

Case Report - Year 2012 - Volume 27 -
Congenital midline cervical cleft
Fissura congênita cervical da linha média
ABSTRACT
Congenital midline cervical cleft is a deformity known by several names. Although its embryologic origin has not been clearly established, the most widely accepted etiology is impaired midline fusion of the distal branchial arches. The main characteristic of this malformation is a protruding lesion at the midline of the anterior neck, between the chin and the suprasternal notch. Complete surgical resection of the lesion is recommended, with repair of the defect using W-plasty or Z-plasty. This article reports the case of a 38-year-old patient with congenital midline cervical cleft. A simple Z-plasty was carried out after excision of the lesion, and a satisfactory aesthetic and functional result was achieved. Congenital midline cervical cleft is a rare abnormality; however, early diagnosis and appropriate surgical treatment are necessary to avoid changes in the development of the face and limitation of neck extension.
Keywords: Branchial region/abnormalities. Neck/surgery. Reconstructive surgical procedures.
RESUMO
Existe uma deformidade cervical da linha média que tem sido descrita com vários nomes. Embora sua causa embriológica continue sendo controversa, a etiologia mais aceita até hoje é a falha da fusão na linha média dos arcos branquiais distais. A característica principal é uma lesão protuberante na linha média da região anterior do pescoço, entre o mento e a fúrcula esternal. Recomenda-se a ressecção cirúrgica completa da lesão, e a reconstrução do defeito com w-plastia ou zetaplastia. Neste artigo, é relatado o caso de uma paciente de 38 anos, com fissura congênita cervical da linha média. Após exérese da lesão, foi realizada zetaplastia simples, obtendo-se bom resultado tanto estético como funcional. As fissuras congênitas cervicais da linha média são alterações raras na população mundial, porém seu diagnóstico precoce e tratamento cirúrgico adequado são necessários para prevenir alterações no crescimento facial e restrição na extensão do pescoço.
Palavras-chave: Região branquial/anormalidades. Pescoço/cirurgia. Procedimentos cirúrgicos reconstrutivos.
Congenital midline cervical cleft (CMCC), also called median fissure of the neck, web neck, or pterygium colli medianum, is a deformity at the midline of the neck. This abnormality was first reported by Luschka in 1848; however, it was described in detail in 1946 by Ombredanne in his book on pediatric surgery1,2.
CMCC is a rare deformity, with less than 100 cases reported in the literature. Its embryologic origin is not clearly established, but most authors classify it as a developmental abnormality of the branchial arches3. CMCC is occasionally associated with other congenital malformations such as thyroglossal cyst, ectopic bronchogenic cyst, or cardiac lesions2,4; however, in the literature reviewed, there are no reports of CMCC as part of a defined syndrome.
The treatment of CMCC consists of complete resection of the lesion followed by primary closure using W-plasty or, most commonly, single or multiple Z-plasty5.
CASE REPORT
A 38-year-old female patient presented with a scar in the midline of the anterior cervical region and limited neck extension.
On clinical examination, the patient was found to have a midline cervical lesion (width, 1 cm; length, 10 cm) that had thin, reddened skin. On palpation, the lesion presented as a firm and fibrous cord. The lesion was superficial, and adherence to deep structures was not noted. It had a slightly harder consistency in the distal region, in which an orifice of approximately 2 mm in diameter was observed; no discharge was present. However, the patient mentioned various episodes of infection at the lesion site, with purulent discharge from the orifice. There was no change in the lesion during swallowing or protrusion of the tongue. In addition, the patient presented with retrognathia and limited neck extension.
A cervical ultrasound revealed an anechoic tubular structure in the subcutaneous planes of the anterior cervical region; this structure was located at the midline, was approximately 2.6 mm at its widest margin, and extended from the submentonian region to the suprasternal notch, where the fistula opening on the skin surface was observed.
During surgery, an ellipse of skin with a 1 mm margin was excised, including the full thickness of the defect. The lesion extended from the submentonian region to slightly above the suprasternal notch. Two bands of muscle tissue that were adjacent to the lesion, were unresponsive to electrical stimulation, and were not adherent to the deeper structures were also excised. A multiple Z-plasty was planned, including use of the platysma to close the defect. However, during surgery, the second Z-plasty was deemed unnecessary.
Figures 1 to 5 show the main steps of the surgical procedure.
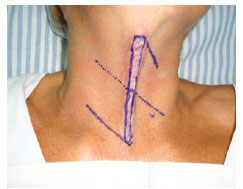
Figure 1 - Preoperative appearance. Marking of the resection line and surgical plane.

Figure 2 - Intraoperative view. Elevation of the flaps; visible muscular band adjacent to the cleft.

Figure 3 - Intraoperative view. Resected muscular band.

Figure 4 - Immediate postoperative appearance. Final suture of the defect.

Figure 5 - Immediate postoperative appearance. Side view showing improvement of the contour of the neck.
Histopathologic examination revealed a cutaneous segment that exhibited an area of ulceration with a dense mixed inflammatory infiltrate. The remaining histologic sections showed the presence of cystic glandular dermal structures that were lined by mucus-secreting and/or ciliated cylindrical epithelium without atypia (Figure 6). The dermis contained dense connective tissue, proliferating vessels, and sparse mononuclear inflammatory infiltrate. Skeletal striated muscle tissue and vascularized connective tissue that formed isolated fragments were observed in continuity with the dermis (Figure 7).
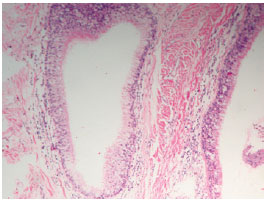
Figure 6 - Histopathologic appearance; visible cystic glandular structures lined by mucus-secreting cylindrical epithelium.
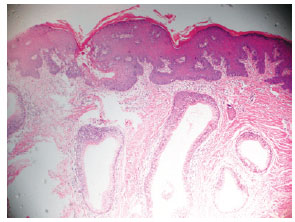
Figure 7 - Histopathologic appearance; dermis containing dense connective tissue, proliferating vessels, and sparse mononuclear inflammatory infiltrate. Skeletal striated muscle tissue and vascularized connective tissue are observed in continuity with the dermis.
The Z-plasty achieved a satisfactory aesthetic and functional result (Figure 8).

Figure 8 - Appearance of the incision on the 15th postoperative day, showing improvement of the contour of the neck.
DISCUSSION
CMCC is a rare abnormality, with less than 100 cases reported in the literature2,6. However, studies have shown that approximately 2% of congenital cervical malformations are CMCCs1,7.
The currently accepted embryologic origin of CMCC is impaired midline fusion of the distal branchial arches3,8,9. However, it has not been clearly established from which arch the malformation is derived and how cellular migration occurs. Cases of CMCC can be grouped into 2 main entities: midline cervical cleft and hypoplasia of the mandibular arch. Decreased or deficient cellular migration through the second arch (hyoid) results in isolated CMCC. More complicated presentations, with mandible or tongue cleft and absence of cervical support structures, are the result of defects in the first arch (mandibular)7.
The branchial arches are formed on the 22nd day of embryonic development. The first arch divides into a maxillary process and a mandibular process, with a horizontal cleft dividing each side at the midline. The mandibular process appears on the 26th day. A delay in this phase could result in the deposition of ectodermal and mesodermal cells on the anterior part of the neck8,9. These cells continue to differentiate to form muscles, salivary gland tissue, and mucosa, resulting in CMCC9.
CMCC is diagnosed by clinical examination, and the main characteristic is a protruding lesion at the midline of the anterior region of the neck, between the chin and the suprasternal notch. This lesion extends caudally as a longitudinal cleft lined by a reddened epithelium that is most commonly desquamative. Usually, a mucus-secreting opening of the fistulous tract can be found in the most caudal portion of the cleft. Palpation reveals a subcutaneous fibrous cord that extends to the entire cleft or part of it, from the submentonian region to the suprasternal notch2,9.
Histologically, the lesion consists of keratinized stratified squamous epithelium and fibrous tissue and is characterized by the absence of epithelial adnexa in the dermis8-10. Salivary gland tissue and pseudostratified ciliated columnar epithelium are observed in the fistulous tract and in the cyst. In the area of the nipple-like protuberance, there is normal skin, but cartilage and muscle can also be found.
Treatment of CMCC involves surgery. However, the condition is often not diagnosed early enough, either because the abnormality is misdiagnosed as another cervical lesion or because clinical findings are overlooked by the parents or even by healthcare professionals. Delay in treatment of CMCC changes the growth of the lower third of the face and particularly affects mandibular development and extension of the neck10. Z-plasty is one of the surgical procedures used to correct CMCC; it is a routine operation among reconstructive plastic surgery techniques. It allows the surgeon to lengthen a contracture scar, reorient the direction of a scar or defect, break up a straight line, and improve soft tissue contour11. Because of these characteristics, single, double, or multiple Z-plasty is the treatment of choice for CMCC11.
Z-plasty involves the rotation of 2 triangular flaps to close a central defect. The classic Z-plasty is symmetrically designed so that the lateral limbs of the Z are equal to the defect that needs reconstruction (central limb), and the angles between the lateral limbs and the central limb are 60º11. The optimal angle is 60º, as it allows a theoretical gain in length of 75%11.
CMCC is a rare abnormality; however, early diagnosis and appropriate surgical treatment are necessary to avoid changes in facial development and limitation of neck extension. Individual treatment depends on the severity of the case, and satisfactory functional and aesthetic outcomes are required to meet the patient's aesthetic expectations.
REFERENCES
1. Derbez R, Nicollas R, Roman S, Estève A, Triglia JM. Congenital midline cervical cleft of the neck: a series of five cases. Int J Pediatr Otorhinolaryngol. 2004;68(9):1215-9.
2. Ayache D, Ducroz V, Roger G, Garabédian EN. Midline cervical cleft. Int J Pediatr Otorhinolaryngol. 1997;40(2-3):189-93.
3. Kawar B, Siplovich L. Congenital midline cervical skin bridge: a case report. J Pediatr Surg. 2008;43(3):544-5.
4. Hirokawa S, Uotani H, Okami H, Tsukada K, Futatani T, Hashimoto I. A case of congenital midline cervical cleft with congenital heart disease. J Pediatr Surg. 2003;38(7):1099-101.
5. Cheng SS, Gottschall JA. Double opposing Z-plasty for congenital midline cervical web: a case report. Int J Pediatr Otorhinolaryngol Extra. 2009;4(3):123-8.
6. Genc A, Taneh C, Arslan O, Daglar Z, Mir E. Congenital midline cervical cleft: a rare embryopathogenic disorder. Eur J Plast Surg. 2002;25(1):29-31.
7. Niranjan NS. Webbing of the neck: correction by tissue expansion. Plast Reconstr Surg. 1989;84(6):985-8.
8. Erçöçen AR, Yilmaz S, Aker H. Congenital midline cervical cleft: case report and review. J Oral Maxillofac Surg. 2002;60(5):580-5.
9. Gardner RO, Moss AL. The congenital cervical midline cleft. Case report and review of literature. Br J Plast Surg. 2005;58(3):399-403.
10. Sharma U, Mehta MM, Bhatia VY. Congenital midline cervical cleft presenting as neck contracture. Eur J Plast Surg. 2009;32(5):263-6.
11. Hirokawa S, Uotani H, Okami H, Tsukada K, Futatani T, Hashimoto I. A case of congenital midline cervical cleft with congenital heart disease. J Pediatr Surg. 2003;38(7):1099-101.
1. Plastic surgeon at the Hospital Universitário Antonio Pedro da Universidade Federal Fluminense (UFF), Niterói, RJ, Brazil. Plastic surgeon at Clínica La Esperanza, Clínica Rey David and Clínica Farallones, Cali, Colombia.
2. Specialist in plastic surgery, full member of the Sociedade Brasileira de Cirurgia Plástica/Brazilian Society of Plastic Surgery (SBCP), director of the Plastic Surgery Department at the Hospital Universitário Antonio Pedro da UFF, Niterói, RJ, Brazil.
3. Specialist member of SBCP, plastic surgeon at the Hospital Universitário Antonio Pedro da UFF, Niterói, RJ, Brasil.
4. Medical intern at the Hospital Universitário Antonio Pedro da UFF, Niterói, RJ, Brasil.
Correspondence to:
Álvaro Hernan Rodriguez Rodriguez
Carreira 41, número 5B-28
Cali, Colombia
E-mail: dralvarohrodriguez@hotmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: December 9, 2011
Article accepted: July 1, 2012
This study was performed at the Hospital Universitário Antonio Pedro da Universidade Federal Fluminense, Niterói, RJ, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter