

Original Article - Year 2012 - Volume 27 -
Fournier's syndrome: a 10-year evaluation study
Síndrome de Fournier: 10 anos de avaliação
ABSTRACT
BACKGROUND: Fournier's gangrene is a synergistic necrotizing fasciitis of the perineum and abdominal wall that develops in the scrotum and penis in men and the vulva and groin in women. This disease was initially believed to be idiopathic; however, recent studies have indicated that it is a serious condition caused by gram-positive, gram-negative, or anaerobic bacteria. It is often associated with severe and fatal systemic involvement.
METHODS: A retrospective study involving a chart review of 23 patients with Fournier's syndrome treated between January 2002 and January 2012 was conducted. Prompt treatment consisted of broad-spectrum antibiotic administration and serial debridement. The reconstruction techniques ranged from edge approximation via simple sutures to the use of flaps and grafts in cases with extensive lesions.
RESULTS: The skin and scrotal reconstruction techniques were effective in all cases, yielding satisfactory aesthetic results. Three (13%) patients died, including 2 patients who had previous illnesses and comorbidities.
CONCLUSIONS: Although Fournier's syndrome is a serious disease, therapeutic measures such as prompt intervention, with early debridement and broad-spectrum antibiotic therapy, in a multidisciplinary approach is very effective for controlling the disease, enabling surgical reconstruction of the affected areas with a low mortality rate.
Keywords: Fournier gangrene. Fasciitis, necrotizing. Reconstructive surgical procedures/methods.
RESUMO
INTRODUÇÃO: A gangrena de Fournier é uma fasciite necrosante sinérgica do períneo e parede abdominal, que tem origem no escroto e pênis, no homem, e vulva e virilha, na mulher. O processo inicialmente foi descrito como idiopático, mas atualmente sabe-se que se trata de grave afecção causada por bactérias Gram positivas, Gram negativas ou anaeróbios, que pode levar a comprometimento sistêmico importante e, eventualmente, morte.
MÉTODO: Foi realizado estudo retrospectivo, baseado na análise de prontuários médicos de 23 pacientes portadores de síndrome de Fournier, no período de janeiro de 2002 a janeiro de 2012. O tratamento dos pacientes incluiu intervenção precoce, com antibioticoterapia de largo espectro e desbridamentos consecutivos. O procedimento terapêutico empregado para a reconstrução variou desde a aproximação das bordas com sutura simples até uso de retalhose enxertos, nas lesões extensas.
RESULTADOS: As técnicas de reparação cutânea foram eficientes e a reparação escrotal foi também efetiva em todos os casos, obtendo-se bons resultados estéticos. Houve 3 (13%) óbitos, 2 deles em pacientes com doenças pregressas e portadores de comorbidades.
CONCLUSÕES: Apesar da reconhecida gravidade da Síndrome de Fournier, as medidas terapêuticas adotadas, como rápida intervenção, desbridamento precoce e antibioticoterapia de amplo espectro, juntamente com abordagem multidisciplinar, demonstraram-se bastante eficazes no controle da doença, permitindo reconstrução cirúrgica das áreas atingidas, com baixa mortalidade.
Palavras-chave: Gangrena de Fournier. Fasciite necrosante. Procedimentos cirúrgicos reconstrutivos/métodos.
Fournier's gangrene is a synergistic necrotizing fasciitis of the perineum and abdominal wall; it develops in the scrotum and penis in men and the vulva and groin in women1,2 (Figure 1). Its pathophysiology is characterized by endarteritis obliterans followed by ischemia and thrombosis of the subcutaneous vessels; this results in skin necrosis as well as necrosis of subcutaneous and surrounding tissue (the infection does not typically cause necrosis but can invade the deep fascia and muscle), which creates an entry site for normal skin flora. As aerobic and anaerobic bacteria disseminate, the tissue oxygen concentration is reduced. Hypoxia and tissue ischemia affect metabolism and lead to increased dissemination of facultative microorganisms that use the cells' energy sources. The resultant gases (i.e., hydrogen and nitrogen) are responsible for the crepitation that occurs in the first 48 to 72 hours of infection3-5.

Figure 1 - Necrotizing fasciitis. In A, necrotizing fasciitis with exposed testicle and abundant necrotic tissue. In B, necrotizing fasciitis with pockets and confluent punctures.
In 1884, French venereologist JeanAlfred Fournier6 described 5 cases of patients with idiopathic gangrene of the penis and scrotum. In the original reports, Fournier describes 3 fundamental features of the clinical presentation: abrupt onset in previously healthy young men, rapid progression, and absence of a discernible cause7-11.
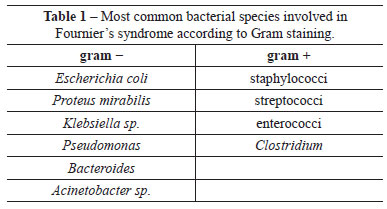
Studies demonstrate the presence of a variety of microorganisms in cultures of wound secretions and necrotic tissues. A polymicrobial flora is usually found, including gram-negative bacteria (e.g., Escherichia coli, Proteus mirabilis, Klebsiella sp., Pseudomonas, Bacteroides sp., Acinetobacter sp.), gram-positive bacteria (e.g., staphylococci, streptococci, enterococci, and Clostridium), and fungi12-15 (Table 1).
Contemporary case series indicate that Fournier's syndrome usually affects patients between the third and sixth decades of life with comorbidities such as debilitating conditions (e.g., malnutrition and sepsis); immunosuppression (e.g., diabetes mellitus, chronic alcoholism, underlying malignancy, AIDS, measles, chemotherapy, and leukemia); colorectal and urogenital diseases; postoperative complications (associatedwithurologic instrumentation use, herniorrhaphy, hemorrhoidectomy, orchiectomy, and prostatectomy), intravenous drug use; and trauma (e.g., local, mechanical, technical, and chemical) including bites, scratches, and vaginal and anal intercourse15-17.
METHODS
A retrospective study involving a chart review of 23 patients with Fournier's syndrome admitted to the department of plastic surgery of the Hospital Universitário da Universidade Federal de Juiz de Fora (Juiz de Fora, MG, Brazil) between January 2002 and January 2012 was performed.
The age of the patients ranged between 20 and 50 years.
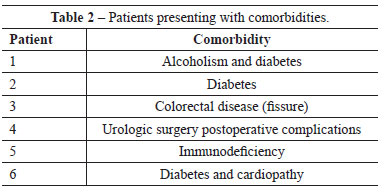
Six (26.1%) patients presented with the following comorbidities: alcoholism, diabetes, colorectal disease (fissure), postoperative complications following urologic surgery, immunodeficiency, and cardiopathy. The remaining patients did not have any comorbidities (Table 2).
Fournier's syndrome was diagnosed on the basis of aggressive infection progression, spread of gangrene to the area surrounding the scrotum, and systemic toxicity. The index proposed by Laor et al.18 was used to evaluate the severity of Fournier's syndrome. In that index, scoring is based on vital signs (i.e., body temperature, cardiac, and respiratory parameters) and laboratory parameters (i.e., sodium, potassium, hemogram, hematocrit, and white cell count).
Treatment
Broad-spectrum antibiotic therapy (maximum dose) against gram-positive, gram-negative, and anaerobic bacteria was initiated at diagnosis and maintained until complete clinical remission of the disease. The necrotic scrotal and perineal skin was incised or excised in the groin area, flanks, and abdominal wall. A final debridement was performed after the extent of necrosis was delineated.
Local wound care consisted of cleansing with antibacterial chlorhexidine and a topical antibacterial agent (1% silver sulfadiazine cream).
The exposed testicles were not removed or implanted in the groin; they were merely protected by moist wound-healing dressings or dressings with topical antibacterial ointment (Figure 2). Colostomy was performed in patients who did not exhibit involvement of the perianal areas.
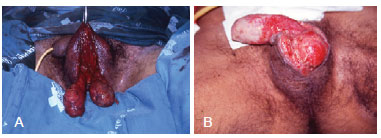
Figure 2 - In A and B, exposed testicles before reconstruction of the scrotal sac.
Surgical reconstruction was performed when the wound area showed no evidence of infection (i.e., negative culture findings, absence of toxemia, and healthy granulation tissue) and necrotic tissue was absent. Topical treatment was maintained until the wounds exhibited adequate granulation tissue for skin autografting or the use of flaps (Figure 3).

Figure 3 - Image prior to scrotal sac reconstruction after dressing with topical antibacterial agents.
The reconstruction procedures used were as simple as possible, ranging from edge approximation via simple sutures (Figure 4) to the use of flaps (Figure 5) and skin grafts in cases involving extensive lesions. In most cases, the residual tissues of the scrotal sac were sufficient for successful repair, given the elasticity and rich vascularization of this region (Figure 6).
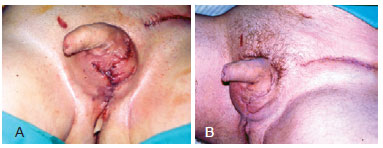
Figure 4 - In A and B, reconstruction of the scrotal sac using direct suture of residual tissue.
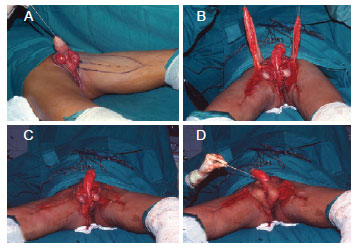
Figure 5 - Internal thigh fasciocutaneous flap. In A, marking of the fasciocutaneous flap. In B and C, created flaps. In D, flap rotation.
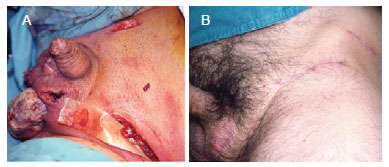
Figure 6 - In A, reconstruction of the scrotal sac using direct suture of residual tissue. In B, late postoperative appearance.
RESULTS
The mean time between hospital admission and the initiation of reconstructive procedures was 30 days.
The skin and scrotal reconstruction techniques were effective in all cases, yielding satisfactory aesthetic results (Figure 6).
Only minor complications were observed, such as suture dehiscence, partial flap necrosis, and partial graft loss. However, these did not compromise the final results. Three (13%) patients died, which included 2 of the 6 patients who had previous illnesses and comorbid conditions.
All patients reported being satisfied with the reconstruction outcome.
DISCUSSION
Available data indicate that the mortality rate associated with Fournier's syndrome is approximately 20%. In 1945, McCrea19 conducted an extensive review of 267 cases documented in the literature. Data collected between 1764 and 1945 indicated a 22% mortality rate. However, in the present 10-year evaluation study, the mortality rate was 13%, which indicates a substantial reduction in mortality16,20,21. The standardization of the integrated approach to patient care implemented in our hospital, including the development of a multidisciplinary team, is believed to have contributed to this improvement.
The medical procedures that improved the outcomes of this group of patients, as compared to the outcomes in the literature, include prompt diagnosis and intervention with broad-spectrum antibiotic therapy and serial debridement. The literature demonstrates the importance of debridement (the mortality rate in patients who do not undergo this procedure is 100%) and prompt intervention (gangrene spreads at 2.5 cm2/h)4,17,21. In Nigeria, Efem22 published a prospective study of 41 patients reporting better outcomes in patients who did not undergo serial debridement, but were instead treated with dressings.
Laor et al.18 note that the probability of death is 75% with a score > 9 as per their index, whereas a score of < 9 corresponds to a 78% probability of survival.
In the present study, reconstructive treatment was based on simple and effective techniques for each case and the affected area. Small defects were treated using edge-to-edge suture or skin autograft. Orchiectomy was not required in any of the cases. Testicle necrosis was rare because of the separate route of blood supply, which is provided by the spermatic vessels1,6,23-25.
Various types of flaps have been proposed for use in Fournier's syndrome26-29, including the thigh fasciocutaneous flap; it has appropriate thickness, ease of rotation, excellent aesthetic appearance, and rarely undergoes necrosis because of the rich vascularization provided by the internal pudendal and circumflex branches of the femoral artery. Therefore, it is a very safe flap to use, especially in patients with diabetes and vasculopathy. However, infertility may occur after the use of such flaps. Spermatogenesis depends on appropriate temperature conditions. Therefore, sperm cryopreservation before rotation of the thigh fasciocutaneous flap is recommended for patients who want to have children14.
Hyperbaric oxygen therapy is useful for the treatment of Fournier's syndrome as it removes exudates, promotes wound closure, enhances angiogenesis, and reduces bacterial contamination1,6,8,29,30. However, this therapy was not used in the present study because it was not available at the hospital.
CONCLUSIONS
Although Fournier's syndrome is a serious disease, therapeutic measures such as prompt intervention, early debridement, and broad-spectrum antibiotic therapy, along with a multidisciplinary approach, are very effective in the control of the disease and facilitate the surgical reconstruction of the affected areas with a low mortality rate.
REFERENCES
1. Korhonen K, Hirn M, Niinikoski J. Hyperbaric oxygen in the treatment of Fournier's gangrene. Eur J Surg. 1998;164(4):251-5.
2. Basoglu M, Gül O, Yildirgan I, Balik AA, Ozbey I, Oren D. Fournier's gangrene: review of fifteen cases. Am Surg. 1997;63(11):1019-21.
3. Cavalini F, Moriya TM, Pelá NTR. Síndrome de Fournier: a percepção do seu portador. Rev Esc Enferm USP. 2002;36(2):108-14.
4. Carvalho JP, Hazan A, Cavalcanti AG, Favorito LA. Relation between the area affected by Fournier's gangrene and the type of reconstructive surgery used. A study with 80 patients. Int Braz J Urol. 2007;33(4):510-4.
5. Roje Z, Roje Z, Matic D, Librenjak D, Dokuzovic S, Varvodic J. Necrotizing fasciitis: literature review of contemporary strategies for diagnosing and management with three case reports: torso, abdominal wall, upper and lower limbs. World J Emerg Surg. 2011;6(1):46.
6. Fournier AJ. Etude clinique de le gangrene foudroyante de la verge. Semaine Med. 1884;4:69.
7. Aboudib Junior JH. Sindrome de Fournier. Rev Bras Cir. 1986;76(1):7-11.
8. Bahlmann JC, Fourie IJ, Arndt TC. Fournier's gangrene: necrotizing fasciitis of the male genitalia. Br J Urol. 1983;55(1):85-8.
9. Jones RB, Hirschmann JV, Brown GS, Tremann JA. Fournier's syndrome: necrotizing subcutaneous infection of the male genitalia. J Urol. 1979; 122(3):279-82.
10. Lee C, Oh C. Necrotizing fasciitis of genitalia. Urology. 1979;13(6):604-6.
11. Ledingham IM, Tehrani MA. Diagnosis, clinical course and treatment of acute dermal gangrene. Br J Surg. 1975;62(5):364-72.
12. Lévy V, Jaffarbey J, Aouad K, Zittoun R. Fournier's gangrene during induction treatment of acute promyelocytic leukemia: a case report. Ann Hematol. 1998;76(2):91-2.
13. Mauro V. Retalho fasciocutâneo de região interna de coxa para reconstrução escrotal na síndrome de Fournier. Rev Bras Cir Plást. 2011;26(4):707-9.
14. Koukouras D, Kallidonis P, Panagopoulos C, Al-Aown A, Athanasopoulos A, Rigopoulos C, et al. Fournier's gangrene, a urologic and surgical emergency: presentation of a multi-institutional experience with 45 cases. Urol Int. 2011;86(2):167-72.
15. Candelária PAP, Klug WA, Capelhuchnik P, Fang CB. Síndrome de Fournier: análise dos fatores de mortalidade. Rev Bras Colo-proctol. 2009;29(2):197-202.
16. Mehl AA, Nogueira Filho DC, Mantovani LM, Grippa MM, Berger R, Krauss D, et al. Manejo da gangrena de Fournier: experiência de um hospital universitário de Curitiba. Rev Col Bras Cir. 2010;37(6):435-41.
17. Andrade ACH, Amarante MTJ, Ferreira MC, Lodovici O. Cirurgia reparadora na sequela da síndrome de Fournier. Rev Assoc Med Bras. 1991;37(1):22-6.
18. Laor E, Palmer LS, Tolia BM, Reid RE, Winter HI. Outcome prediction in patients with Fournier's gangrene. J Urol. 1995;154(1):89-92.
19. McCrea LE. Fulminating gangrene of the penis. Clinics. 1945:4:796-829.
20. Nakatani H, Hamada S, Okanoue T, Kawamura A, Chikai T, Yamamoto S, et al. Fournier's gangrene in elderly patient: report of a case. J Med Invest. 2011;58(3-4):255-8.
21. Gonzalez-Ulloa M. Severe avulsion of the scrotum in a bullfighter: reconstructive procedure. Br J Plast Surg. 1962;16:154-9.
22. Efem SE. Recent advances in the management of Fournier's gangrene: preliminary observations. Surgery. 1993;113(2):200-4.
23. Parkash S, Gajendran V. Surgical reconstruction of the sequelae of penile and scrotal gangrene: a plea for simplicity. Br J Plast Surg. 1984;37(3):354-7.
24. Silva C. Síndrome de Fournier. Rev Bras Cir. 1985;75(3):199-204.
25. Thomas JF. Fournier's gangrene of the penis and the scrotum. J Urol. 1956;75(4):719-27.
26. Westfall CT, Keller HB. Scrotal reconstruction utilizing bilateral gracilis myocutaneous flaps. Plast Reconstr Surg. 1981;68(6):945-7.
27. Batista RR, Ramacciotti Filho PR, Castro CAT, Fonseca MFM, Albuquerque IC, Formiga GJS. Síndrome de Fournier secundária a adenocarcinoma de próstata avançado: relato de caso. Rev Bras Colo-proctol. 2010;30(2):228-31.
28. Hallock GG. Scrotal reconstruction following Fournier gangrene using the medial circumflex femoral artery perforator flap. Ann Plast Surg. 2006;57(3):333-5.
29. Pizzorno R, Bonini F, Donelli A, Stubinski R, Medica M, Carmignani G. Hyperbaric oxygen therapy in the treatment of Fournier's disease in 11 male patients. J Urol. 1997;158(3 pt 1):837-40.
30. Hollabaugh RS Jr, Dmochowski RR, Hickerson WL, Cox CE. Fournier's gangrene: therapeutic impact of hyperbaric oxygen. Plast Reconstr Surg. 1998;101(1):94-100.
1. Plastic surgeon, full member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery) - SBCP, member of the clinical staff of the Department of Plastic Surgery, Hospital Universitário da Universidade Federal de Juiz de Fora (HU-UFJF), master in Health at UFJF, Juiz de Fora, MG, Brazil.
2. Plastic surgeon, full member of the SBCP, head of the Department of Plastic Surgery of the HU-UFJF, master in Health at UFJF, Juiz de Fora, MG, Brazil.
3. Medical student at the UFJF, intern at the Department of Plastic Surgery of the HU-UFJF, Juiz de Fora, MG, Brazil.
4. Medical student at the Faculdade de Ciências Médicas e da Saúde de Juiz de Fora (Suprema), Juiz de Fora, MG, Brazil.
5. Plastic surgeon, specialist member of the SBCP, Juiz de Fora, MG, Brazil.
Correspondence to:
Marilho Tadeu Dornelas
Rua Dom Viçoso, 20 - Alto dos Passos
Juiz de Fora, MG, Brazil - CEP 36026-390
E-mail: marilho.dornelas@ufjf.edu.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: August 1, 2012
Article accepted: October 30, 2012
This study was performed at the Department of Plastic Surgery, Hospital Universitário da Universidade Federal de Juiz de Fora,
Juiz de Fora, MG, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter