surg. 2008;18(1):27-33.
7. Zuelzer HB, Baugh NG. Bariatric and body-contouring surgery: a continuum of care for excess and lax skin. Plast Surg Nurs. 2007;27(1):3-13.
8. Velhote MC, Damiani D. Bariatric surgery in adolescents: preliminary 1-year results with a novel technique (Santoro III). Obes Surg. 2010;20(12):1710-5.
9. Greco JA 3rd, Castaldo ET, Nanney LB, Wendel JJ, Summitt JB, Kelly KJ, et al. The effect of weight loss surgery and body mass index on wound complications after abdominal contouring operations. Ann Plast Surg. 2008;61(3):235-42.
10. Vastine VL, Morgan RF, Williams GS, Gampper TJ, Drake DB, Knox LK, et al. Wound complications of abdominoplasty in obese patients. Ann Plast Surg. 1999;42(1):34-9.
11. Michaels J 5th, Coon D, Rubin JP. Complications in postbariatric body contouring: postoperative management and treatment. Plast Reconst Surg. 2011;127(4):1693-700.
12. Cintra W Jr, Modolin ML, Gemperli R, Gobbi CI, Faintuch J, Ferreira MC. Quality of life after abdominoplasty in women after bariatric surgery. Obes Surg. 2008;18(6):728-32.
13. Modolin M, Cintra W Jr, Gobbi CI, Ferreira MC. Circumferential abdominoplasty for sequential treatment after morbid obesity. Obes Surg. 2003;13(1):95-100.
14. Cintra Junior W, Modolin M, Gobbi CIC, Gemperli R, Ferreira MC. Abdominoplastia circunferencial em pacientes após cirurgia bariátrica: avaliação da qualidade de vida pelo critério adaptativo. Rev Bras Cir Plást. 2009;24(1):52-6.
15. Schmitt GL, Rios MP, Scopel SO, Saito FL, Marques M, Ferreira MC. Abdominoplastia no paciente após perda ponderal maciça: experiência de cinco anos em hospital público secundário. Rev Bras Cir Plást. 2010;25(supl.):41.
16. Salles AG, Ferreira MC, Remigio AFN, Gemperli R. Escala para avaliação de resultados de cirurgia estética do abdome. Rev Bras Cir Plást. 2011;26(1):147-50.
17. Furtado IR, Nogueira CH, Lima Júnior EM. Cirurgia plástica após a gastroplastia redutora: planejamento das cirurgias e técnicas. Rev Soc Bras Cir Plást. 2004;19(2):29-40.
18. Rasmussen MH, Jensen LT, Andersen T, Breum L, Hilsted J. Collagen metabolism in obesity: the effect of weight loss. Int J Obes Relat Metab Disord. 1995;19(9):659-63.
19. Orpheu SC, Coltro PS, Scopel GP, Gomez DS, Rodrigues CJ, Modolin ML, et al. Collagen and elastic content of abdominal skin after surgical weight loss. Obes Surg. 2010;20(4):480-6.
1. Assistant physician of the Department of Plastic Surgery, Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (Hospital das Clinicas, Faculty of Medicine, University of São Paulo - HCFMUSP), São Paulo, SP, Brazil.
2. Lecturer, Associate Professor of the Plastic Surgery Course of the Faculdade de Medicina da Universidade de São Paulo (School of Medicine of the Universidade de São Paulo), São Paulo, SP, Brazil.
3. PhD, Assistant physician, at the Department of Plastic Surgery of the Faculdade de Medicina da Universidade de São Paulo (School of Medicine, Universidade de São Paulo), São Paulo, SP, Brazil.
4. Associate professor of the Course in Pediatric Surgery of the Instituto da Criança do HCFMUSP (Children's Institute of HCFMUSP), São Paulo, SP, Brazil.
5. Full professor of Plastic Surgery of the Faculdade de Medicina da Universidade de São Paulo (School of Medicine, Universidade de São Paulo), São Paulo, SP, Brazil.
Correspondence to:
Rodrigo Itocazo Rocha
Rua Cubatão, 86 - cj. 310 - Paraíso
São Paulo, SP, Brazil - CEP 04013 -000
E-mail: rodrigoitocazo@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: June 19, 2012
Article accepted: October 4, 2012
This study was performed at the Department of Plastic Surgery of the Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (Hospital das Clínicas of the School of Medicine of the Universidade de São Paulo), São Paulo, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter