

Original Article - Year 2013 - Volume 28 -
Analysis of structured fat grafting for redefining facial contours
Análise da lipoenxertia estruturada na redefinição do contorno facial
ABSTRACT
INTRODUCTION: Fat grafting as a filling method for the rejuvenation and enhancement of facial contours was demonstrated by some authors to be an excellent alternative method for redefining facial contours, based on the premise that the donor tissue used in the correction of the deformities has similar characteristics as the recipient tissue. The objective of the present study was to clinically evaluate the efficiency of structured fat grafting when redefining facial contours.
METHODS: A retrospective evaluation was performed in 39 patients who underwent structured fat grafting to redefine their facial contours between 2002 and 2012. The patients selected included those who underwent corrections of deformities, asymmetrical features, contour smoothing, and increased bone projection. Patients who underwent facial contour rejuvenation were excluded. The clinical outcome assessment was performed by the patient and surgeon, with the aid of preoperative and postoperative photographic documentation. The clinical outcome was rated by the patient and surgeon, using a scale ranging from 1 to 3, defined as follows: 1, the objective has not been achieved in any way; 2, the objective was partially achieved; or 3, the objective was fully achieved. In addition, a survey was conducted using the patients' medical charts to obtain the following data: age, weight change, volume grafted by area, number of grafting sessions performed, history of smoking, and complications.
RESULTS: The mean surgeon and patient assessment scores were 2.6 ± 0.6 and 2.7 ± 0.5, respectively, with a statistically significant correlation (P < 0.0001). No significant relationship was found between the assessments and age, weight change, graft volume, or smoking habit, with the exception of the cheekbone area.
CONCLUSIONS: Structured fat grafting proved to be an efficient adjuvant technique for redefining facial contours, and its efficiency was not affected by age, weight change, or smoking habit. However, the fat volume to be grafted should be adequate for the specific needs of each area.
Keywords: Adipose tissue/surgery. Transplantation. Lipectomy. Injections subcutaneous.
RESUMO
INTRODUÇÃO: A enxertia de gordura como preenchimento no rejuvenescimento e melhoria do contorno facial vem sendo usada por alguns autores e demonstra um potencial excelente como método de escolha para essa finalidade, uma vez que tem como premissa o princípio básico de corrigir as deformidades com o tecido mais semelhante possível. O objetivo deste trabalho foi avaliar clinicamente a eficiência da enxertia de gordura estruturada na redefinição do contorno facial.
MÉTODO: Foi realizada análise retrospectiva de 39 pacientes submetidos a lipoenxertia estruturada para a redefinição do contorno facial, entre 2002 e 2012. A seleção de pacientes incluiu correção de deformidades, assimetrias, harmonização do contorno e aumento da projeção óssea, mas excluiu o rejuvenescimento per se. A avaliação do resultado clínico foi realizada pelo paciente e pelo cirurgião, com auxílio de documentação fotográfica pré e pós-operatória. O resultado clínico foi classificado pelo paciente e cirurgião, empregando escala que variava de 1 a 3: (1) o objetivo não foi alcançado de forma alguma; (2) o objetivo foi alcançado parcialmente; ou (3) o objetivo foi alcançado totalmente. Foi realizado, também, levantamento de prontuários para obtenção dos seguintes dados: idade, alteração ponderal, volume enxertado por área, número de sessões de enxertia realizadas, história de tabagismo e complicações.
RESULTADOS: As médias das avaliações do cirurgião e paciente foram, respectivamente, 2,6 ± 0,6 e 2,7 ± 0,5, havendo correlação estatisticamente significante (P < 0,0001). Não foi encontrada relação significativa entre as avaliações e idade, alteração ponderal, volume de enxertia ou tabagismo, com uma única exceção.
CONCLUSÕES: A lipoenxertia estruturada demonstrou ser eficiente adjuvante na redefinição do contorno facial e sua eficiência não foi prejudicada por idade, alteração ponderal ou tabagismo. O volume a ser enxertado deve ser adequado às necessidades específicas de cada área.
Palavras-chave: Tecido adiposo/cirurgia. Transplante. Lipectomia. Injeções subcutâneas.
Augmentation by fat grafting has become very popular in the last years, after decades of being overlooked, and this become possible due to new knowledge and techniques that made results more predictable and long-lasting1. Additionally, new interest arouse from the discovery of the presence of large amounts of stem cells in the lipoaspirate, which increased it's use and research on the subject2. Different methods of harvesting and reinjection of the fat, which damaged this delicate tissue, yielded conflicting results, even in the hands of experienced surgeons and that rendered the procedure's reputation unreliable3-7.
The use of fat grafting as a filler for facial rejuvenation and contour enhancement has been reported as successful by several authors and appears to be promising as the method of choice for such purpose, once it has attributes of the ideal filler, replacing like with like8,9.
Structural fat grafting, or lipostructure, term coined by Coleman, is one of those methods and possibly the most popularized one, because of it's didactic presentation and widespread reporting8. Nevertheless, others have shown good results as well with their methods9-11. Essentially this method focuses on obtaining fat with low negative pressure, separating the viable tissue from other matter through centrifugation under low acceleration and injecting small globules of fat at a time in order to allow for adequate graft take.
Many of the patients who seek facial contour enhancement do not accept or wish for skeletal surgery, since it is perceived as traumatic and associated with significant morbidity. Furthermore, some patients who underwent skeletal surgery need refinement of their result and it appears only logical that a simpler procedure be sought.
The authors experience with structural fat grafting in body and facial contour enhancement rendered such promising results that a decision was made to give continuity on a previous work on the matter12,13. The goal of this study was to clinically evaluate the efficiency of structural fat grafting for the enhancement of facial contour in a larger number of patients, followed for a longer period of time and in a more analytic fashion, so as to better characterize the procedure and allow for more objective comparison between different surgeons and techniques. In this study structural fat grafting applications included augmentation of bony projection, correction of deformities and asymmetries, excluding rejuvenation per se. Additionally, albeit the small number of patients that underwent this application, intraorbital fat grafting was performed to treat posttraumatic enophthalmos, which has rarely been reported in the literature14,15. Furthermore, alterations in the neighboring tissues were noted, since there has been an increasing number of reports to the benefits of fat grafting in surrounding tissues16,17.
METHODS
From 54 patients operated on from 2002 to 2012, 39 were chosen for this study for having pre and postoperative photographic documentation that allowed for evaluation of results. The group included patients of both sexes, between 23 and 71 years of age (mean of 44.6 years and median of 44 years), followed for 1.5 to 114 months (mean of 31.5 months and median of 23 months).
Patients included had facial deformities, asymmetries, needed more bony projection or enhancement of their facial contour, whether they had gone through skeletal surgery or not previously. Patients seeking rejuvenation exclusively were excluded from the study.
Data obtained from their charts included number of grafting sessions and volumes for each patient and area, complications, smoking habits and body weight changes between surgery and final evaluation.
Weight change was arbitrarily set as being 5% or more from baseline and patients were ranked 0 for no change, 1 for gain and -1 for loss. Complications were noted and classified as being present (1) or absent (0).
The method of structural fat grafting used was that of Coleman8.
Areas evaluated were periorbital, intraorbital frontal, nasal, malar, maxillary, mandibular and mental, different patients had different areas grafted. Intraorbital grafting was performed posterior to the orbital septum, in 2 patients to correct posttraumatic enophthalmos.
Results were ranked in a scale of 1 to 3, in reference to the level of satisfaction, or achievement of the proposed goal, by the patient and the surgeon, thus 1 for not satisfied at all, 2 for partially and 3 for totally satisfied. Both surgeon and patient made their evaluation. Pre and postoperative photos were used for this purpose, in front, side and 3/4 side views.
Data obtained form the evaluation of the surgeon was correlated to that of the patient by nonparametric Kendall's test (Analyse-it®). Regression analyses were carried out to see if there was relation of dependence between the surgeons evaluation and other factors such as weight change, patient age, volume injected or smoking, both simple and polinomial regression (Analyse-it®).
RESULTS
The number of grafting sessions in each patient varied from 1 to 6 with a mean of 1.4 and a median of 1. Complications occurred in 3 patients, two of which were submitted to the greatest number of sessions, respectively 4 and 6: In the first patient there was excessive grafting in the malar area that had to be aspirated in the second session and a dehiscence of a canthopexy performed simultaneously. In the second patient, there was excessive grafting to the periorbital area, that had to be surgically removed and a more apparent excess in the frontal area after the patient gained nearly 17% of her body weight, that resolved spontaneously after she returned to her normal weight. Finally, in the third patient there was a third degree burn in her buttocks from a faulty electrocautery. Complications occurred in 7.69% (3/39) of patients.
The mean result evaluation for the surgeon was 2.6 (median 3 ± 0.6 SD) and for the patient 2.7 (median 3 ± 0.5 SD). The surgeons and patients evaluation correlated positively and significantly (P < 0.0001).
Simple regression analyses showed no relation of dependence between volume injected, weight change, smoking, or patient age and the surgeons evaluation, with a single exception: an inverse relation between age and the surgeon's evaluation of the malar area (P = 0.0053).
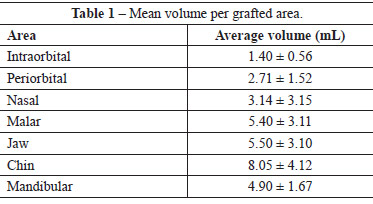
Table 1 presents the mean volumes injected per area with standard deviations.
The following cases illustrate the results achieved with lipostructure.
Case 1 - The patient needed more projection of her nose tip and chin, fat graft was performed injecting the alar bases, 2 ml to the right and 1.5 ml to the left and 15 ml to the chin, in a single session. Figure 1 shows the preoperative aspects at 5 years.
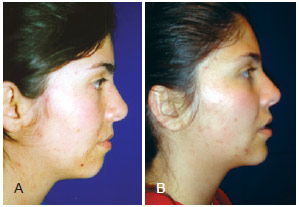
Figure 1 - Case 1. In A, preoperative appearance. In B, appearance 5 years after completion of the structured fat grafting in the alar bases and chin.
Case 2 - The patient had a clear indication for skeletal surgery, but would not accept it after many years of unplanned orthodontic treatment. A rhinoplasty was performed along fat grafting of her alar bases and malar areas, mounting to 5.5 ml to the right an 6 ml to the left, in a single session. Figure 2 depicts the preoperative and postoperative appearances at 1 year. In the following 5 years, the patient had lost 6 kg of weight, which was slightly more than 10% of the total body weight. Although the patient was emaciated, much of the projection obtained had remained (Figure 3).

Figure 2 - Case 2. In A and B, preoperative aspect. In C, appearance 1 year after rhinoplasty and structured fat grafting in the cheekbones and alar bases.
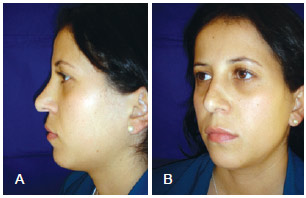
Figure 3 - Case 2. In A and B, appearance 5 years after rhinoplasty and structured fat grafting in the cheekbones and alar bases.
Case 3 - This patient fractured of her zygoma, maxilla and orbit and had a resultant enophthalmos, distopia and malar depression (Figure 4). Four grafting sessions were performed, injecting 3.9 ml in the left periorbit, 7 ml in the left malar area and 1 ml in the intraorbital area. Figures 4A and 4B show her postop of over 5 years, and even though the preoperative worm's view is not available, it is possible to see the improvement on the dystopia, scleral show and position of the superior eyelid crease.
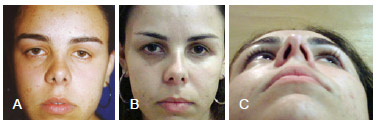
Figure 4 - Case 3. In A, preoperative appearance. In B and C, appearance at slightly more than 5 years after completion of the structured fat grafting in the periorbital region, left cheekbone, and left intraorbital region and the patient lost around 10% of her body weight.
Case 4 - This patient had discoid lupus and underwent 2 sessions of fat grafting, having injected 6 ml in the nose and 4 ml in the chin in the first session and 5 ml in the nose and 4 ml in the chin in the second one. A partial resection of the keratotic kin over the dorsum of the nose was performed in another surgery after the grafting. Figure 5 shows the preoperative and postoperative appearances after slightly more than 5 years.
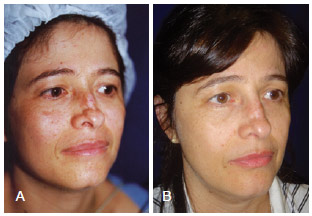
Figure 5 - Case 4. In A, preoperative appearance. In B, appearance at slightly more than 5 years after performing the structured fat grafting in the nose and chin, complemented with partial resection of the keratotic zone of the nasal dorsum.
Case 5 - This patient has Romberg syndrome and was initially treated with Medpore® in her forehead and traditional fat grafting, with poor results. Figure 6A shows the preoperative appearance, Figure 6B shows the postoperative appearance at almost 4 years after the first structured fat grafting session, and Figure 6C shows the appearance 6 months after the second session. In the first session, 3.5 mL of fat was injected into the forehead, 1 mL into the upper eyelid, and 15 mL into the cheek. In the second session, 9 mL of fat was injected into the left forehead, 2.7 mL of fat into the upper eyelid, 6.5 mL of fat into the left cheekbone, and 3.5 mL into the scalp.
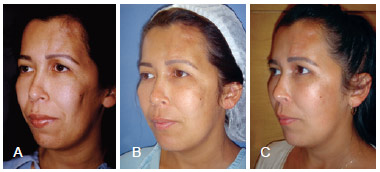
Figure 6 - Case 5. In A, preoperative appearance. In B, postoperative appearance almost 4 years after the first session of the structured fat grafting in the forehead, upper eyelid, and cheek. In C, appearance 6 months after the second session of structured fat grafting in the forehead, left upper eyelid, left cheek, and scalp.
Case 6 - This patient demonstrates one of the possible complications, that is, overgrafting, which can easily happen in the periorbital area and needed to be surgically removed (Figure 7).

Figure 7 - Case 6. Patient presenting with excess grafting, especially in the periorbital region, which was visible and had to be surgically removed.
Both cases of chronic diseases, lupus and Romberg presented a clinically visible improvement of the surrounding tissues. The patient with lupus reported that she her glasses no longer hurt the area where they leaned on her nose. Pathological analysis revealed degenerative changes of the fragment removed from the dorsum of her nose.
DISCUSSION
As strong points this study has patients operated by the same surgeon with the same technique, followed over a long period of time, with a detailed evaluation per area, which facilitates more objective comparison between different surgeons and methods.
On the other hand, as with all retrospective studies, it is limited by the analysis of the available data only and shows a qualitative evaluation, which always carries some subjectivity. A quantitative analysis through 3 dimensional photography or magnetic resonance imaging is the next step to bring in hard data for a more objective point of view.
There was a low incidence of complication that, if on one hand eventually demanded surgical correction, on the other hand had a simple and total resolution.
The significant correlation between the surgeon's and the patient's evaluation helped validate the method, even though it is still subjective. The evaluation was always done through the photographs for two reasons: some results could only be fully analyzed with a side view, which is hard for the patient to do and rarely does the patient remember his preoperative appearance. Furthermore, structural fat grafting rarely if ever produces nodules or long term inflammatory reaction, which sometimes makes the patient think that the fat got reabsorbed1,18,19.
Very significant weight changes, specially gain, may cause contour deformation, but returning to previous weight corrects the problem. This aspect should always be discussed with the patient prior to surgery.
Regression analysis indicated an inverse relation between the surgeons evaluation of the malar area and patient age, that is, the younger the patient the better the evaluation. Although this makes sense, since younger patients will have firmer tissue that will tend to retain better the new projection obtained, analysis of the dispersion plot of the variables showed some outliers that could potentially change this relation. Additionally, the quality of adjustment of the model, translated by the coefficient of determination (r2) was not as high as ideally should be. A larger sample in future studies may resolve that point by confirming this tendency to extend on to other areas, or disappearing.
All techniques have a learning curve and in this case it may be steep. It is important to say that overcorrection is not recommended with this method, since it is expected that most of the graft takes, especially in the periorbital area, where skin and subcutaneous tissue are very thin and any excess will turnout visible.
The mean volumes injected in each area presented here may help the surgeon who may be initiating in this technique to find the right volume for the desired correction, but one should probably inject less rather than more, when first using this method, for the fat will be layered into the tissues and it may be very hard to remove if excessive amounts are placed8.
Although there is still some controversy regarding the efficacy of structural fat grafting, there is no doubt that it's application has gained popularity and that will bring the opportunity of establishing it's true value in plastic and reconstructive surgery20,21.
Little is known about intraorbital fat grafting and it's outcome and only two references were found14,15. The first one, a clinical paper on patients who underwent this type of grafting after enucleation in which there was need to remove excessive fat after overcorrection. The second one was an experimental work, on an animal model, on interposition of buccal fat in the orbital cone for the treatment of posttraumatic diplopia. In this series, albeit the small number of cases, there was significant improvement of the enophthalmos, without concurrent complications related to the procedure. It is essential though to be cautious when performing intraorbital injections to avoid undue trauma, which could lead to bleeding and retrobulbar hematoma with possible compression of the optic nerve.
The reason for the beneficial effects of the graft on surrounding tissues is not clear. Some of the studies point to the effect of the adipo se derived stem cells itself or their ability to release cytokines and hormones that may act on angiogenesis, or enhancing the immune response22-24.
CONCLUSIONS
Structural fat grafting was, in this series, an efficient adjunct to facial contour enhancement, shown by satisfactory long term results, both from the point of view of the surgeon as well as the patient's. Complications were minimal and, in many cases, a single session of grafting was enough to achieve the desired result.
REFERENCES
1. Coleman SR. Structural fat grafting: more than a permanent filler. Plast Reconstr Surg. 2006;118(3 Suppl):108S-20S.
2. Aust L, Devlin B, Foster SJ, Halvorsen YD, Hicok K, du Laney T, et al. Yield of human adipose-derived adult stem cells from liposuction aspirates. Cytotherapy. 2004;6(1):7-14.
3. Illouz YG. The fat cell "graft": a new technique to fill depressions. Plast Reconstr Surg. 1986;78(1):122-3.
4. Teimourian B. Repair of soft-tissue contour deficit by means of semi-liquid fat graft. Plast Reconstr Surg. 1986;78(1):123-4.
5. Illouz YG. Fat injection: a four-year clinical trial. In: Hetter GP, ed. Lipoplasty: the theory and practice of blunt suction lipectomy. Boston: Little Brown; 1990. p.239-46.
6. Carpaneda CA, Ribeiro MT. Study of histologic alterations and viability of the adipose graft in humans. Aesthetic Plast Surg. 1993;17(1):43-7.
7. Marques A, Brenda E, Saldiva PHN, Amarante MTJ, Ferreira MCF. Enxerto de gordura em coelhos. Rev Bras Cir Plást. 1998;13(1):37-50.
8. Coleman SR. Facial recontouring with lipostructure. Clin Plast Surg. 1997;24(2):347-67.
9. Bersou Júnior A. Lipoenxertia: técnica expansiva. Rev Bras Cir Plást. 2008;23(2):89-97.
10. Ersek RA, Chang P, Salisbury MA. Lipo layering of autologous fat: an improved technique with promising results. Plast Reconstr Surg. 1998;101(3):820-6.
11. Ellenbogen R. Fat transfer: current use in practice. Clin Plast Surg. 2000;27(4):545-56.
12. Amarante MTJ. Lipoestrutura: rejuvenescimento e redefinição do contorno facial e corporal. In: XLII Congresso Brasileiro de Cirurgia Plástica; 2005; Belo Horizonte, Brasil.
13. Amarante MTJ. Lipostructure: an efficient adjunct to facial contour. In: Wolfe SA, ed. Craniofacial surgery. Bologna: Manduzzi Editore; 2008.
14. Anderson OA, Tumuluri K, Francis ND, Olver JM. Periocular autologous Coleman fat graft survival and histopathology. Ophthal Plast Reconstr Surg. 2008;24(3):213-7.
15. Yu JC, Brooks SE, Preston D, Johnson MH. Treatment of posttraumatic ocular dysmotility using autogenous buccal fat grafts in a porcine model. Plast Reconstr Surg. 1999;104(3):719-25.
16. García-Olmo D, García-Arranz M, García LG, Cuellar ES, Blanco IF, Prianes LA, et al. Autologous stem cell transplantation for treatment of rectovaginal fistula in perianal Crohn's disease: a new cell-based therapy. Int J Colorectal Dis. 2003;18(5):451-4.
17. Cantarella G, Mazzola RF, Domenichini E, Arnone F, Maraschi B. Vocal fold augmentation by autologous fat injection with lipostructure procedure. Otolaryngol Head Neck Surg. 2005;132(2):239-43.
18. Broder KW, Cohen SR. An overview of permanent and semipermanent fillers. Plast Reconstr Surg. 2006;118(3 Suppl):7S-14S.
19. Vargas AF, Amorim NG, Pitanguy I. Complicações tardias dos preenchimentos permanentes. Rev Bras Cir Plást. 2009;24(1):71-81.
20. Obagi S. Autologous fat augmentation: a perfect fit in new and emerging technologies. Facial Plast Surg Clin North Am. 2007;15(2):221-8.
21. Seth R, Nabili V, Fritz MA, Alam DS, Knott PD. Volume-directed facial soft tissue deficit reconstruction. Facial Plast Surg. 2010;26(6)494-503.
22. Nakagami H, Maeda K, Morishita R, Iguchi S, Nishikawa T, Takami Y, et al. Novel autologous cell therapy in ischemic limb disease through growth factor secretion by cultured adipose tissue-derived stromal cells. Arterioscler Thomb Vasc Biol. 2005;25(12):2542-7.
23. Charriere G, Cousin B, Arnaud E, André M, Bacou F, Penicaud L, et al. Preadipocyte conversion to macrophage. Evidence of plasticity. J Biol Chem. 2003;278(11):9850-5.
24. Cousin B, André M, Casteilla L, Pénicaud L. Altered macrophage-like functions of preadipocytes in inflammation and genetic obesity. J Cell Physiol. 2001;186(3):380-6.
Plastic surgeon, full member of the Sociedade Brasileira de Cirurgia Plástica/Brazilian Society of Plastic Surgery, master's degree in medicine from the School of Medicine, University of São Paulo, Poços de Caldas, MG, Brazil
Correspondence to
Marco Tulio Junqueira Amarante
Av. Santo Antonio, 200 - cj. 302 - Cascatinha
Pocos de Caldas, MG, Brazil - CEP 37701-036
E-mail: marcotulioja@marcotulioja.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: November 19, 2012
Article accepted: February 2, 2013
This study was performed at the private clinic of the author, Poços de Caldas, MG, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter