

Original Article - Year 2013 - Volume 28 - Issue 1
Breast augmentation via the abdominoplasty incision approach: a prospective study of 100 cases
Aumento mamário por meio da incisão da abdominoplastia: estudo prospectivo de 100 casos
ABSTRACT
INTRODUCTION: Pregnancy and obesity cause distension of the abdominal wall and produce changes in the shape and size of the breasts. Thus, the need of aesthetic improvement of the abdominal area is not uncommon, coinciding with the desire for breast augmentation. Performing mammoplasty via the abdominoplasty incision approach was first described in 1976. Because of the lack of prospective studies using this approach, we performed a series of dermolipectomy procedures using the abdominal incision to insert a pair of silicone gel breast implants.
METHODS: In total, 100 consecutive patients were selected, with a mean age of 33 ± 2 years. Classic abdominoplasty was performed, and 2 tunnels were then made in the right and left hypochondria. After implant placement, the mammary fold was reconstructed using simple sutures with absorbable threads to attach the subcutaneous tissue to the aponeurosis.
RESULTS: None of the following complications were observed: deep-vein thrombosis, cardiorespiratory or anesthetic complications, skin necrosis, visible bleeding, hematoma, or clinically detectable infection. The volume of the implants ranged from 280 to 450 mL (median, 350 mL). The mean operation time was 116 minutes. Reoperation was not necessary in any of the cases. The monitoring period ranged from 9 to 84 months (mean, 36 months).
CONCLUSIONS: Breast augmentation via the abdominoplasty incision approach was demonstrated to be a reliable and simple technique, providing a new, scar-free alternative to mammary surgical procedures.
Keywords: Plastic surgery. Mammaplasty. Breast implantation. Breast/surgery. Abdomen/surgery. Abdominoplasty. Lipectomy.
RESUMO
INTRODUÇÃO: A gravidez e a obesidade causam distensão da parede abdominal e também produzem mudanças na forma e no tamanho das mamas. Assim, não é incomum a necessidade de melhoria estética da área abdominal, coincidindo com o desejo de aumento de mama. A mamoplastia utilizando a mesma incisão da abdominoplastia foi descrita pela primeira vez em 1976. Em decorrência da falta de estudos prospectivos empregando essa abordagem, os autores realizaram uma série de dermolipectomias usando a incisão abdominal para inserir o par de implantes mamários de silicone gel.
MÉTODO: Cem pacientes consecutivas foram selecionadas, com média de idade de 33 ± 2 anos. A abdominoplastia clássica foi realizada e, em seguida, confeccionados 2 túneis sobre os hipocondrios direito e esquerdo. Após colocação dos implantes, foi realizada reconstrução do sulco mamário com pontos simples usando fios absorvíveis, fixando o subcutâneo à aponeurose.
RESULTADOS: Não houve nenhuma das seguintes complicações: trombose venosa profunda, complicações cardiorrespiratórias ou anestésicas, necrose de pele, sangramento visível, e hematoma ou infecção detectáveis clinicamente. O volume dos implantes variou de 280 ml a 450 ml (mediana de 350 ml). O tempo médio de operação foi de 116 minutos. Em nenhum caso foi necessária reoperação. O período de acompanhamento mínimo foi de 9 meses e máximo, de 84 meses (média de 36 meses).
CONCLUSÕES: A técnica de aumento mamário por meio da incisão da abdominoplastia se mostrou confiável e simples, constituindo uma nova opção para a cirurgia mamária sem cicatriz nas mamas.
Palavras-chave: Cirurgia plástica. Mamoplastia. Implante mamário. Mama/cirurgia. Abdome/cirurgia. Abdominoplastia. Lipectomia.
Pregnancy and obesity cause distension of the abdominal wall, resulting in diastasis of the muscle aponeurosis in the region. To correct these alterations, plastic surgeons perform abdominoplasty or abdominal dermolipectomy, which are also used to repair the following 3 most common defects: excessive skin, excessive subjacent fat, and musculoaponeurotic laxity1-3. Moreover, plastic surgeons have found that performing dermolipectomy in combination with musculoaponeurotic plication may be effective in restoring a satisfactory and graceful abdominal shape.
Pregnancy does not produce changes exclusively in the abdominal wall. The female body as a whole experiences modifications as a result of hormonal alterations. A significant change is observed in the shape and size of the breasts as they are prepared to produce milk. The skin is stretched as the breast grows, and may eventually develop stretch marks. The increase in blood supply to the breast causes the appearance of bluish veins; in addition, the areolas and papillae may become darker and expanded. After breastfeeding, laxity and involution of the parenchyma are commonly present. Breast ptosis is 2 times more frequent in postpartum women than in nulliparous women4-7. Thus, the need to improve the aesthetics of the abdominal region in conjunction with the desire to increase breast size is not uncommon8,9.
Data from the International Society of Aesthetic Plastic Surgery10 revealed that breast augmentation is the second most frequently performed plastic surgery procedure, with more than 1,506,475 cases in 2010 alone. In the case of breasts with a small volume prior to pregnancy, a simple prosthesis implantation may provide the desired effect, and can thus restore the self-confidence, self-image, and self-esteem of a woman.
The main goal in any plastic surgery procedure is to provide the best result with the smallest possible scar, by concealing the scar or making the incision in places that are not easily visible. Several techniques, incision types, and approaches have been used for breast augmentation. The final decision depends on physical and regional characteristics, with consideration of the surgeon's recommendations and the patient's preference11-14.
Planas15 was the first to report on augmentation mammoplasty via the abdominoplasty incision approach. The introduction of silicone implants was performed through subcutaneous tunnels made in the region of the right and left hypochondria, reaching the retroglandular plane15-20. The technical difficulty associated with this technique may be due to the great distance of the anatomic structure to be dissected during tunnel construction and establishment of the implantation site. Moreover, confirmation of hemostasis and suture preparation for the prevention of caudal migration of the implant, asymmetry, and seroma formation become difficult without the proper equipment and an endoscope17,21-23. Owing to the lack of prospective studies implementing this technique, we conducted a series of dermolipectomy procedures using an abdominal incision to insert silicone gel breast implants.
METHODS
A total of 100 consecutive patients who wanted to undergo abdominoplasty and breast augmentation between January 1, 2006, and August 31, 2011, were enrolled in this study. The age of the patients at the time of surgery ranged from 21 to 56 years (mean, 33 ± 2 years; median, 30 years).
The inclusion criteria were as follows:
The exclusion criteria were as follows:excessive abdominal skin and fat, and diastasis of the rectus abdominis muscle (patients with Matarasso24 type II body types); desire and indication for breast augmentation; age between 20 and 60 years; body mass index lower than 35 (overweight and obesity grade 1).
Surgical Techniqueany contraindication to the indicated clinical-surgical procedure; patients previously subj ected to bariatric surgery by laparotomy; patients at recent postpartum period (< 1 year) or who were breastfeeding; patients with acute or chronic uncontrolled disease; patients who refused to participate in the study or who did not return for postoperative evaluation; need of any incision for the removal of skin or previous scars in the breast.
All the surgical procedures were conducted at the hospital and under general anesthesia. A transverse suprapubic incision was performed, and the detachment of the dermalfat flap was made just above the aponeurosis of the rectus abdominis muscle and partly on the external oblique muscle to the height of the xiphoid appendix.
An infiltration solution was prepared before resection of the hypochondrium region and the lower region of the breasts, and administered using 60-mL syringes, at a total dose of 300 mL for each breast. A long cannula (3 mm) was connected to the tip of the syringes to facilitate the infiltration (Figure 1).
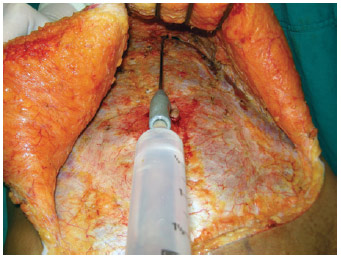
Figure 1 - Infiltration into the area to be removed from the region under the breast.
Tunnels were created over the costal arches to reach the retroglandular space, at 1 o'clock and 11 o'clock positions (Figure 2). Meters were used to create symmetrical sites to determine the appropriate implant size (Figure 3). Small fragments were resected via electrocautery using Allis clamps, with the base of the breast disconnected from the pectoralis fascia to reduce breast volume (Figure 4).
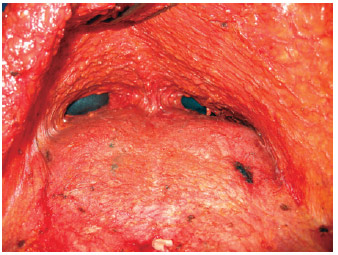
Figure 2 - The tunnels created to access the breast over the costal arches.

Figure 3 - Volumetric analysis using molds and a profile comparison with the original breast.
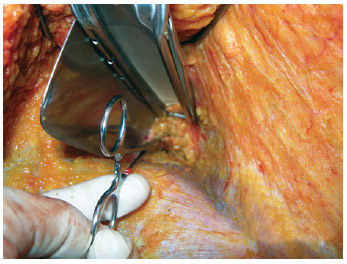
Figure 4 - Resection of fragments of the larger breast to obtain better symmetry.
The prosthesis used was composed of a high-profile cohesive gel silicone with a textured wrap, and volume ranging from 260 to 450 mL. The reconstruction of the mammary fold was performed with a simple suture after implant placement, using a polyglactin 2-0 absorbable thread, fixing the subcutaneous tissue to the aponeurosis. The same operation was performed with several sutures in the dissected tunnels (Figures 5 and 6).
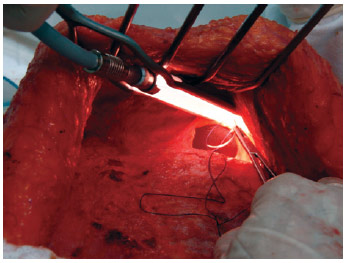
Figure 5 - Reconstruction of the mammary fold and protection of the prosthetic suture needle.
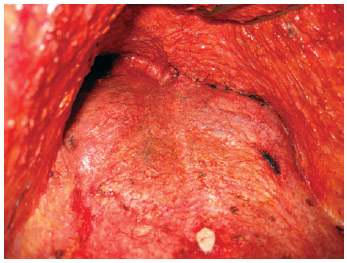
Figure 6 - Complete tunnel fixation.
The abdominal diastasis of the rectus abdominis muscle was corrected using a simple and interrupted suture with a 2-0 monofilament nylon thread, at a distance of approximately 2.5 cm, followed by continuous suture with the same thread over the existing sutures. After confirmation of hemostasis, the abdominal flap was fixed to the aponeurosis of the rectus abdominis muscle with at least 30 simple sutures using polyglactin, leaving spaces < 5 cm between the sutures13-15. The umbilical scar was fixed in its new position in the abdominal flap, using external and subdermal sutures with a 4.0 nylon thread. Finally, a non-allergenic adhesive tape was placed over the skin of the base of the breast to assist coaptation and prevent serosal collection. The bandage was maintained for 7 days.
All the surgical procedures were performed in the morning, and the patients were discharged on the following day.
RESULTS
None of the following complications were observed: deep-vein thrombosis, pulmonary embolism, anesthesia-related or cardiopulmonary complications, skin necrosis, visible bleeding, hematoma, or clinically detectable infection. A small dehiscence (< 5 cm) was detected in 6 patients. Dehiscence of major proportions was not observed in any other case. One patient developed seroma, which was resolved after 2 punctures and the associated use of a compression bandage.
The size of the implants ranged from 280 to 450 mL, with a mean of 350 mL. All the implants used were of the same model, high profile, and textured surface with cohesive silicone gel. The surgery duration (excluding the anesthesia period between intubation and extubation) ranged from 93 to 154 minutes, with a mean of 116 minutes. Reoperation as a result of hematoma, seroma, or suture dehiscence was not required in any patient. The monitoring period ranged from 9 to 84 months, with a mean of 36 months. During the monitoring period, contracture was not observed in any patient.
For critical analysis of the frontal-view photographs of all the patients, we drew a line from the front of the sternal furcula down to the navel. Based on this line, another perpendicular line was digitally drawn across the center of the right nipple, as well as an additional one at the base of the same breast.
Perfect symmetry was not found in any of the 100 women in the study; that is, every woman differed in height, distance of the breast to the medial line, and breast size. Thus, achieving perfect breast symmetry was the primary goal.
After surgery, a photographic evaluation revealed that asymmetric position was still present in 26 patients (26%), although all of them were satisfied with the result. Figures 7 to 13 depict some of the surgical outcomes of the present cases.

Figure 7 - In A and C, preoperative appearance. In A, frontal and in C, lateral views. In B and D, appearance at 12 months after bilateral placement of 375 mL, high-profile, textured, silicone gel breast implants. In B, frontal and in D, lateral views.
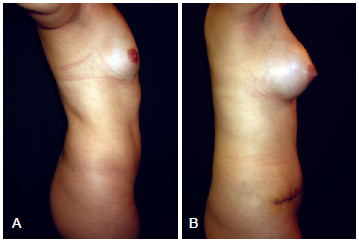
Figure 8 - In A, preoperative appearance at a right-side view. In B, appearance (right-side view) after bilateral placement of 300 mL, high-profile, textured, silicone gel breast implants.
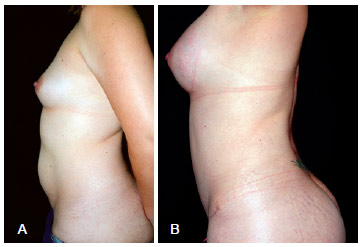
Figure 9 - In A, preoperative appearance at a left-side view. In B, appearance (left-side view) at 7 months after bilateral placement of 325 mL, high-profile, textured, silicone gel breast implants.
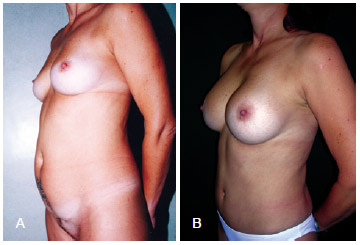
Figure 10 - In A, Preoperative appearance at a left oblique view. In B, appearance (left oblique view) at 8 months after bilateral placement of 350 mL, high-profile, textured, silicone gel breast implants.
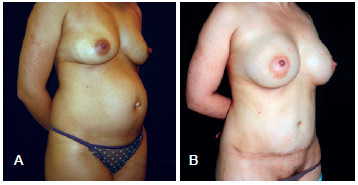
Figure 11 - In A, preoperative appearance at a right oblique view. In B, appearance (right oblique view) at 6 months after bilateral placement of 325 mL, high-profile, textured, silicone gel breast implants.

Figure 12 - In A, appearance (right oblique view) at 12 months after bilateral placement of 375 mL, high-profile, textured, silicone gel breast implants.

Figure 13 - Appearance (frontal view) at 6 months after bilateral placement of 400 mL, high-profile, textured, silicone gel breast implants, demonstrating a transverse abdominal scar resulting from the 2 surgeries, which could be hidden under the underwear.
DISCUSSION
Women candidates for abdominoplasty usually also request for breast augmentation. Access to the breast through the incision in abdominoplasty may avoid the formation of a scar in an anatomically significant area.
The technique described herein is simple and based on principles abundantly described in medical literature. Planas15 first published the outcomes of this approach, between 1972 and 1976, in 12 patients. Barrett and Kelly16 compared the abdominal access in 8 women, and 2 distinct incisions (abdominal and breast) were performed in 4 of the women. Differences in relation to the clinical evolution of the patients were not found, regardless of the surgical technique applied. Wallach18 reported 6 cases of breast augmentation via the abdominoplasty incision approach, after reviewing 70 consecutive abdominoplasty procedures. Dini et al.20 reported a series of 30 patients, and highlighted the importance of reattaching the mammary fold and tunnels to the costal arches to prevent seroma15-20. In the present study, complications were associated with the small number of sutures used to reduce the dead space in the tunnels (i.e., the more the better) and the excessively tight adhesion sutures in the fold (Figures 14 and 15). After the study period, the seroma noted in 1 case was no longer observed owing to the 2 punctures applied and the associated use of a compression bandage. A poorly fixed fold may be improved with subsequent release of one or another suture with a needle, taking utmost care to not perforate the implant or further aggravate the aesthetic result with destruction of the mammary fold.

Figure 14 - Seroma resulting from inadequate fixation (due to very few adhesion sutures).

Figure 15 - Postoperative appearance demonstrating an uneven and too tight fixation of the mammary fold.
The ideal candidates for breast augmentation via the abdominal incision approach are patients without ptosis, pseudoptosis, or first-degree mammary ptosis. In contrast, better results may be obtained with mastopexy in patients with second or third-degree ptosis who desire breast augmentation.
Our study population was composed of young women with a mean age of 33 years, similar to the data reported by Barrett and Kelly16. Among the 100 patients in this study, 84 were primiparous, 9 had 2 pregnancies, and 7 had 3 or more pregnancies. All the patients had their implants inserted in the subglandular plane according to our preference, even though submuscular insertion is easier. The release of the pectoralis major muscle near the rectus abdominis is associated with a greater amount of bleeding an greater tunnel size. Therefore, we suggest the use of the following long instruments because of the great distance of the anatomical structure to be dissected: a 22-cm needle holder, an electrocautery extender, a 5-cm malleable retractor, long Kelly clamps, Allis clamps, and most importantly, the longest available illuminated retractor (approximately 25 cm).
The dissection necessary to reach the mammary fold may cause some discomfort to the novice surgeon because it is necessary to change the direction of the dissection, that is, from a rise to the edge of the first rib encountered to a slope in the direction of the pectoral muscle. Once the dissection is directed downward, the surgeon may be hesitant to enter the pleural laminas. However, such fear is unfounded because such dissection is completely performed under direct vision. After raising the inferior part of the breast, a decision must be made as to whether surgical site preparation should be performed under or over the pectoral muscle. Although using the subpectoral plane is more laborious, it is completely feasible.
Endoscopic techniques may be easily incorporated into the surgical arsenal but are more laborious than beneficial in this kind of surgery. A strict hemostasis in the retroglandular site is not necessary given the option to operate via the subglandular plane. Resection of the mammary gland is performed via electrocautery until the release of the mammary fold. Thereafter, the dissection is made only by blunt dissection using the fingers. The inability to move forward only with the fingers indicates that the mammary fold has not yet been crossed. Occasionally, the fingers are not long enough to detach the upper pole of the breast. In such cases, rectified malleable retractors are useful, as they have a rounded tip. The retractors used for gluteal implants are not suitable for this resection because the surgical site should be constructed as round as possible. An improper resection may result in an angled and unnatural shape of the breasts. The aim is to perform traction of the pectoral muscle using forceps to help create a suitable site. However, the surgeon should have be prepared to use a long Kelly clamp and electrocautery extender in case of any eventual hemostasis.
The use of molds helps achieving a perfect symmetry and they assist in establishing hemostasis by compression while the surgeon operates the other side by detaching the tunnel and contralateral site. Small adjustments in the size of the breast may be performed through resection of portions of the breast base, using Allis clamps, and resecting it to the desired volume via electrocautery. In some cases not pertaining to this series, we performed the removal of glandular gynecomastia in men who lost weight and required abdominoplasty, while avoiding incisions in the breast skin.
When critically analyzing the frontal-view photographs of the 100 patients, we found that breast asymmetry is a natural feature of the normal human body. Therefore, surgeons need to discuss with the patient if she wants the center of the implant coinciding with the center of the nipples so that the superior medial pole of the breasts will be at different heights and distances from the sternal midline. It seems more appropriate to place the implant in the most central and symmetrical position in terms of height even if the nipples are not symmetrical, considering that the use of a décolletée shirt exposes the upper medial quadrant of the breast.
This aspect is controversial, but the final decision should be made by the patient. A preoperative consent form must be discussed with, and signed by the patient. In the consent form, the patient indicates her preference regarding whether to keep one breast larger than the other, according to the nipple symmetry at birth, or to place the implant in a more medial position, without concern of the immutable position of the nipple.
During breast resection, hemostasis with electrocautery or suture may not be necessary in case of injury to any large vessel, as placing 3 or 4 compresses soaked in 0.9% saline solution with the addition of adrenaline 1:500.000 for 10 minutes would be enough to stop the abundant bleeding while the surgeon works on the contralateral side or initiates plication of the rectus abdominis muscle diastasis. For the present series of patients, reoperation for revision due to bleeding or hematoma was not required. However, it was imperative to create a site with the exact size of the prosthesis to be implanted. A silicone implant in a tight site would compress the sectioned vessels.
The reconstruction of the mammary fold is the key point of the technique described herein. The technique involves simple sutures, using an absorbable polyglactin 2-0 thread with a needle > 2.5 cm. The number of sutures is another important detail, as it must be sufficient to allow perfect coaptation of the arched mammary fold. Few sutures may provide a fragmented appearance to the fold. Although such sutures do not present any difficulty, the surgeon must be patient to remove and replicate them as many times as necessary until a natural-looking mammary fold and perfect symmetry are achieved. The smaller the dissected tunnel, the easier the suturing; however, the surgeon must make an adequately sized tunnel in order to allow mobility during the construction of the surgical site. For inexperienced surgeons, the tunnel should allow an easy and extensive release of the mammary fold and ensure careful reattachment. In addition, it should provide enough space for the surgeon to insert one hand underneath the breast. Once the surgeon's experience with this technique increases, smaller tunnels may be made and surgery duration will be shorter than that in traditional breast incisions.
The release of the mammary fold is an important technical detail, which should not be performed completely from the medial and lateral sides. However, in cases where this occurs, recreating the fold will likely result in breasts with a square base. It is important to note that the fold has a semicircular structure and to ensure that the sutures for recreating the base of the breast should not be too tight; otherwise, they will create marks in the skin. If a suture is found marking the skin during the postoperative period, the suture may be cut under local anesthesia using a "pink" needle (caliber 40 ' 1.2 mm).
In this surgical procedure, the surgeon's gloves are often stained with blood and thus must be cleaned along with the patient's skin to accurately perceive the ideal fold. It is essential that the surgeon does not consider fixing the incision with a bandage and tape compression on the skin, as curatives do not replace a poor-quality suture. However, if the result of the sutures of the fold in the aponeurosis attachment is not satisfactory, the sutures should be redone as many times as necessary to avoid unacceptable results. For inexperienced surgeons, such sutures present a high level of difficulty and stress, at which point they often ask, "Why am I doing this?" However, over time, this can become the easiest part of the surgery. Breast surgery via the abdominal incision approach is much faster than the 2 surgical procedures performed separately through 3 incisions (2 in the breasts and 1 in the abdomen).
Further, we recommend not implementing this surgical approach without the proper equipment, including a long illuminated retractor and an electrocautery extender, to avoid stress. Adequate retroglandular infiltration is also required. If an intercostal artery is sectioned, it is imperative that the surgeon is ready to clamp the vessel with a long Kelly clamp or a similar instrument. If blood obscures the implantation site, the subsequent dissection will be more difficult. Dissection of the internal part of the implantation site is easier to perform with a malleable retractor. The malleable retractor must be held with the index finger, using the tip of the retractor as if it were an extension of the finger, and we should aim to dissect the target site to yield the desired size. The malleable retractor will also be useful to deviate and protect the prosthesis during the closing of the site to achieve a well-defined mammary fold.
In this study, no surgical drainage was performed or required, as all the blood and plasma flowed through the tunnels. Despite being subjective observations, our findings reveal that the recovery with the present surgical approach was much faster and the intumescences of the breast disappeared at an earlier stage.
If we compare the risk involved between performing breast augmentation and abdominoplasty separately (with 3 different incisions), and via an abdominal incision, as proposed in this study, the only difference is the dissection of 2 hypogastric tunnels. In general, these tunnels do not reach the path of the superior superficial epigastric artery or separate the intercostal arteries and veins below the height of the xiphoid appendix, and thus they are not associated with an increased risk of abdominal devascularization (Figure 1). Only a small suture dehiscence (< 5 cm) was identified in 6 cases, which is the same ratio found in previously reported cases of isolated abdominoplasty.
Psychologically, the patient feels much safer to shower on the day after the surgery, without fear of breaking some sutures on the breast skin. Another extremely important point is the patient's satisfaction in having her breasts enlarged with no scars, as the breasts are one of the most erogenous parts of the body. Thus, the patient does not need to undergo months of uncertainty and tension because she can be assured of an aesthetically acceptable scar. In addition, the patient would be free from any risk of dehiscence, scar widening, skin color changes (hyperpigmentation or hypochromy), or keloids in her breast.
The abdominoplasty incision technique is excellent for patients who need subglandular implants and prefer a distant incision. It provides a good control of dissection and allows the use of silicone gel implants, thereby avoiding the risk of deflation. Moreover, the recovery is faster because there is no risk of rupturing sutures in the breast skin, with fewer injuries and less pain owing to minimal cauterization and fewer incisions in the breast tissue. Less aggression to the mammary ducts is also possible because the breast is detached from the pectoral fascia as a whole.
CONCLUSIONS
Breast augmentation via the abdominal incision approach provides patients the opportunity to restore their appearance with an easy-to-hide scar. Furthermore, the complications associated with the present technique do not differ from those associated with the traditional technique involving the use of 3 incisions.
REFERENCES
1. Trussler AP, Kurkjian TJ, Hatef DA, Farkas JP, Rohrich RJ. Refinements in abdominoplasty: a critical outcomes analysis over a 20-year period. Plast Reconstr Surg. 2010;126(3):1063-74.
2. Dini GM. A new position to hide the abdominoplasty scar. Plast Reconstr Surg. 2007;119(4):1391-2.
3. Dini GM, Ferreira LM. Putting the umbilicus in the midline. Plast Reconstr Surg. 2007;119(6):1971-3.
4. Rohrich RJ, Adams WP Jr, Potter JK. A review of psychological outcomes and suicide in aesthetic breast augmentation. Plast Reconstr Surg. 2007;119(1):401-8.
5. Burk J, Zelen SL, Terino EO. More than skin deep: a self-consistency approach to the psychology of cosmetic surgery. Plast Reconstr Surg. 1985;76(2):270-80.
6. Sarwer DB, Bartlett SP, Bucky LP, LaRossa D, Low DW, Pertschuk MJ, et al. Bigger is not always better: body image dissatisfaction in breast reduction and breast augmentation patients. Plast Reconstr Surg. 1998;101(7):1956-61.
7. Aboudib JH Júnior, Castro CC, Coelho RS, Cupello AM. Analysis of late results in postpregnancy mammoplasty. Ann Plast Surg.1991;26(2):111-6.
8. Brito MJ, Nahas FX, Barbosa MV, Dini GM, Kimura AK, Farah AB, et al. Abdominoplasty and its effect on body image, self-esteem, and mental health. Ann Plast Surg. 2010;65(1):5-10.
9. Dini GM, Ferreira LM. Fat necrosis and dermolipectomy. Plast Reconstr Surg. 2007;119(6):1970-1.
10. ISAPS Procedure Study, 2010; Disponível em: http://www.isaps.org/isaps-global-statistics.html.
11. Rohrich RJ, Hartley W, Brown S. Incidence of breast and chest wall asymmetry in breast augmentation: a retrospective analysis of 100 patients. Plast Reconstr Surg. 2006;118(7 Suppl):7S-13S.
12. Rohrich RJ, Adams WP Jr, Potter JK. A review of psychological outcomes and suicide in aesthetic breast augmentation. Plast Reconstr Surg. 2007;119(1):401-8.
13. Rohrich RJ, Cunningham BL, Jewell ML, Spear SL. Teenage breast augmentation: validating outcome data and statistics in plastic surgery. Plast Reconstr Surg. 2005;115(3):943-4.
14. Spear SL, Bulan EJ, Venturi ML. Breast augmentation. Plast Reconstr Surg. 2004;114(5):73E-81E.
15. Planas J. Introduction of breast implants through the abdominal route. Plast Reconstr Surg. 1976;57(4):434-7.
16. Barrett BM Jr, Kelly 2nd MV. Combined abdominoplasty and augmentation mammaplasty through a transverse suprapubic incision. Ann Plast Surg. 1980;4(4):286-91.
17. Hakme F, Gomes BS, Toledo OMR, Sjostedt CO, Muller PM. Prevenção e tratamento da contratura capsular. Rev Bras Cir. 1984;74(2):59-64.
18. Wallach SG. Maximizing the use of the abdominoplasty incision. Plast Reconstr Surg. 2004;113(1):411-7.
19. Wallach SG. Transabdominal breast augmentation. Aesthet Surg J. 2004;24(4):373-8.
20. Dini GM, Albuquerque LG, Masako LM. Prótese de mama usando a via de acesso abdominal. In: Ferreira LM, ed. Guia de cirurgia plástica. Barueri: Manole; 2007. p.539-43.
21. Baroudi R, Ferreira CA. Seroma: how to avoid it and how to treat it. Aesthet Surg J. 1998;18(6):439-41.
22. Hanra S. Circunferential body lift. Aesthet Surg J. 1999;19(3):244-8.
23. Nahas FX, Ferreira LM, Ghelfond C. Does quilting suture prevent seroma in abdominoplasty? Plast Reconstr Surg. 2007;119(3):1060-4.
24. Matarasso A. Classification and patient selection in abdominoplasty. Oper Tech Plast Reconstr Surg. 1996;3:7.
1. Physician, Affiliate Professor, Graduation Supervisor, Chief of the Rhinoplasty Sector of the Discipline of Plastic Surgery (UNIFESP-EPM), plastic surgeon, full member of the Sociedade Brasileira de Cirurgia Plástica/Brazilian Society of Plastic Surgery (SBCP), São Paulo, SP, Brazil
2. Undergraduate student of medicine (UNIFESP-EPM), São Paulo, SP, Brazil
3. Physician, graduated at the City of São Paulo University (UNICID), São Paulo, SP, Brazil
4. Plastic Surgeon, Medical Collaborator of the Discipline of Plastic Surgery (UNIFESP-EPM), associate member of the SBCP, São Paulo, SP, Brazil
5. Plastic Surgeon, graduated at UNIFESP-EPM, associate member of the SBCP, São Paulo, SP, Brazil
6. Full Professor of the Discipline of Plastic Surgery and of the Graduation Program (UNIFESP-EPM), full member of the SBCP, São Paulo, SP, Brazil
Correspondence to:
Gal Moreira Dini
Rua Vicência Faria Versage, 400 - ap. 113-114 - Jardim Emília
Sorocaba, SP, Brazil - CEP 18031-080
E-mail: dr.gal@uol.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: November 28, 2012
Article accepted: February 10, 2013
This study was performed at the Department of Plastic Surgery, Federal University of São Paulo - Paulista School of Medicine (UNIFESP-EPM), São Paulo, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter