

Reviw Article - Year 2012 - Volume 27 -
Breast fat grafting: experimental or established procedure?
Lipoenxertia nas mamas: procedimento consagrado ou experimental?
ABSTRACT
There has recently been an increase in the use of fat grafting for the correction of congenital or acquired breast deformities and for aesthetic breast treatment. This increase is due to the emergence of novel fat grafting techniques that produce lasting and reliable results despite some authors' beliefs that the procedure might hinder breast cancer screening. This literature review aims to identify the most frequently used breast fat grafting techniques, evaluate their efficacy and safety, and report their major complications. The review was performed after a search in the PubMed and LILACS databases, and only English-language articles published over the past 5 years were assessed. There have been an increased number of studies on the topic in recent years, and a specific fat grafting technique has been primarily reported. Most studies in this area have shown that breast fat grafting does not affect radiological breast cancer screening, whereas some studies have suggested that the use of grafted fat may enhance the development of breast cancer. Despite the increased number of published studies, few have a good level of scientific evidence. This review concludes that fat grafting is an alternative technique for the correction of breast deformities and moderate aesthetic breast enlargement and should be performed by properly trained surgeons accompanied by a radiology team that is experienced in breast imaging. Further studies with appropriate scientific methodologies are needed to evaluate breast fat grafting.
Keywords: Breast fat grafting. Fat graft.
RESUMO
Atualmente vem ocorrendo aumento da incidência de utilização de enxertia de gordura para correção de defeitos mamários congênitos ou adquiridos e para tratamento mamário estético. Esse aumento é decorrente do surgimento de novas técnicas de lipoenxertia, que produzem resultados mais duradouros e confiáveis, apesar da crença de alguns autores de que o procedimento possa dificultar o rastreamento do câncer mamário. Esta revisão de literatura tem como objetivo identificar as técnicas de lipoenxertia mamárias mais utilizadas, avaliá-las quanto à eficácia e à segurança, e relatar as principais complicações associadas. A revisão foi realizada nas bases de dados PubMed e LILACS, e os fatores de inclusão foram: artigos em idioma inglês, publicados nos últimos cinco anos. Como resultado observou-se aumento do número de trabalhos abordando o tema nos últimos anos, e predomínio de uma técnica de lipoenxertia específica. A maioria dos trabalhos demonstra que a lipoenxertia mamária não prejudica o rastreamento radiológico para câncer mamário, e alguns sugerem que a gordura enxertada potencializa o desenvolvimento de câncer nas mamas. Apesar do aumento do número de trabalhos, existem ainda poucos com bom nível de evidência científica. Esta revisão permitiu concluir que a lipoenxertia é uma técnica alternativa para reparação de defeitos mamários e discreto aumento estético das mamas, devendo ser utilizada por cirurgiões com treinamento adequado e acompanhada por equipe de radiologia experiente em imagenologia mamária. Mais trabalhos com metodologia científica adequada são necessários para avaliar a lipoenxertia mamária.
Palavras-chave: Lipoenxertia mamária. Enxerto de gordura.
Autologous fat grafts have long been used as a filling material to correct soft tissue defects. One of the first reports on fat grafting described a case of breast defect correction1. Fat is considered an ideal filling material since it is autologous, easily accessed, widely abundant in the body, and has low immunogenic and allergic reactivity2. However, fat grafts often have high rates of resorption and replacement with fibrous scar tissue or calcified oil cysts, which can generate aftereffects and result in difficulties in interpreting radiological breast images3.
Publications on this subject are increasing due to the development of new techniques for fat harvest, preparation, and grafting, despite the belief of some authors that the procedure may hinder breast cancer screening3. Novel techniques have been developed to improve the viability and aesthetic results of fat grafts2,4,5. Fat grafting, which has primarily been used to correct breast deformities, has also been used for aesthetic purposes and to increase breast volume in an attempt to replace the use of breast implants6-8.
Several studies have shown that fat grafting did not effectively hinder radiological breast screening2,9-16. However, Wang et al.17 challenge these findings. In cases in which fat grafting is used for breast reconstruction after mastectomy or breast conservation therapy, new concerns have arisen regarding the possibility that the transplanted cells stimulate carcinogenesis in breasts with a predisposition to developing cancer18,19.
In this context, this literature review aims to identify the main techniques used for breast fat grafting, evaluate their efficacy and safety, and report their results and associated complications.
METHODS
Article Selection Process
An article search was performed in the PubMed and LILACS databases using the following key words: "breast fat graft", "breast fat transplantation", "breast adipose tissue injection", "breast lipomodelling", and "breast lipofilling". The number of articles retrieved per keyword was 37, 35, 151, 4, and 11, respectively.
Articles published in the last 5 years (between 2006 and 2011) in English were selected. We included all original articles indexed between January 2006 and November 2011, including experimental (clinical trials, randomized or not) and observational studies (case-control, cohort studies) performed in humans. Duplicate references were excluded, as were articles "ahead of print," reviews, letters to the editor, and editorials.
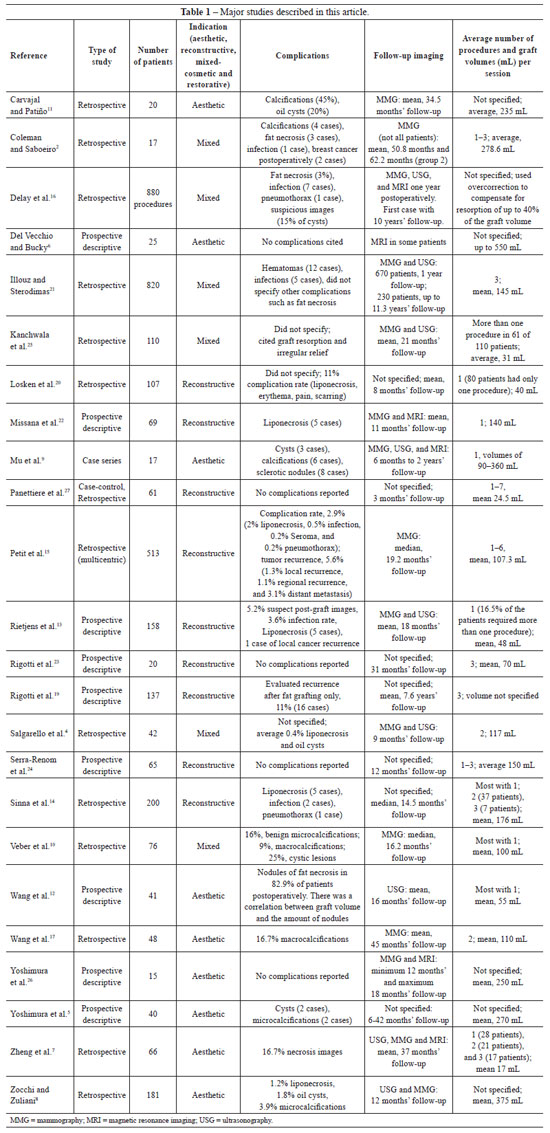
A total of 24 studies were assessed for study design, number of patients, indication for surgery, surgical technique, complications, follow-up imaging, and oncological follow-up.
RESULTS
After the selected articles were analyzed, we noted that the number of publications had grown in recent years (Figure 1). The studies were mostly retrospective (n = 13) or prospective and descriptive (n = 10), and there were no randomized controlled studies.
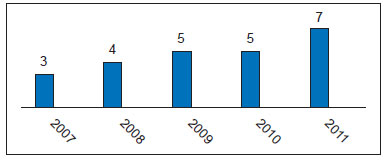
Figure 1 - Number of publications on fat grafting by publication year.
Studies involving large numbers of patients involved retrospective analyses of medical records or prospective evaluations of patients undergoing a specific technique and did not allow for an overall assessment of fat grafting8,13-16,19-21. The publications mentioned various techniques for obtaining, treating, and grafting fat. The main differences between the techniques were present in the treatment of the obtained fat (Figure 2). The studies generally reported that the grafts must be obtained by liposuction using the tumescent technique from body areas with an abundance of fat tissue (abdomen, flank, inner thigh, lateral thigh, medial knees, and back, as the commonly-used donor areas, in descending order)2,13-16,20,21.
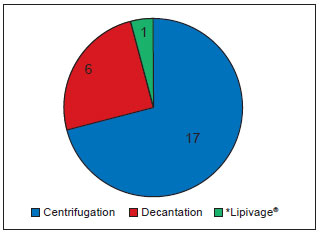
Figure 2 - Distribution of published studies according to fat preparation technique. *Closed system for collecting, washing, and transferring fat.
Most of these studies emphasized that liposuction should be gentle, involve the use of syringes or a low-pressure apparatus, and avoid exposure of the fat to ambient air (closed technique) to ensure that the fatty material is handled as little as possible2-8,13-16,19-24. The obtained fat should then be purified using low-speed centrifugation (Figure 2).
Fat grafting is performed through small cannulas in small quantities, and retroinjection occurs after tunnels are established using the cannulas. More fat grafting procedures emphasize that the grafting of fat should be performed using small quantities to ensure that the grafted tissue is in full contact with the vascularized tissue of the receptor region2,16,21.
In most of the studies, repeated fat grafting procedures were used to obtain the desired results, and an average of 3 procedures were required per patient (Table 1). However, some papers presented techniques for performing larger grafts and fewer procedures5,6,8,25,26. All studies that evaluated breast reconstruction after radiotherapy noted that additional fat grafting procedures are required23-25,27.
No conclusive studies have examined the percentage of fat remaining after the procedure. Most studies estimate that 30%-40% of the volume is lost after the first procedure, thus requiring subsequent procedures5,21,22,25,26 or graft over-correction14,16,25.
Several studies have shown high rates of patient satisfaction after fat grafting as well as good aesthetic results that are subjectively evaluated using photographs2,5-8,14,16,20-24.
These studies considered breast fat grafting as a safe technique with a low number of major complications (Table 1). The main complications of most studies were liponecrosis and oil cyst formation (Table 1), whereas local infection of the grafted area2,13-15,21 occurred in a few cases. Most studies reported no difficulty with radiological breast screening after fat grafting procedures. Screening was conducted primarily using mammography and breast ultrasonography4,7,8,10-13,15,16,21,22,25,26 by radiology teams experienced in discerning images of benign and malignant breast calcification4,7,13,15,16,21. All tissues with suspected abnormal radiological findings were biopsied, which revealed a low number of malignant disease confirmations7-12,16,17,22. Rietjens et al.13 concluded that the only case of recurrence detected in their study was likely due to underdiagnosis of the initial cancer. Petit et al.15 and Ilouz and Sterodimas21 stated that the number of cancer cases detected after fat grafting was similar to the cancer incidence in the general population, although they did not present data on this statement in their studies. Rigotti et al.19 found a similar incidence of tumor recurrence in patients treated with fat grafting compared to patients who did not receive fat grafting treatment. However, their comparison of the same group of patients at different time windows has been criticized by other authors15.
After a review of studies in vitro and in animals confirmed their hypothesis, Lohsiriwat et al.18 hypothesized that fat grafting in predisposed breasts could lead to carcinogenesis but concluded that there is insufficient evidence for this association in humans.
DISCUSSION
Fat grafting is a widely used and established technique that is used to correct soft tissue deformities1. Nevertheless, it is no longer used by some surgeons as a result of the large resorption of graft material, the loss of results, and calcification and oil cyst formation within the graft. This could possibly interfere with radiological follow-up of the breasts, thereby affecting the diagnosis of new breast tumors or recurrences3. With the development of new techniques for obtaining, processing, and grafting fat material2, more durable grafts could be obtained initially, thus presenting good results in the correction of soft tissue defects of the face and subsequently in other locations such as the breast. Coleman & Saboeiro2 questioned the restriction on the use of fat grafting by the American Society of Plastic and Reconstructive Surgery in 19873 and argued that the same regions of calcifications and liponecrosis that are observed after fat grafting procedures are also observed after other breast procedures such as breast reduction and mastopexy. According to this study, the number of published studies on breast fat grafting have increased in recent years. Despite this increase, few questions have been answered scientifically, primarily because most studies were related to case series or reports of new techniques and had small numbers of patients. Moreover, few observational, case-control26, or large studies have been performed.
Fat grafting was used mainly in cases of breast reconstruction, particularly to correct deformities after primary reconstructions13-15,16,20,22 or adjuvant treatments such as radiotherapy19,23,27 (Table 1). Some articles mention its use to correct deformities after aesthetic surgeries, such as breast augmentation and mammoplasty5,21,26, and others describe the use of fat grafting for aesthetic breast augmentation, as an alternative to prostheses use6-9.
Several studies have emphasized that the fat must be collected and purified through low-pressure liposuction, which is usually performed using syringes, to minimize the resultant trauma to the autologous material being collected. Moreover, prolonged contact between the fat and the air must be avoided, and the samples should be purified by low-speed centrifugation or decantation. Purified fat grafts are then constructed through the use of smaller cannulas in small portions or amounts such that the graft material maintains maximum contact with the receptor tissue and its blood vessels. This protocol ensures appropriate nutrition in the early days after grafting. The same reasoning is used for fat grafts in the tissue after radiotherapy, when vascularization is scarce but the graft still shows good results19,23.
Although several studies have shown good results through photographs and high levels of satisfaction by patients and surgeons, few have quantified the percentage of grafted fat that did not undergo resorption, degeneration, or necrosis. Some authors recommended overcorrection to allow for resorption14,16,25. Del Vecchio & Bucky6 evaluated the amount of graft absorbed by comparing magnetic resonance imaging (MRI) of the breast before and after the procedure, indicating that this can be a good tool to evaluate fat graft absorption. However, in their study, tests were not performed on all patients since they were asked to finance them, thus affecting the final assessment of this variable. Most surgeons subjectively estimate the amount of fat that is needed to correct the defect and state that the fat grafting procedure should be performed in more than one step, particularly in cases of reconstruction after radiotherapy.
Most of these studies cited a low number of complications. Liponecrosis and oil cyst formation comprise the most common complications, followed by local infection of the graft material. Despite a considerable number of liponecrosis events and oil cysts after the breast fat grafting process, most studies concluded that these images appear benign when evaluated by a radiologist who is experienced in mammography or breast ultrasonography2,7,9-16,21. Results that generate doubts should be better evaluated using MRI or guided breast biopsy7,9,15,16,22,25. Some studies report that the number of liponecrosis events was higher at the beginning of the series, and following the development of more suitable fat grafting techniques, the number of liponecrosis events underwent a significant reduction that approached zero16.
Coleman and Saboeiro2 mentioned that the number of suspect images after breast fat grafting is similar to that of post-operative breast surgeries such as mastopexy and breast reduction. Wang et al.17 challenged the published studies and concluded that the calcifications observed after fat grafting in the breast can be a confounding factor in the diagnosis of future breast cancer. In their study, the fat grafting technique is not very detailed, but it is inferred that, although the authors used a moderate amount of fat in each procedure (mean, 110 mL), the grafts were introduced in large increments and required a "massage" after grafting to accommodate the graft, which would result in a higher rate of necrosis in the central portion of the grafts12.
Although some experimental studies in vitro and in animals suggested that fat grafting could lead to cancer18, no studies have properly evaluated a cause and effect relationship between breast fat grafting and cancer in humans. Some studies have reported on the incidence or recurrence of breast cancer events after fat grafting but did not draw conclusions about the causal effect. Most of the cases observed were attributed to "underdiagnosis" of the initial cancer, which would have occurred regardless of the fat grafting13,15,16.
CONCLUSIONS
Although none of the analyzed studies have indicated a high level of scientific evidence, fat grafting seems to be an adequate and safe technique to repair breast deformities and is a good alternative to moderate aesthetic breast enlargement. Fat grafting presents a low number of complications when performed by experienced professionals and yields good results and high levels of patient satisfaction. It should be performed by well-trained breast grafting teams, and patients should be monitored by an experienced breast imaging radiology team.
Issues regarding the effective evaluation of the integration of the graft with the breast tissue, the percentage of graft resorption according to the technique used, and the long-term changes in graft material as well as their influence on the grafted area have yet to be addressed and require randomized studies with larger numbers of patients and a better scientific design.
REFERENCES
1. Czerny V. Plastischer ersatz der brustdruse durch ein lipom. Zentralbl Chir.1895;27-72.
2. Coleman SR, Saboeiro AP. Fat grafting to the breast revisited: safety and efficacy. Plast Reconstr Surg. 2007;119(3):775-85.
3. ASPRS Ad-Hoc Committee on New Procedures. Report on autologous fat transplantation. Plast Surg Nurs. 1987;7(4):140-1.
4. Salgarello M, Visconti G, Rusciani A. Breast fat grafting with platelet-rich plasma: a comparative clinical study and current state of the art. Plast Reconstr Surg. 2011;127(6):2176-85.
5. Yoshimura K, Sato K, Aoi N, Kurita M, Hirohi T, Harii K. Cell-assisted lipotransfer for cosmetic breast augmentation: supportive use of adipose-derived stem/stromal cells. Aesthetic Plast Surg. 2008;32(1):48-55.
6. Del Vecchio DA, Bucky LP. Breast augmentation using preexpansion and autologous fat transplantation: a clinical radiographic study. Plast Reconstr Surg. 2011;127(6):2441-50.
7. Zheng DN, Li QF, Lei H, Zheng SW, Xie YZ, Xu QH, et al. Autologous fat grafting to the breast for cosmetic enhancement: experience in 66 patients with long-term follow up. J Plast Reconstr Aesthet Surg. 2008;61(7):792-8.
8. Zocchi ML, Zuliani F. Bicompartmental breast lipostructuring. Aesthetic Plast Surg. 2008;32(2):313-28.
9. Mu DL, Luan J, Mu L, Xin MQ. Breast augmentation by autologous fat injection grafting: management and clinical analysis of complications. Ann Plast Surg. 2009;63(2):124-7.
10. Veber M, Tourasse C, Toussoun G, Moutran M, Mojallal A, Delay E. Radiographic findings after breast augmentation by autologous fat transfer. Plast Reconstr Surg. 2011;127(3):1289-99.
11. Carvajal J, Patiño JH. Mammographic findings after breast augmentation with autologous fat injection. Aesthet Surg J. 2008;28(2):153-62.
12. Wang H, Jiang Y, Meng H, Zhu Q, Dai Q, Qi K. Sonographic identification of complications of cosmetic augmentation with autologous fat obtained by liposuction. Ann Plast Surg. 2010;64(4):385-9.
13. Rietjens M, De Lorenzi F, Rossetto F, Brenelli F, Manconi A, Martella S, et al. Safety of fat grafting in secondary breast reconstruction after cancer. J Plast Reconstr Aesthet Surg. 2011;64(4):477-83.
14. Sinna R, Delay E, Garson S, Delaporte T, Toussoun G. Breast fat grafting (lipomodelling) after extended latissimus dorsi flap breast reconstruction: a preliminary report of 200 consecutive cases. J Plast Reconstr Aesthet Surg. 2010;63(11):1769-77.
15. Petit JY, Lohsiriwat V, Clough KB, Sarfati I, Ihrai T, Rietjens M, et al. The oncologic outcome and immediate surgical complications of lipofilling in breast cancer patients: a multicenter study: Milan-Paris-Lyon experience of 646 lipofilling procedures. Plast Reconstr Surg. 2011;128(2):341-6.
16. Delay E, Garson S, Tousson G, Sinna R. Fat injection to the breast: technique, results, and indications based on 880 procedures over 10 years. Aesthet Surg J. 2009;29(5):360-76.
17. Wang CF, Zhou Z, Yan YJ, Zhao DM, Chen F, Qiao Q. Clinical analyses of clustered microcalcifications after autologous fat injection for breast augmentation. Plast Reconstr Surg. 2011;127(4):1669-73.
18. Lohsiriwat V, Curigliano G, Rietjens M, Goldhirsch A, Petit JY. Autologous fat transplantation in patients with breast cancer: "silencing" or "fueling" cancer recurrence? Breast. 2011;20(4):351-7.
19. Rigotti G, Marchi A, Stringhini P, Baroni G, Galiè M, Molino AM, et al. Determining the oncological risk of autologous lipoaspirate grafting for post-mastectomy breast reconstruction. Aesthetic Plast Surg. 2010;34(4):475-80.
20. Losken A, Pinell XA, Sikoro K, Yezhelyev MV, Anderson E, Carlson GW. Autologous fat grafting in secondary breast reconstruction. Ann Plast Surg. 2011;66(5):518-22.
21. Illouz YG, Sterodimas A. Autologous fat transplantation to the breast: a personal technique with 25 years of experience. Aesthetic Plast Surg. 2009;33(5):706-15.
22. Missana MC, Laurent I, Barreau L, Balleyguier C. Autologous fat transfer in reconstructive breast surgery: indications, technique and results. Eur J Surg Oncol. 2007;33(6):685-90.
23. Rigotti G, Marchi A, Galiè M, Baroni G, Benati D, Krampera M, et al. Clinical treatment of radiotherapy tissue damage by lipoaspirate transplant: a healing process mediated by adipose-derived adult stem cells. Plast Reconstr Surg. 2007;119(5):1409-22.
24. Serra-Renom JM, Muñoz-Olmo JL, Serra-Mestre JM. Fat grafting in postmastectomy breast reconstruction with expanders and prostheses in patients who have received radiotherapy: formation of new subcutaneous tissue. Plast Reconstr Surg. 2010;125(1):12-8.
25. Kanchwala SK, Glatt BS, Conant EF, Bucky LPAutologous fat grafting to the reconstructed breast: the management of acquired contour deformities. Plast Reconstr Surg. 2009;124(2):409-18.
26. Yoshimura K, Asano Y, Aoi N, Kurita M, Oshima Y, Sato K, et al. Progenitor-enriched adipose tissue transplantation as rescue for breast implant complications. Breast J. 2010;16(2):169-75.
27. Panettiere P, Marchetti L, Accorsi D. The serial free fat transfer in irradiated prosthetic breast reconstructions. Aesthetic Plast Surg. 2009;33(5):695-700.
Correspondence to:
Alexandre Roriz Blumenschein Instituto de Mastologia e Oncologia Alameda das Rosas, 533 - Setor Oeste
Goiânia, GO, Brazil - CEP 74110-060
E-mail: ablumenschein@hotmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: February 8, 2012
Article accepted: June 7, 2012
This study was performed at the Faculdade de Medicina da Universidade Federal de Goiás (Faculty of Medicine of the Federal University of Goiás), Goiânia, GO, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter