

Original Article - Year 2013 - Volume 28 -
Neo-omphaloplasty in anchor-line abdominoplasty performed in patients who have previously undergone bariatric surgery
Neo-onfaloplastia no decurso das abdominoplastias em ancora em pacientes pos-cirurgia bariatrica
ABSTRACT
INTRODUCTION: In formerly morbidly obese individuals, major weight loss after bariatric surgery leads to the development of extensive areas of sagging skin with large fat deposits that mainly affect the limbs, several regions of the trunk, and the anterior abdominal wall in particular. The gold standard procedure, anchor-line abdominoplasty (also known as inverted T), is performed with the simultaneous removal of the navel followed by neo-umbilicoplasty during surgery. In the present report, we describe our experience with neo-omphaloplasty in anchor-line abdominoplasty performed in patients who previously underwent bariatric surgery. The neo-omphaloplasty mainly consists of 2 skin flaps bilaterally positioned at the extremities of the skin incision, facilitating a natural appearance of the navel after they are sutured to the fascia.
METHODS: From March 2011 to June 2012, 50 patients, who previously underwent bariatric surgery and had stable body weight for at least 6 months, were operated on at the Plastic Surgery Service of the Clinics Hospital of the Faculty of Medicine of the University of Campinas.
RESULTS: In the 50 patients, the neo-umbilicus was positioned at a location that was preoperatively established, and these patients exhibited characteristics similar to individuals who had not undergone abdominal surgeries. There was no evidence of dehiscence, necrosis, stenosis, suture line enlargement in the neo-umbilicus, or seroma formation in this cohort.
CONCLUSIONS: When neo-omphaloplasty is performed using 2 skin flaps conventionally positioned in the abdominal wall, at a distance varying between 16 and 18 cm from the xiphoid process, the aesthetic outcomes are similar to the natural appearance of the navel. This technical approach is quick and easy to implement.
Keywords: Umbilicus/surgery. Abdomen/surgery. Bariatric surgery. Surgery, plastic/methods.
RESUMO
INTRODUÇÃO: As grandes perdas ponderais pós-cirurgia bariátrica resultam, nos ex-obesos mórbidos, em grande flacidez cutânea nas áreas mais volumosas, com maiores depósitos adiposos nos membros, nas diversas regiões do tronco e, particularmente, na parede anterior do abdome. A abdominoplastia em âncora, também chamada tipo T invertido, tem sido o procedimento de eleição pelos especialistas, com ressecção concomitante do umbigo, seguida da neoumbilicoplastia no ato operatório. O objetivo do presente estudo é descrever nossa experiência com a técnica de neo-onfaloplastia no decurso das abdominoplastias em âncora em pacientes pós-cirurgia bariátrica, que consiste, basicamente, na utilização de 2 retalhos cutâneos, bilateralmente posicionados nas bordas da pele incisada, que, suturados à fáscia, determinam a umbilicação de aspecto natural.
MÉTODO: Entre março de 2011 e junho de 2012, foram operados, pela Disciplina de Cirurgia Plástica do Hospital das Clínicas da Faculdade de Medicina da Universidade de Campinas, 50 pacientes submetidos a cirurgia bariátrica prévia, com estabilização do peso corpóreo por, no mínimo, 6 meses.
RESULTADOS: Nos 50 pacientes operados, o neoumbigo ficou posicionado no local estabelecido pré-operatoriamente, apresentando características semelhantes às de indivíduos sem histórico de cirurgia abdominal prévia. Não ocorreram deiscência, necrose, estenose, alargamento das linhas de sutura no neoumbigo ou seromas nessa série de casos.
CONCLUSÕES: A neo-onfaloplastia com emprego de 2 retalhos cutâneos e padronização de seu posicionamento na parede abdominal, distante 16 cm a 18 cm do apêndice xifoide, permitiu resultado estético compatível com o aspecto natural da cicatriz umbilical. Essa abordagem técnica é de fácil e rápida execução.
Palavras-chave: Umbigo/cirurgia. Abdome/cirurgia. Cirurgia bariátrica. Cirurgia plástica/métodos.
Major cutaneous/adipose dysmorphic disorders in morbidly obese patients lead to physical and psychological changes. Multidisciplinary treatment aims to restore patients to normal conditions in a cost-effective manner. The effects of bariatric surgeries have already been established in the literature. However, they are frequently associated with dystrophies of the integumentary system. Despite the known risk of formation of major scars, patients undergo several surgical procedures for excess skin removal.
In all cases, the navel is the body part that evokes different reactions in patients in cases of absence or distortion of the navel, from trying to solve the problem to investigating the possibility of surgical treatment for its maintenance. This is because the navel is psychologically considered as part of the body. When patients are inquired about the possible removal of the navel, most individuals of both genders express their desire that the navel be retained1-3.
Several omphaloplasty procedures that are performed in cases undergoing lower pubic transverse abdominoplasty or even in cases of total necrosis of the navel have been published in the literature4-8. In anchor-line abdominoplasty, in which the navel is routinely removed, umbilicus reconstruction is performed with 1 or 2 skin flaps, which are shaped as a small tongue and placed on one of the extremities of the residual skin with a pedicle. Once sutured to the fascia, the appearance is similar to the natural navel9-14.
Here, we report our experience with neo-omphaloplasty in anchor-line abdominoplasty performed in patients who had previously undergone bariatric surgery. This procedure involves the use of 2 skin flaps that are bilaterally positioned at the extremities of the skin incision, which mimic the natural appearance of the navel once they are sutured to the fascia.
METHODS
From March 2011 to June 2012, 50 patients, who previously underwent bariatric surgery with stable body weight for at least 6 months, were operated on at the Plastic Surgery Service of the Clinics Hospital of the Faculty of Medicine of the University of Campinas. Most patients (90%) were women.
All patients underwent the anchor-line procedure, in which the neo-umbilicus was reconstructed with the aid of 2 skin flaps that were bilaterally positioned at the extremities of residual skin flaps.
Surgical resection limits
With the patient in the orthostatic position, a xiphoid-pubic line was established up to the anterior vulvar commissure in women and up to the base of the penis in men. With the patient in the dorsal horizontal decubitus position, another line, 6 cm above the line described above, was drawn bilaterally and transversally to each side of the iliac spine. Through a digital maneuver, starting from the iliac-pubic line, the upper limit was traced through a transverse and bilateral line. The area assumed the shape of a large ellipse with extremities that varied according to the excess skin and fat.
After stretching the skin caudally, another bidigital maneuver was used to define the epigastric excess, from the xiphoid process to the upper transversal limit at the level of the navel; these new epigastric lines formed an "A" shape. Finally, 2 small cutaneous rectangles (2 cm in width and 3 cm in height) were defined bilaterally 16 to 18 cm below the xiphoid process and medially to the vertical limits of the resection (Figures 1 and 2).
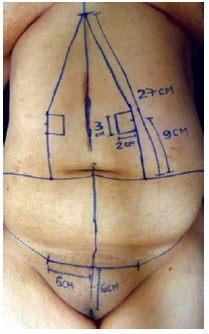
Figure 1 - Frontal view defining the neo-umbilicus in the epigastrium. Limits of 6 cm were drawn bilaterally to the midline and at a distance of 6 cm from the vulvar commissure; they define the lower transversal incision of the inverted T and the position of the vertical suture line after excess skin removal.
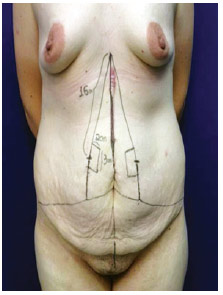
Figure 2 - Frontal and profile views of the cutaneous surgical limits. A xiphoid-pubic line, followed by vertical bidigital epigastric clamping in the transverse umbilicus-pubic direction, defines the excess skin to be removed. A xiphoid superior transverse line of approximately 27 cm in length is divided into three 9-cm segments. The 2 skin quadrilaterals drawn at the level of the neo-umbilicus and measuring 3 × 2 cm are located at a distance of 16 to 18 cm from the xiphoid process and help in reconstructing the neo-umbilicus.
Surgical procedure
Patients underwent general anesthesia with or without epidural anesthesia. Infiltration was performed with 0.9% saline solution and 1:500,000 epinephrine. A skin incision was subsequently made along the entire resection limit. Dissection and monoblock resection of the entire overlying skin were performed with electrocautery until the aponeurotic plane, including the navel and its pedicle, was reached. The umbilical stump was invaginated and sutured when necessary (Figure 3). Rectus abdominis muscles were plicated by suturing the aponeurosis in 2 planes using 2-0 nylon thread isolated sutures every 5 cm followed by 0 Vicryl continuous sutures. With the patient in Fowler's position, the limits of the 2 hemi-skin flaps were sutured at the pubic midline with 0 Vicryl isolated sutures. The 2 bilateral and rectangular skin flaps were sutured medially to the aponeurosis of the rectus abdominis muscles with two 2-0 nylon thread isolated sutures, while the extremities were sutured with 4-0 nylon thread (Figures 4 to 6). The remaining vertical and horizontal sutures on the extremities of the skin; the superficial fascia, and dermis were performed using isolated 0 Vicryl sutures followed by continuous intradermal 3-0 Monocryl sutures.
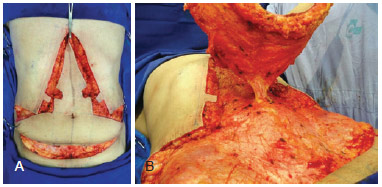
Figure 3 - Intraoperative appearance after the resection of excess skin and amputation of the umbilicus pedicle at its base, with defined quadrangular skin flaps
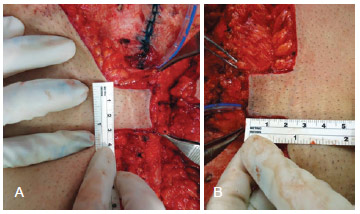
Figure 4 - Rectangular skin flaps (measuring 3 cm in height and 2 cm in width), with no resection of the cellular subcutaneous tissue
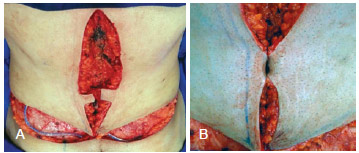
Figure 5 - Extremities of the flaps sutured at the midline, corresponding to the muscular fascia
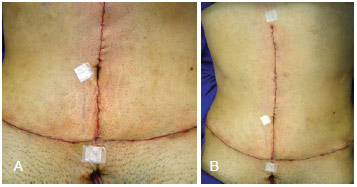
Figure 6 - Final postoperative aspect, with the xiphoid-umbilical distance ranging between 16 and 18 cm. The vertical aspect of the navel varies among operated patients; it usually remains elongated for months and opens once the skin enlarges.
Adhesive strips were applied in dead space areas. A suction drain was placed in the central area of the pubis, emerging through the skin, and was maintained for 7 days.
Dressing involved applying an adhesive sterile and porous bandage on the entire suture, which was then covered with cotton and elastic strip. Dry gauze was maintained within the neo-umbilicus for 24 hours.
RESULTS
In the 50 operated patients, the neo-umbilicus was positioned as established preoperatively and presented characteristics similar to individuals not previously submitted to abdominal surgeries (Figures 7 to 10).

Figure 7 - A 38-year-old female patient who underwent anchor-line abdominoplasty and neo-umbilicoplasty using the procedure described herein after major weight loss. In A, preoperative aspect, frontal view. In B, 6 months postoperatively, frontal view.
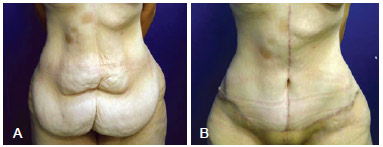
Figure 8 - A 31-year-old female patient who underwent anchor-line abdominoplasty and neo-umbilicoplasty using the procedure described herein after major weight loss. In A, preoperative aspect, frontal view. In B, 3 months postoperatively, frontal view.
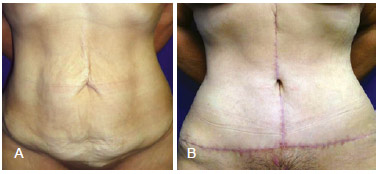
Figure 9 - A 62-year-old female patient who underwent anchor-line abdominoplasty and neo-umbilicoplasty using the procedure described herein after major weight loss. In A, preoperative aspect, frontal view. In B, 2 months postoperatively, frontal view.
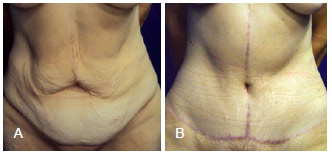
Figure 10 - Distances of 16.5- and 18-cm from the xiphoid to the neo-umbilicus.
There was no appearance of dehiscence, necrosis, stenosis, suture line enlargement in the neo-umbilicus, or seroma formation in this cohort.
DISCUSSION
Systematic removal of the navel in patients undergoing abdominoplasty after bariatric surgery is based on the preoperative characteristics presented by individual patients, such as a large pedicle. Conventional umbilicoplasty involves surgical maneuvers that often result in dysmorphic disorders postoperatively, such as stenosis or enlargement of the navel, hypertrophic scar on a skin island, wound dehiscence, and pedicle necrosis, which often require surgical revision.
The neo-umbilicoplasty, based on the use of 2 skin flaps, described in this article is similar to other procedures described in the literature. However, it differs with respect to the conventional surgical limits, which are defined irrespective of the physical characteristics of the patient, weight loss, skin extension, or adipose panniculus thickness9-14. A distance of approximately 16 to 18 cm below the xiphoid process is a more aesthetically acceptable position, even for healthy individuals or patients who have previously undergone lower pubic transverse abdominoplasty. To determine this distance, xiphoid-umbilical measurements were performed in 15 healthy individuals with normal weight and height while they were placed in the orthostatic position. The distance ranged between 16 and 18 cm, with an average of 16.5 cm. The xiphoid process was a more accurate reference point than the vulvar commissure because of factors inherent to the adipose-cutaneous component of each individual.
The surgical maneuvers used for this procedure are quick and easy to implement; they only require the fixation of 2 skin flaps to the aponeurotic plane through isolated sutures of skin extremities and no removal of the overlaying fat. Moreover, specific dressing is not necessary, because the gauze is maintained inside the neo-umbilicus for 24 hours.
Patients are instructed to clean their neo-umbilicus with soap and water as well as place new dry gauzes daily for 4 weeks postoperatively. Placement of an elastic bandage to cover the trunk, from the inframammary groove up to the thighs, is recommended for 3 months.
Patients are allowed to perform light physical activities such as walking and water aerobics 1 month after surgery. However, weight training and abdominal exercises are recommended only 3 months after surgery.
CONCLUSIONS
Neo-omphaloplasty, using 2 skin flaps that are conventionally positioned in the abdominal wall at a distance varying between 16 and 18 cm from the xiphoid process, yields aesthetic outcomes similar to the natural appearance of the navel. This technical approach is quick and easy to implement.
REFERENCES
1. Francischi RPP, Pereira LO, Freitas CS, Klopfer M, Santos RC, Vieira P, et al. Obesidade: atualização sobre sua etiologia, morbidade e tratamento. Rev Nutr. 2000;13(1):17-28.
2. Visscher TL, Seidell JC. The public health impact of obesity. Annu Rev Public Health. 2001;22:355-75.
3. Furtado IR, Nogueira CH, Lima Jr EM. Cirurgia plástica após a gastroplastia redutora: planejamento das cirurgias e técnicas. Rev Soc Bras Cir Plást. 2004;19(2):35-40.
4. Avelar JM. Cicatriz umbilical: da sua importância e técnica de confecção nas abdominoplastias. Rev Bras Cir. 1979;69(1/2):41-52.
5. Ribeiro L, Muzy S, Accorsi A. Omphaloplasty. Ann Plast Surg. 1991;27(5):457-75.
6. Nogueira DSC. Neo-onfaloplastia de rotina em abdominoplastias. Rev Bras Cir Plást. 2008;23(3):207-13.
7. Baroudi R, Carvalho C. Neoumbilicoplastias. Un procedimiento eclético en el transcurso de las abdominoplastias. Cir Plast Iberolatinoam. 1981;7(4):391-401.
8. Silva FN, Oliveira EA. Neo-onfaloplastia na abdominoplastia vertical. Rev Bras Cir Plást. 2010;25(2):330-6.
9. Cavalcanti ELF. Neoumbilicoplastia como opção de reconstrução umbilical nas dermolipectomias abdominais em âncora pós-gastroplastia. Rev Bras Cir Plást. 2010;25(3):509-18.
10. Pfulg M, Van de Sijpe K, Blondeel P. A simple new technique for neoumbilicoplasty. Br J Plast Surg. 2005;58(5):688-91.
11. Franco T, Franco D. Neoomphaloplasty: an old and new technique. Aesthetic Plast Surg. 1999;23(2):151-4.
12. Franco D, Medeiros J, Farias C, Franco T. Umbilical reconstruction for patients with a midline scar. Aesthetic Plast Surg. 2006;30(5):595-8.
13. el-Dessouki NI, Shehata SM, Torki AM, Hashish AA. Double half-cone flap umbilicoplasty: a new technique for the proboscoid umbilical hernia in children. Hernia. 2004;8(3):182-5.
14. Tardelli HC, Vilela DB, Schwartzmann GLE, Azevedo M, Mello Jr AM, Farina Jr JA. Padronização cirúrgica das abdominoplastias em âncora pós-gastroplastia. Rev Bras Cir Plást. 2011;26(2):266-74.
1. Resident physician of the Plastic Surgery Service of the Faculty of Medicine of the State University of Campinas (UNICAMP), Campinas, SP, Brazil
2. Plastic surgeon, specialist member of the Sociedade Brasileira de Cirurgia Plástica/Brazilian Society of Plastic Surgery (SBCP), Campinas, SP, Brazil
3. Plastic surgeon, full member of the SBCP, Campinas, SP, Brazil
4. Plastic surgeon, full member of the SBCP, head of the Plastic Surgery Service of the Faculty of Medicine of the State University of Campinas (UNICAMP), Campinas, SP, Brazil
5. Plastic surgeon, associate member of the SBCP, assistant surgeon of the Plastic Surgery Service of the Faculty of Medicine of UNICAMP, Campinas, SP, Brazil
Correspondence to:
Brenda Artuzi Reno
Rua Jasmim, 750 - ap. 52 - Chácara Primavera
Campinas, SR Brazil - CEP 13087-460
E-mail: beartuzi@yahoo.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: November 11, 2012
Article accepted: February 2, 2013
This study was performed at the Plastic Surgery Service of the Faculty of Medicine of the State University of Campinas (UNICAMP), Campinas, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter