

Original Article - Year 2013 - Volume 28 -
Complications in total breast reconstruction in patients treated for breast cancer: long-term comparative analysis of the influence of the technique, operative time, timing of reconstruction, and adjuvant treatment
Complicações em reconstrução mamária total em pacientes mastectomizadas por câncer de mama: análise comparativa de longo prazo quanto a influência de técnica, tempo de cirurgia, momento da reconstrução e tratamento adjuvante
ABSTRACT
INTRODUCTION: Some techniques for total reconstruction of the breast, regardless of complexity, present specific complications, with varying degrees of morbidity. Therefore, the aim of this study was to identify the most frequent complications of the main techniques used for breast reconstruction, and to compare these complications to the relevant independent variables.
METHODS: This cross-sectional observational study was conducted by reviewing the medical records of patients who had their breasts completely rebuilt after a mastectomy due to breast cancer from January 2007 to December 2009, with a minimum postoperative follow-up of 3 years. The data collected, such as the timing of the intervention, reconstruction techniques, operative time, and adjuvant treatment, were statistically related to the presence of complications.
RESULTS: Of the 48 total breast reconstructions analyzed, the technique in which expanders were used followed by replacement with implants showed the lowest prevalence of complications (16.7%, P < 0.000). Some techniques showed specific complications. The operative time for transplantation of transverse rectus abdominis musculocutaneous flap (363.57 ± 59.91 min) was significantly higher than that required for techniques using alloplastic materials (155.71 ± 38.02 min, P = 0.01), but similar to that for the latissimus dorsi flap (309.69 ± 77.66 min). The operative time, timing of surgical intervention, and type of adjuvant treatment did not correlate with the incidence of complications.
CONCLUSIONS: Each technique has its indications, contraindications, and complications. The application of each technique should be individualized on the basis of the individual characteristics of the patient to obtain better results, avoiding short- and long-term complications.
Keywords: Breast/surgery. Breast implantation. Mammaplasty/complications. Postoperative complications.
RESUMO
INTRODUÇÃO: Algumas técnicas de reconstrução total de mama, independentemente de sua complexidade, apresentam complicações específicas, com diferentes graus de morbidade. Com base nessas informações, o objetivo deste estudo foi identificar as complicações mais frequentes apresentadas pelas principais técnicas de reconstrução mamária e compará-las a relevantes variáveis independentes.
MÉTODO: Estudo observacional tipo coorte transversal, realizado por meio de revisão de prontuários médicos de pacientes que tiveram suas mamas totalmente reconstruídas após mastectomia por câncer de mama, no período de janeiro de 2007 a dezembro de 2009, com tempo mínimo de seguimento pós-operatório de 3 anos. Os dados coletados, como momento da intervenção, técnicas de reconstrução, tempo de cirurgia e tratamento adjuvante, foram estatisticamente relacionados à presença de complicações.
RESULTADOS: Das 48 reconstruções mamárias totais analisadas, a técnica com expansor seguido pela troca por implante mamário foi a que apresentou menor prevalência de complicação em relação às outras técnicas (16,7%; P < 0,000). Algumas técnicas apresentaram complicações específicas. O tempo cirúrgico do retalho transverso do músculo reto abdominal (TRAM; 363,57 ± 59,91 minutos) foi significativamente maior que das técnicas com materiais aloplásticos (155,71 ± 38,02 minutos; P = 0,01), mas semelhante ao do grande dorsal (309,69 ± 77,66 minutos). O tempo de cirurgia, o momento da intervenção cirúrgica e o tipo de tratamento adjuvante não apresentaram relação com a incidência de complicações.
CONCLUSÕES: Cada técnica empregada tem sua indicação, contraindicação e complicação e a aplicação de cada técnica deve ser individualizada, baseando-se em características individuais da paciente, a fim de se obter um melhor resultado, evitando complicações a curto e longo prazos.
Palavras-chave: Mama/cirurgia. Implante mamário. Mamoplastia/complicações. Complicações pós-operatórias.
The major advances in breast oncology in recent decades have provided a better understanding of the pathophysiology of breast cancer. This has enabled early detection of this disease, with a consequential increase in the number of cases treated, as well as development of more conservative surgeries that enable immediate breast reconstruction using various techniques.
The advent of adenomastectomy, which is the total removal of 1 or both breasts with preservation of the skin and, when possible, even the nipple areolar complex, has resulted in an increasing number of indications for prophylactic breast resection. Consequently, total breast reconstruction has become an increasingly common procedure1-3.
Many breast reconstruction techniques have been developed over the years, and their indications are often based on factors related to the sequelae of mastectomy, physical characteristics of the patients, prognosis of breast cancer, qualifications of the medical staff, and available institutional resources. Despite the specific indications dependent on the above conditions, in many cases, various techniques for total breast reconstruction can be performed immediately or at a later time. Among the procedures most commonly used in the field are implantation of myocutaneous pedicled flaps, such as latissimus dorsi muscle (LD) and transverse rectus abdominis musculocutaneous (TRAM) flaps, and the use of alloplastic materials (AM), such as temporary or permanent tissue expanders and silicone implants.
At the beginning of the last century, the treatment of breast cancer resulted in mutilation, with broad surgeries that removed the entire breast, including a large area of skin and even muscles. Furthermore, the treatment involved a combination of radiotherapy, which results in considerable aesthetic and functional sequelae. With a better understanding of the biology of breast tumors, the treatment began to be less radical, and concern about the psychological aspect and quality of life of patients grew4,5. Skin-sparing mastectomy emerged as a procedure that results in an improved quality of the reconstructed breast, allowing the use of techniques that may not be less complex but are less debilitating than reconstruction with AM implants4,6-10. The preservation of the skin envelope of the breast provides a satisfactory color tone, texture, and contour to the reconstructed breast, either with tissue expanders, alloplastic implants, fat grafts, or de-epithelialized flaps3,4.
Some techniques for breast reconstruction, regardless of complexity, present specific complications, with varying degrees of morbidity. Therefore, the aim of this study was to identify the most frequent complications of the main techniques used for breast reconstruction and compare these complications to the relevant independent variables. In this manner, this long-term study (minimum follow-up of 3 years) sought to address the scarcity of information on complications related to total breast reconstruction and the respective clinical courses in a period exceeding 1 year.
METHODS
Patients
This cross-sectional observational study was performed through review of medical records of patients by the main author.
The inclusion criteria were female sex and complete breast reconstruction after a mastectomy due to breast cancer from January 2007 to December 2009 at the Santa Cruz Plastic Surgery Institute, with a minimum postoperative follow-up period of 3 years (time defined by the median time of the studies focusing on capsular contracture Baker III/IV).
Parameters Analyzed
We analyzed and correlated data such as patient age, timing of the reconstruction (immediate or delayed), laterality of the reconstructed breast, operative time (in minutes), length of hospital stay (in days), technique used for the reconstruction, adjuvant treatment for breast cancer, complications, and readmission.
Statistical Analysis
The Kolmogorov-Smirnov test was performed beforehand to assess the normal distribution of the data analyzed for ordinal variables. After confirmation, the mean and standard deviation were calculated, and these variables were correlated with the complication and readmission variables by comparison of the means using Student's t test. The alpha error was set at 5% (P < 0.05%), and a confidence interval of 95% (95% CI) was used.
For nominal variables, the prevalence was analyzed. The correlation of these variables with the complication and readmission parameters was performed by cross-tabulation of up to 2 independent variables, and significance was calculated using the chi-square or Fisher test (when n < 5), with the level of significance set at 5% (P < 5%). All statistical analyses were performed using SAS software version 9.2 (SAS Institute Inc., Cary, NC, USA).
Results
The average age of the women was 48 years and 9 months, with a standard deviation of ±10.59, ranging from 26 to 71 years. Forty-eight breast reconstruction procedures were performed by residents of the care unit, under the supervision and assistance of tutors, to correct the sequelae of total mastectomy for the treatment of breast cancer. Twenty-five procedures were performed in the right breast and 23 in the left breast. Approximately 69% were immediate reconstructions and 31% were delayed reconstructions. The techniques involving the use of AM alone were the most frequent and accounted for 43.8% of the reconstructions (9 surgeries with a permanent expander, 6 with an expander followed by implant exchange, and 6 with implant alone). LD reconstructions accounted for 37.4% and TRAM for 18.8% of all reconstructions (Figure 1).
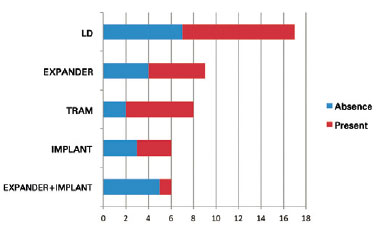
Figure 1 - Frequency of techniques used for total breast reconstruction in the sample analyzed and overall prevalence of their complications. LD = latissimus dorsi muscle; TRAM = transverse rectus abdominis flap.
The average patient age was similar in the 3 groups, being 49.81 ± 11.04, 49 ± 12.37, and 46 ± 2.27 years for reconstruction with AM only, LD, and TRAM, respectively (Table 1). The operative time for the procedure with TRAM (363.57 ± 59.91 min) was significantly higher than that for the procedures with AM (155.71 ± 38.02 min) (P = 0.01, 95% CI -266.65 to -119 of, 06), but similar to that for procedures with LD (309.69 ± 77.66 min); no statistically significant difference was found between AM and LD (P = 0.07). The duration of surgery did not correlate with the incidence of complications. In patients who received TRAM flaps, the length of hospital stay (3.43 ± 2.27 days) was significantly higher than that for patients who received LD (1.69 ± 0.48 days) (P = 0.004; 95% CI, -2.85 to -0.87) and AM (1.05 ± 0.22 days) (P = 0.000; 95% CI, -2.74 to -1.83). There was no statistically significant difference for the length of stay between LD and AM.
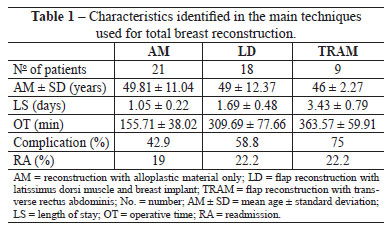
The presence of any local complication, regardless of severity, was detected in 22 cases. Seroma accounted for 10% of the complications identified and was most prevalent in the donor site of the LD, representing 16.7% of the complications identified with this technique (Figure 2). The second most frequent complications were capsular contracture, superficial infection, and deep infection (Figure 3), which individually accounted for 6.3% of the complications. In the present study, capsular contracture was identified exclusively in techniques with LD, representing, similar to seroma, 16.7% of complications with this technique. In turn, superficial infection was not associated with any specific technique and had a homogeneous distribution, whereas deep infection was identified only in reconstructions with permanent expanders (22.2% of complications in this technique) and single-step breast implants (16.7% of complications in this technique). Other noteworthy complications included the presence of abdominal bulging (Figure 4) and infection of the abdominal lining as TRAM-specific complications, which represented 22.2% and 11.1% of the total complications, respectively.
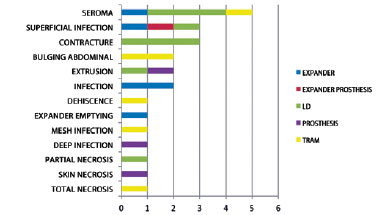
Figure 2 - Distribution of clinical complications according to the technique used for total breast reconstruction; LD = latissimus dorsi muscle; TRAM = transverse rectus abdominis flap.

Figure 3 - Infection on the topography of a breast reconstructed using a permanent expander. The patient developed worsening of symptoms, requiring the removal of the expander.

Figure 4 - Patient who underwent delayed total breast reconstruction with a rectus abdominis muscle flap (TRAM), presenting significant bulging of the abdominal wall 6 months after the reconstruction.
Among the identified complications, those that demonstrated the greatest severity, with 100% of patients requiring readmission for treatment, were extrusion (Figure 5) and deep infection (Figure 6). One patient who underwent reconstruction with TRAM had infection of the abdominal lining that progressed to sepsis. This patient remained hospitalized for 2 months for treatment and had a good recovery. The patient did not require replacement of the lining and showed no sequelae.

Figure 5 - Immediate bilateral breast reconstruction with implants. In an attempt to preserve tissue, the oncologist performed bilateral adenomastectomy with thin skin faps, and the patient developed skin necrosis, dehiscence, and implant extrusion (hole in base of the right breast, black arrow).
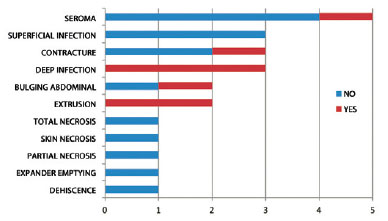
Figure 6 - The need for readmission according to the technique of total breast reconstruction used.
There were no deaths in this series of patients. The technique of breast reconstruction in 2 procedures with an expander and an implant showed the lowest incidence of complications (16.7%), represented by superficial infection and the absence of need for readmission (Table 1). The technique with the highest prevalence of infection was the use of TRAM (75%), representing 22.2% of the readmission cases. However, the surgery that had the highest incidence of readmission (33.3%) was reconstruction with an implant in a single procedure. There was a difference in the need for readmission between the technique using expanders and breast implants in 2 procedures and the other techniques (chi-square test, P < 0.001).
Regardless of the technique used, the incidence of complications was lower in patients who underwent delayed reconstruction without radiation therapy (33.3%) and higher in those who underwent delayed reconstructions combined with radiation therapy (62.5%); however, there was no significant difference (Figure 7).
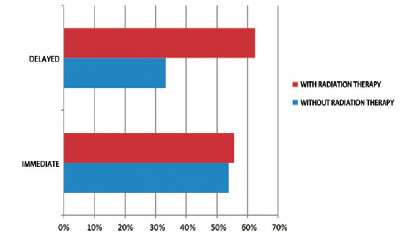
Figure 7 - Correlation of complications to the timing of total breast reconstruction and the presence of adjuvant treatment.
DISCUSSION
Breast reconstruction is assuming an increasingly important role in the treatment of breast cancer, because of the proven physical and psychological benefits for patients. This procedure favors a more rapid return of patients to their daily lifestyle, with enhanced immunity and better prognosis4,5.
In our study, the percentage of use of expanders, with or without flaps of LD or rectus abdominis, was 31.25%, which corresponds to the results reported in most health-care services for breast reconstruction, in which the incidence ranges from 30% to 43%11-15. The TRAM was used for approximately one-fourth of the reconstructions, especially in cases of delayed reconstructions and in patients with radiodermatitis.
The overall incidence of any complication (approximately 50%) in this study was consistent with that of previous studies (range, 4-58%; median, 30%)6-10,16-29; however, the prevalence of readmission was low (approximately 16%), and there were no deaths. These data demonstrate the complexity of the procedure and the need for an experienced surgical team and a well-equipped hospital, regardless of the technique used. No relation was found between the complications and the timing of reconstruction or the adjuvant treatment received by the patient, probably because the authors knew which technique would be most suitable for each case. This hypothesis was confirmed by an incidence of complications similar to that described in the literature, the favorable long-term outcomes of reconstructions, and the low rates of hospital readmission.
The use of AMs, despite allowing fast and simple breast reconstruction when there is adequate skin preservation and without distant flaps, usually presents specific complications that often require readmission. The percentage of capsular contracture Baker III/IV observed in this study (6.3%) is lower than that in other publications, ranging from 10% to 56% (median, 28% for a follow-up time of approximately 3 years)13-15,23-29. Capsular contracture has an increased incidence when the reconstructed breast received radiation therapy after the implantation of AM, even in the presence of a myocutaneous flap cover, as demonstrated in the 3 cases of reconstruction with LD. Reconstruction with AM only after irradiation was not performed in the group of patients in this study, probably because of the relative contraindication of this technique.
In this study, total reconstruction with distant myocutaneous flaps showed good aesthetic results, especially in cases involving major skin loss; however, the procedures were more complex and had longer operative times than those of other reconstruction techniques. Because other body surfaces are involved, these techniques have unique complications16,19,20,22 such as seroma at the donor site (abdomen in TRAM and dorsal region in LD). Some authors have described a reduction in the incidence of seroma by using adhesion sutures at donor sites after muscle flaps removal19,22. Scevola et al.20 analyzed 768 breast reconstructions with TRAM and deduced that the use of 2 drains in the abdomen may reduce the incidence of seroma.
Other common complications specific to total reconstructions with TRAM are the development of hernias and abdominal bulging, resulting from weakness of the abdominal wall secondary to resection of the rectus abdominis. Ascherman et al.30 reasoned that such complications could be related to the amount of muscle used to create the flap; they found no statistical difference in the incidence of these complications when compared with single-pedicle or double-pedicle TRAM flaps. One factor that appears to contribute to the decrease in these complications is a careful reconstruction of the abdominal wall with nonabsorbable mesh by planes31.
As the focus of this study was the clinical complications of total breast reconstructions, long-term analysis was crucial. The main limitation of this study was the small sample size, owing to the strict inclusion criteria and the large loss to follow-up because the follow-up period was longer than one year. Nevertheless, we identified fairly consistent results for complications resulting from total breast reconstructions. The long period of postoperative follow-up and the normal and proportionate distribution of patients treated with each type of total breast reconstruction technique permitted adequate statistical comparisons between the techniques, their main complications, and the individual patient factors related to these complications.
CONCLUSIONS
Breast reconstruction provides satisfactory results. However, throughout the clinical course, complications of low severity is common; these complications are usually treated with clinical therapy alone, and readmission is not required. Reconstructions with AMs, while generally being more simple and with less surgical comorbidity, have a higher incidence of rehospitalization for the treatment of complications than techniques that do not use these materials. Each technique has its indications, contraindications, and complications. The application of each technique should be individualized according to the individual characteristics of the patient in order to obtain better results, thus avoiding short- and long-term complications.
REFERENCES
1. Veronesi U, Saccozzi R, Del Velcchio M, Banfi A, Clemente C, De Lena M, et al. Comparing radical mastectomy with quadrantectomy, axillary dissection, and radiotherapy in patients with small cancers of the breast. N Engl J Med. 1981;305(1):6-11.
2. Fisher B, Anderson S. Conservative surgery for the management of invasive and noninvasive carcinoma of the breast: NSABP trials. National Surgical Adjuvant Breast and Bowel Project. Word J Surg. 1994;18(1):63-9.
3. Freeman BS. Subcutaneous mastectomy for benign breast lesions with immediate or delayed prosthetic replacement. Plast Recontr Surg Transplant Bull. 1962;30:676-82.
4. Veiga DF, Veiga-Filho J, Ribeiro LM, Archangelo I Jr, Balbino PF, Caetano LV, et al. Quality-of-life and self-esteem outcomes after oncoplastic breast-conserving surgery. Plast Reconstr Surg. 2010;125(3):811-7.
5. Bellino S, Fenocchio M, Zizza M, Rocca G, Bogetti P, Bogetto F. Quality of life of patients who undergo breast reconstruction after mastectomy: effects of personality characteristics. Plast Reconstr Surg. 2011;127(1):10-7.
6. Hudson DA, Skoll PJ. Complete one-stage, immediate breast reconstruction with prosthetic material in patients with large or ptotic breasts. Plast Reconstr Surg. 2002;110(2):487-93.
7. Hammond DC, Capraro PA, Ozolins EB, Arnold JF. Use of a skin-sparing reduction pattern to create a combination skin-muscle flap pocket in immediate breast reconstruction. Plast Reconstr Surg. 2002;110(1):206-11.
8. Derderian CA, Karp NS, Choi M. Wise-pattern breast reconstruction: modification using AlloDerm and a vascularized dermal-subcutaneous pedicle. Ann Plast Surg. 2009;62(5):528-32.
9. Nava MB, Cortinovis U, Ottolenghi J, Riggio E, Pennati A, Catanuto G, et al. Skin-reducing mastectomy. Plast Reconstr Surg. 2006;118(3):603-10.
10. Losken A, Collins BA, Carlson GW. Dual-plane prosthetic reconstruction using the modified wise pattern mastectomy and fasciocutaneous flap in women with macromastia. Plast Reconstr Surg. 2010;126(3):731-8.
11. Neumann CG. The expansion of an area of skin by progressive distention of a subcutaneous balloon; use of the method for securing skin for subtotal reconstruction of the ear. Plast Reconstr Surg. 1957;19(2):124-30.
12. Almeida Júnior GL, Macedo JLS, Borges SZ, Souza AO, Henriques FAM, Suschino CMH, et al. Reconstrução mamária imediata após cirurgia conservadora do câncer de mama. Rev Soc Bras Cir Plást. 2007;22(1):10-8.
13. Bronz G, Bronz L. Mammareconstruction with skin-expander and silicone prostheses: 15 years' experience. Aesthetic Plast Surg. 2002;26(3):215-8.
14. Ringberg A, Tengrup I, Aspegren K, Palmer B. Immediate breast reconstruction after mastectomy for cancer. Eur J Surg Oncol. 1999;25(5):470-6.
15. Munhoz AM, Aldrighi C, Montag E, Arruda EG, Aldrighi JM, Filassi JR, et al. Periareolar skin-sparing mastectomy and latissimus dorsi flap with biodimensional expander implant reconstruction: surgical planning, outcome, and complications. Plast Reconstr Surg. 2007;119(6):1637-49.
16. Atisha D, Alderman AK. A systematic review of abdominal wall function following abdominal flaps for postmastectomy breast reconstruction. Ann Plast Surg. 2009;63(2):222-30.
17. Rietjens M, Urban CA, De Lorenzi F, Bonato Jr A. Reconstrução mamária com retalho miocutâneo do músculo reto abdominal (TRAM). In: Mélega JM, Montoro AF, Albertoni WM, eds. Cirurgia plástica fundamentos e arte: cirurgia reparadora de tronco e membros. Rio de Janeiro: MEDSI; 2004. p.92-6.
18. Wilkins EG, August DA, Kuzon WM Jr, Chang AE, Smith DJ. Immediate transverse rectus abdominis musculocutaneous flap reconstruction after mastectomy. J Am Coll Surg. 1995;180(2):177-83.
19. Baroudi R, Ferreira CA. Seroma: how to avoid it and how to treat it. Aesthet Surg J. 1998;18(6):439-41.
20. Scevola S, Youssef A, Kroll SS, Langstein H. Drains and seromas in TRAM flap breast reconstruction. Ann Plast Surg. 2002;48(5):511-4.
21. Sigurdson L, Lalonde DH. Breast reconstruction. Plast Reconstr Surg. 2008;121(1 Suppl):1-12.
22. McCarthy C, Lennox P, Germann E, Clugston P. Use of abdominal quilting sutures for seroma prevention in TRAM flap reconstruction: a prospective, controlled trial. Ann Plast Surg. 2005;54(4):361-4.
23. Lejour M, Alemanno P, De Mey A, Gerard T, Duchateau J, Eder H, et al. Analysis of 56 breast reconstructions using the latissimus dorsi flap. Ann Chir Plast Esthet. 1985;30(1):7-16.
24. Tschopp H. Evaluation of long-term results in breast reconstruction using the latissimus dorsi flap. Ann Plast Surg. 1991;26(4):328-40.
25. Christensen BO, Overgaard J, Kettner LO, Damsgaard TE. Long-term evaluation of postmastectomy breast reconstruction. Acta Oncol. 2011;50(7):1053-61.
26. McCraw JB, Maxwell GP. Early and late capsular "deformation" as a cause of unsatisfactory results in the latissimus dorsi breast reconstruction. Clin Plast Surg. 1988;15(4):717-26.
27. Bostwick J 3rd, Scheflan M. The latissimus dorsi musculocutaneous flap: a one-stage breast reconstruction. Clin Plast Surg. 1980;7(1):71-8.
28. Lejour M, Jabri M, Deraemaecker R. Analysis of long-term results of 326 breast reconstructions. Clin Plast Surg. 1988;15(4):689-701.
29. Tarantino I, Banic A, Fischer T. Evaluation of late results in breast reconstruction by latissimus dorsi flap and prosthesis implantation. Plast Reconstr Surg. 2006;117(5):1387-94.
30. Ascherman JA, Seruya M, Bartsich SA. Abdominal wall morbidity following unilateral and bilateral breast reconstruction with pedicled TRAM flaps: an outcomes analysis of 117 consecutive patients. Plast Reconstr Surg. 2008;121(1):1-8.
31. Oliveira Junior FC, Mélega JM, Pinheiro AS, Destro C, Maciel PJ. Comparação entre a utilização da tela de Marlex em um e dois planos para a reconstrução da parede abdominal pós-TRAM. Rev Bras Cir Plást. 2010;25(Supl. 1):49.
1. Master, PhD student at the Universidade Estadual de Campinas (UNICAMP), plastic surgeon, full member of the Sociedade Brasileira de Cirurgia Plástica/Brazilian Society of Plastic Surgery (SBCP), São Paulo, SP, Brazil
2. Resident of Plastic Surgery at the Santa Cruz Institute of Plastic Surgery (ICPSC), São Paulo, SP, Brazil
3. Head Professor of the Department of Obstetrics and Gynecology, UNICAMP, Campinas, SP, Brazil
Correspondence to:
Francisco Claro Jr.
Av. Indianópolis, 2.244 - Planalto Paulista
São Paulo, SP, Brazil - CEP 04062-000
E-mail: drfranciscoclarojr@cplastica.org.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: December 13, 2012
Article accepted: February 21, 2013
Funding in the form of grant was received from the Coordination of Development of Personnel of Higher Education (CAPES - Coordenação de Aperfeiçoamento de Pessoal de Nível Superior).
This study was performed at the Department of Obstetrics and Gynecology, Universidade Estadual de Campinas (UNICAMP), Campinas, SP, Brazil and at the Santa Cruz Plastic Surgery Institute (ICPSC - Instituto de Cirurgia Plástica Santa Cruz), São Paulo, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter