

Original Article - Year 2012 - Volume 27 -
Epidemiological study of burns in children treated at a tertiary hospital in São Paulo
Estudo epidemiológico de queimaduras em crianças atendidas em hospital terciário na cidade de São Paulo
ABSTRACT
BACKGROUND: This study describes the experience with the care of burned children in the Burn Treatment Unit, Division of Plastic Surgery, Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (Hospital of the Faculty of Medicine, University of São Paulo - HCFMUSP) over 15 consecutive months.
METHODS: The data of 98 patients up to 13 years of age treated in the Burn Treatment Unit of HCFMUSP from October 2009 to December 2010 were analyzed.
RESULTS: The average age of the children was 5.2 years; 67 (68.4%) were boys. Accidents were responsible for burns in 93 (94.9%) cases, whereas 1 (1%) case of burns was caused by aggression. There was a higher incidence of burns in children under 2 years of age. The main agent causing burns was hot liquids (48%), followed by fire (17%) and hot solids (17%). The mean body surface area affected by second-and third-degree burns was 10%. Six (6.1%) patients had burns over more than 20% of their body surface area - 5 (83.3%) of them had burns due to burning alcohol and 1 (16.7%) due to scalding water. All cases in which more than 30% of the body surface was affected by second- and third-degree burns were due to alcohol burns.
CONCLUSIONS: This survey demonstrates the importance of burn injuries in pediatric patients. The dataset suggests prevention efforts should focus on the domestic environment, particularly against scalding in children less than 5 years of age. In children older than 5 years, prevention programs should focus on both domestic and extradomestic environments.
Keywords: Burns. Child. Accident prevention.
RESUMO
INTRODUÇÃO: O objetivo deste estudo é descrever a experiência da Unidade de Tratamento de Queimados da Divisão de Cirurgia Plástica do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (HCFMUSP), em 15 meses consecutivos, no atendimento às crianças queimadas.
MÉTODO: Foram analisados os dados de 98 pacientes, com idade < 13 anos, atendidos na Unidade de Tratamento de Queimados do HCFMUSP, de outubro de 2009 a dezembro de 2010.
RESULTADOS: A média de idade das crianças atendidas foi de 5,2 anos, sendo 67 (68,4%) do sexo masculino. Os acidentes foram responsáveis por 93 (94,9%) casos, enquanto em 1 (1%) caso ocorreu agressão. Observou-se maior ocorrência de queimaduras em crianças com até 2 anos de idade. O principal agente da queimadura foi escaldadura (48%), seguido de fogo (17%) e sólido aquecido (17%). A média da superfície corpórea queimada de 2º e 3º graus foi de 10%. Seis (6,1%) pacientes apresentaram > 20% da superfície corpórea queimada, 5 (83,3%) deles por combustão de álcool e 1 (16,7%) por escaldo com água. Entre os 3 casos em que a superfície corpórea queimada de 2º e 3ºgraus foi > 30%, todos ocorreram por combustão de álcool.
CONCLUSÕES: O levantamento demonstra a importância da queimadura em pacientes da faixa etária pediátrica. O con-junto de dados obtidos permite inferir que os esforços de prevenção devem se concentrar no ambiente doméstico, contra a possibilidade de ocorrência de escaldaduras nas crianças com < 5 anos de idade. A partir dos 5 anos, as campanhas devem abordar tanto o ambiente doméstico como o extradoméstico.
Palavras-chave: Queimaduras. Criança. Prevenção de acidentes.
Child mortality in Brazil has declined greatly in recent decades. Moreover, its causes have changed as well. The decrease in the frequency of diarrheal and infectious diseases as causes of death resulted in a proportionate increase in perinatal causes (i.e., problems during pregnancy and childbirth) and external agents1. In Brazilian children between 1 and 14 years of age, external agents are the main causes of death. More than 5,000 children die, and approximately 137,000 are hospitalized annually according to the Ministry of Health, highlighting this serious public health problem1. Sequelae also have a significant impact. For every death, an estimated 4 children have permanent sequelae. According to the World Report on Preventing Accidents to Children and Adolescents released in December 2008 by the World Health Organization and UNICEF, 830,000 children die from accidents worldwide2,3. Domestic and automobile accidents as well as assault are among the top causes. However, there are no reliable statistics on the manner in which traumatic accidents occur. Burns can be classified as either due to aggression or accident.
This study describes the experience of the Burn Treatment Unit, Department of Plastic Surgery, Hospital das Clinicas, Faculty of Medicine, University of São Paulo (HCFMUSP) in the care of burned children over 15 consecutive months. The epidemiological profiles of the patients were evaluated, including the causative agent, and surface and body parts affected with second- and third-degree burns. In addition, treatments performed and prognoses were analyzed.
METHODS
We analyzed the data of all patients younger than 13 years treated between October 2009 and December 2010. During that period, 129 children with burns were treated (Figure 1). We excluded 31 cases with incomplete data, resulting in a total of 98 cases for analysis.
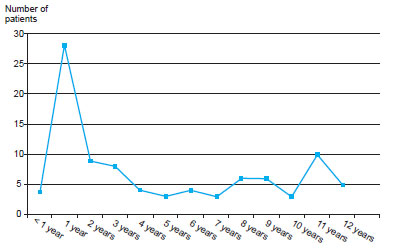
Figure 1 - Age distribution of the study population.
The following information was collected: date of burn occurrence, date of initial presentation at HCFMUSP, circumstance and mechanism of burn, body segments affected, percentage of body surface area burned, and eventual status of the patient (i.e., discharge, outpatient care, inpatient ward, or intensive care unit). The treatments performed were also analyzed, including dressing, debridement, escharotomy, fasciotomy, skin grafting, and amputation flaps. Among the hospitalized patients, the time between admission and discharge or death was also noted.
RESULTS
The mean age of the children examined was 5.2 years. Among a total of 98 children, there were 67 (68.4%) boys and 31 (31.6%) girls. The average duration between the time at which the burn occurred and admission at HCFMUSP was 68 hours, ranging from 1 to 160 hours.
Accidents were responsible for burns in 93 (94.9%) cases, whereas in 1 (1%) case, burns were caused due to aggression. The cause of the burn was unknown in 4 (4.1%) cases.
There was a higher incidence of burns in children under 2 years of age.
The causes and type of causative agent for all cases is presented in Table 1.
Scalding was the most prevalent cause among all age groups; it was slightly higher in children aged 1 to 5 years. Burns due to heated solids were predominant in patients under 1 year of age, and the incidence of this type of burn decreased with increasing age. In contrast, burns due to fire, explosions, and electrical trauma increased with increasing age (Figure 2).
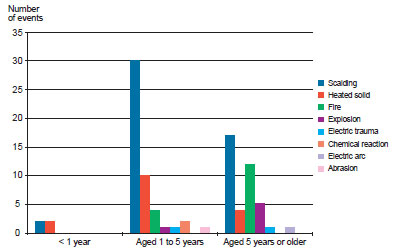
Figure 2 - Causes of burns by age group, as absolute number of events.
The mean body surface area affected by second- and third-degree burns was 10%. Six (6.1%) patients experienced burns over more than 20% of their body surface area; 5 (83.3%) had burns due to burning alcohol, and 1 (16.7%) had burns due to scalding water. All cases in which more than 30% of body surface area was affected by second- and third-degree burns were due to burning alcohol.
The upper limbs were affected in 53 (54.1%) cases, head and neck in 46 (46.9%), trunk in 45 (45.9%), lower limbs/perineum in 33 (33.7%), and airways in 1 (1%) (Figure 3).
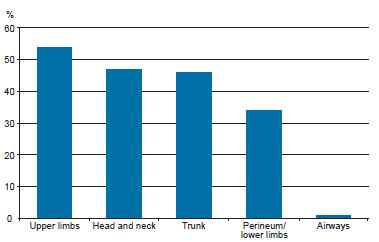
Figure 3 - Affected body areas as the percentage of total events.
Burns affecting the upper limbs were the most common in all age groups, especially among children between 1 and 4 years of age. Burns located on the trunk were present in 50% of cases in children up to 4 years of age, and occurred less frequently in children more than 5 years of age. Among the burns located on the head and neck, there were no cases in children less than 1 year of age. Such burns predominated in children aged 1 to 4 years, and decreased in children more than 5 years of age. Burns on the perineum and lower limbs were less prevalent in children less than 5 years of age but were the most frequent location for burns in children more than 5 years of age, along with burns on the upper limbs, and head and neck. Airway injuries were observed only in children more than 5 years of age (Figure 4).
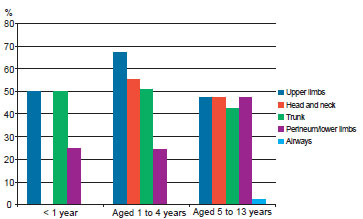
Figure 4 - Affected body regions by age group as the percentage of total events.
Of the patients admitted, 52 (53.1%) were discharged after initial treatment for subsequent outpatient follow-up, 27 (27.6%) were admitted to the ward, and 16 (16.3%) were admitted to the Intensive Care Unit (ICU) for burn treatment by specialists. Among the 16 patients in the ICU, 15 (93.8%) were discharged and 1 (6.2%) died.
The average hospitalization duration of all patients was 18 days. Among children hospitalized in the ICU, the average duration was 26 days.
Most patients (93 cases) were treated with occlusive dressings during initial care. In 5 cases, there was no need for bandages, because the body area affected by the burn was less than 1% of the body surface area. Dressing was the only treatment in 41 (41.8%) patients. The other 57 patients underwent procedures or surgical treatments such as surgical debridement in 51 cases (52%), skin grafting in 31 (31.6%), skin flap in 1 (1%), fasciotomy in 2 (2%), and escharotomy in (2%) (Figure 5).
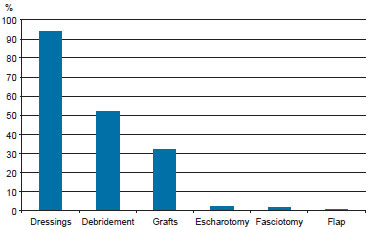
Figure 5 - Treatments as the percentage of the total number of cases.
Among the patients receiving skin grafts, meshed grafts were used in 15 (48.4%), slides in 14 (45.2%), and mixed grafts with mesh and blades in 2 (6.4%) patients. The mean body surface areas affected by second- and third-degree burns among patients treated with blade and meshed grafts were 10.9% and 10.2%, respectively. The 2 patients who received both types of grafts had burns on 22% and 42% of their body surface area (Figure 5).
DISCUSSION
In Brazil, there are no accurate statistics on the incidence of burns in children. In some developing countries, burns are among the leading causes of morbidity and mortality in children4,5. In this context, understanding the most frequent causes may aid in the development of a health policy to prevent burns, as well as guidelines for all phases of treatment and rehabilitation6.
Shani et al.7 studied different populations in Israel and recommended programs for burn prevention tailored to each population, taking into consideration their habits and seasonal variability in burn incidence.
The present data from the experience of a burn treatment unit located within a tertiary hospital in São Paulo may aid the planning of policies for the prevention and treatment of children experiencing burns.
Although located in a high complexity hospital, the Burn Treatment Unit serves patients admitted from other units at all levels of healthcare as well as patients seeking hospital care, as needed. Thus, the analyzed sample is similar to that of other units in the country. The spontaneous seeking of care is primarily demonstrated by the simple cases. Fifty-two patients were discharged after treatment in the emergency room, and 41 patients received dressings as the sole treatment. In patients undergoing surgery, treatment almost always involved the use of partial-thickness skin grafting.
In the population of children studied, the majority of treatments were performed on children between 1 and 5 years of age. This corroborates the data reported in other studies. Cheng et al.8 analyzed 1,704 burned children and found that children aged 1 to 2 years have the highest risk of burns. Moreover, Mashreky et al.4 report that children aged 1 to 4 years have the highest risk of burns. Furthermore, Cuenca-Pardo et al.9 analyzed the data of 1,025 burned children and found that younger age was associated with a higher risk of burns. This age group is more likely associated with burns due to the general neurodevelopment of children. After the stage where the child is completely dependent on adults is completed, the child begins to walk and experience the world with much more freedom. Parents should be vigilant during this stage, because household scalding accidents with agents such as oil and water are more common at this age. Unattended children can come into contact with flammable and toxic substances such as alcohol.
Up to 1 year of age, a child is almost completely dependent on an adult. During this time, burns usually occur due to the negligence of the adult. At this age, the most frequently observed type of burn was located on the trunk and caused by a hot liquid.
Children aged 1 year indicated an increased occurrence of burns in the present study. As mentioned above, at this age, children begin to walk and explore the environment around them; this often coincides with their mothers returning to work, which means that children are left at daycare or at home with individuals other than their parents. The importance of hot liquid as a causative agent of burns has been widely explored in other studies10.
Children aged 5 to 13 years had the greatest extent of body surface area burned, predominantly due to alcohol burns. This is probably because children at this age become increasingly independent and active outside the domestic environment and may come into contact with fireworks, alcohol, and electrical equipment, among other hazards. Combustion burns, explosions, and electrical injuries start occurring more frequently at this time.
The gender distribution of children with burns is similar to that reported in the literature5,8,11,12. Boys exhibit a higher incidence of burns, probably because of differences in behavior and activity between genders. Badger et al.13 studied the presence of attention deficit hyperactivity disorders in burned children and conclude that children with these disorders have an increased risk of experiencing burns.
Werneck & Reichenheim14 published a study correlating the risk of burns to the family environment. They report that households with many children, mothers who were pregnant or had recently lost jobs, and change of residence are factors that increase the risk of burns in children. Although the present study did not analyze the family environment, such information can also be useful for planning prevention campaigns.
The average age of the children admitted in the present study was 5.2 years, with the highest incidence observed among children aged more than 1 year. The most frequent cause of burns in this age group was hot liquid, whereas children aged 5 to 13 years were most often affected by combustion explosions and electrical trauma.
Most children did not require hospitalization and only received specific curative treatment. However, half of the children in the present study required hospitalization, and at least 1 required surgical intervention. In this group of patients, morbidity and the possibility of sequelae had a major impact.
CONCLUSIONS
This analysis highlights the importance of burn injuries in pediatric patients, especially those caused by scalding and burning alcohol. This dataset suggests that prevention efforts should focus on ensuring that the domestic environment does not provide opportunities for scalding in children aged less than 5 years. In children older than 5 years, prevention campaigns should focus on both domestic and extradomestic environments.
REFERENCES
1. Ministério da Saúde. Datasus [homepage na internet]. Disponível em www.datasus.gov.br Acesso em: 12/12/2011.
2. Organização Mundial da Saúde. [homepage na internet]. Disponível em www.who.int Acesso em: 12/12/2011.
3. Abib SCV. Prevenção de acidentes com crianças. I Fórum de Prevenção de Acidentes com Crianças, São Paulo, Brasil, 2004.
4. Mashreky SR, Rahman A, Chowdhury SM, Giashuddin S, Svanstrom L, Linnan M, et al. Epidemiology of childhood burn: yield of largest community based injury survey in Bangladesh. Burns. 2008;34(6):856-62.
5. Albertyn R, Bickler SW, Rode H. Paediatric burn injuries in Sub Saharan Africa: an overview. Burns. 2006;32(5):605-12.
6. Piccolo NS. The 2002 Everett Idris Evans Memorial Lecture. Burn care in Brazil: ideas from the past, trends of the present, and hopes for the future. J Burn Care Rehabil. 2002;23(6):385-400.
7. Shani E, Bahar-Fuchs SA, Abu-Hammad I, Friger M, Rosenberg L. A burn prevention program as a long-term investment: trends in burn injuries among Jews and Bedouin children in Israel. Burns. 2000;26(2):171-7.
8. Cheng JC, Leung KS, Lam ZC, Leung PC. An analysis of 1704 burn injuries in Hong Kong children. Burns. 1990;16(3):182-4.
9. Cuenca-Pardo J, Jesús Alvarez-Díaz C, Comprés-Pichardo TA. Related factors in burn children. Epidemiological study of the burn unit at the "Magdalena de las Salinas" Traumatology Hospital. J Burn Care Res. 2008;29(3):468-74.
10. Lacerda LA, Carneiro AC, Oliveira AF, Gragnani A, Ferreira LM. Estudo epidemiológico da Unidade de Tratamento de Queimaduras da Universidade Federal de São Paulo. Rev Bras Queimaduras. 2010;9(3):82-8.
11. Istre GR, McCoy M, Carlin DK, McClain J. Residential fire related deaths and injuries among children: fireplay, smoke alarms, and prevention. Inj Prev. 2002;8(2):128-32.
12. Ying SY, Ho WS. Playing with fire: a significant cause of burn injury in children. Burns. 2001;27(1):39-41.
13. Badger KL, Anderson RJ, Kagan RJ. Attention deficit-hyperactivity disorder in children with burn injuries. J Burn Care Res. 2008;29(5):724-9.
14. Werneck GL, Reichenheim ME. Paediatric burns and associated risk factors in Rio de Janeiro, Brazil. Burns. 1997;23(6):478-83.
1. Mentoring Physician of the Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (Hospital of the Faculty of Medicine, University of São Paulo - HCFMUSP), physician assistant to Plastic Surgery Servidor Público Estadual de São Paulo (Services of the Hospital for State Civil Servants of St. Paulo), associate member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery) - SBCP, São Paulo, SP, Brazil.
2. Lecturer at the Faculdade de Medicina da Universidade de São Paulo (Faculty of Medicine, University of São Paulo - FMUSP), associate professor of FMUSP, full member of the SBCP, São Paulo, SP, Brazil.
3. Resident of Plastic Surgery of HCFMUSP, São Paulo, SP, Brazil.
4. Ph.D., Technical Director of the Division of Plastic Surgery and Burns of HCFMUSP, associate member of the SBCP, São Paulo, SP, Brazil.
5. Professor, Chief of the Division of Plastic Surgery and Burns of HCFMUSP, full member of the SBCP, São Paulo, SP, Brazil.
Correspondence to:
Lincoln Saito Millan
Av. Doutor Enéas Carvalho de Aguiar, 255 - 8º andar - sala 8128
São Paulo, SP, Brazil - CEP 05403-900
E-mail: lincolnsaito@gmail.com
This study was performed at the Division of Plastic Surgery and Burns of the Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (Hospital das Clinicas, Faculty of Medicine, University of São Paulo), São Paulo, SP, Brazil.
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: July 24, 2012
Article accepted: October 15, 2012


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter