

Original Article - Year 2013 - Volume 28 -
Laser lipolysis with a 980-nm diode laser: experience with 400 cases
Laserlipolise com diodo 980 nm: experiencia com 400 casos
ABSTRACT
INTRODUCTION: Liposuction has undergone several improvements since its first description, including changes in the cannulas, variation in the concentration of the infiltrating solution, and the use of different devices and technologies. The use of laser technology devices for lipolysis and stimulation of skin retraction has contributed to the procedure. This article presents the authors' experience with laser lipolysis in 400 patients, within a 5-year period, and discusses the principles of the technology and its effect on tissues.
METHODS: This is a study performed between July 2007 and July 2012 and included 400 patients who underwent laser lipolysis. All procedures were performed following the original protocol - infiltration of cold saline, passage of the cannula with an optic fiber for conducting the energy needed for laser lipolysis, skin retraction, and finally, conventional liposuction.
RESULTS: Hospitalization type ranged from outpatient to overnight surgery. Approximately 45% (180 of 400) of patients had minimal bruising, with involvement of 2% or more of the affected body surface. Hematoma, seroma, and dehiscence occurred in a total of 9% (36 of 400) of patients. We did not find any case of thermal burn of the skin.
CONCLUSIONS: Laser lipolysis performed according to the described technique was safe and reproducible.
Keywords: Lasers. Lipolysis. Subcutaneous fat. Connective tissues.
RESUMO
INTRODUÇÃO: A técnica de lipoaspiração recebeu várias contribuições desde sua primeira descrição, como modificações nas cânulas, variação na concentração da solução de infiltração e uso de aparelhos com tecnologias variadas. A utilização de aparelhos com tecnologia laser vem contribuir com o procedimento por meio da lipólise e com o estímulo de retração cutânea. Neste artigo é apresentada a experiência dos autores com a laserlipólise em 400 pacientes, no intervalo de 5 anos, sendo discutidos aspectos dos princípios da tecnologia e sua ação sobre os tecidos.
MÉTODO: Estudo realizado entre julho de 2007 e julho de 2012, que incluiu 400 pacientes submetidos a procedimento de laserlipólise. Os procedimentos foram realizados seguindo protocolo original, com infiltração de soro gelado, passagem da cânula com fibra óptica para a condução da energia laser visando à laserlipólise, retração cutânea e, por último, lipoaspiração convencional.
RESULTADOS: O período de internação variou de cirurgia em regime ambulatorial a pernoite. Cerca de 45% (180/400 pacientes) dos pacientes evoluíram com equimoses mínimas, com acometimento de 2% ou mais da superfície corporal comprometida. Os casos de hematoma, seroma e deiscência totalizaram 9% (36/400 pacientes). Em nenhum caso foi constatada queimadura por lesão térmica na pele.
CONCLUSÕES: O procedimento de laserlipólise realizado com a técnica descrita demonstrou segurança e reprodutibilidade.
Palavras-chave: Lasers. Lipólise. Gordura subcutânea. Tecido conjuntivo.
Since 1983, with the publication by Illouz1 of a series of > 3,000 cases of liposuction for lipodystrophy, as an initial or complementary treatment, liposuction has been recognized as a plastic surgery for the treatment of body contour irregularities. Regardless of the method, this consists of a procedure in which the surgeon decreases the fat content in such a way that the skin will naturally adapt to this reduction of fatty tissue volume, either through spontaneous elasticity or by exogenous stimulation.
Since the first descriptions of the liposuction technique, the principle of vacuum removal of fat tissue has remained. Initially, a dry technique was performed, consisting of direct aspiration without infiltration, which was efficient in the removal of fat. However, the trauma caused by friction against tissue resulted in hematomas with severe blood loss, bruises, and therefore long-lasting inflammatory processes, triggering fibrosis and skin irregularities. With the availability of infiltration solutions with vasoconstrictors in various concentrations, the results became more uniform, with less bleeding, less risk, and shorter recovery periods2. Nevertheless, it was still a traumatic and aggressive technique, with a high percentage of complications, some of which were fatal.
Technological advances seen in recent years, such as the development of ultrasonic liposuction and vibroliposuction, has brought benefits to patients, such as decreased tissue trauma, and also largely to surgeons, with a reduction in the physical stress of the surgery.
The introduction of laser technology in liposuction initially generated considerable doubts about its effectiveness in the treatment of tissue, owing to the use of inadequate equipment with unsuitable wavelengths or without water affinity/absorption in the target fat tissue3.
Relevant scientific studies that relate some wavelengths (e.g., 980 nm) to a high affinity/absorption of the water contained in the adipocytes have demonstrated the efficacy and safety of the use of laser in liposuction4,5.
With the application of laser liposuction, there is a reduction of mechanical trauma to the surrounding tissues, which translates into less fibrosis and reduced bleeding due to clotting of the blood vessels. This provides the benefits of postoperative comfort and a more rapid recovery6. In addition, considerable tissue retraction, both immediate and delayed, is achieved by stimulating collagen formation7.
The selective photothermal, photochemical, and photoacoustic properties of laser have long been known; however, it is only recently being used as a treatment for joint optimization of the results of lipoplasty8. The use of this technology for lipolysis and stimulation of collagen formation has been shown to be effective9.
The aim of this article is to present the experience of 400 consecutive cases of laser lipolysis performed by the authors using a 980-nm diode laser, as an adjuvant procedure in liposuction.
METHODS
In this retrospective, observational study, 400 patients who underwent laser lipolysis, between July 2007 and July 2012, were evaluated. Of them, 285 patients were operated on in the private practice of one of the authors (P.C.) in Peru, and 115 patients were from private clinics of the other authors in Brazil. Two hundred eighty patients underwent surgical treatment with laser lipolysis liposuction only, and the rest received laser lipolysis as an adjuvant treatment with other surgeries such as abdominoplasty and mammoplasty.
The average age of the patients at operation was 29 years (range 18-52 years). Twenty-eight patients were men and 257 were women.
All patients completed an informed consent form and underwent preoperative routine exams with hematology and cardiology assessment.
The treated areas varied and included the abdomen, flanks, back, submental area, inner thighs, and inner arms.
The procedures were performed in the hospital, and the type of anesthesia was general, regional (epidural), or local with sedation, according to the extent and indications of each case.
The standard infiltration technique of Centurion et al.5 was used, using a 0.9% saline solution with a temperature of around 4ºC, and 1:500,000 epinephrine. The infiltration was performed preferably with the aid of a continuous pressure system at 150 mm Hg, provided by placing the reservoir solution with a cuff pressure drop, to allow a homogeneous distribution during infusion with a 2-mm-diameter Klein needle. A uniform deposit was performed only in the deepest layer, parallel to the muscular plane, to avoid tunneling the fat tissue. The infused volume was equivalent to the estimated volume drawn from each region. This infiltration technique took 7 to 8 min to infuse 1 liter into each decubitus, an adequate period for vasoconstriction.
A 980-nm-wavelength diode laser (ORLight®) equipment was used in all treatments. A 2-mm-diameter rigid cannula with a 600-µm optical fiber was used to transfer energy to the tissues. The passage of the laser was initiated in the deep layers, with slow fan-shaped movements, at a rate of about 2.5 cm/s, from the incision, with application of back-and-forth laser movements, always with the free control of the operator's hand on the treated region to maintain the distance from the end of the fiber to the surface. At the end of the outward stroke of each passage, the fiber end was maintained at a safe distance from the skin, with the aid of a red light display, in order to avoid injury. After the passage of the cannula into the deeper plane, passes were made with the same care in the middle plane, and then the more superficial plane to the skin surface.
For body treatment, power was maintained between 18 and 22 W, except in the submental region, inner arms, and thighs, where 14 to 16 W was used.
To stimulate the cutaneous retraction of the treated area after laser lipolysis, the cannula passes were made with the laser fiber in a subdermal position with the end directed toward the surface. The foot pedal was operated only in the outward movement (Figure 1). This passage was also fan-shaped from the incision, under the visual control of the red light from the fiber end, with a speed of not less than 5 cm/s. In this maneuver, with the operator's free hand laid flat on the skin surface, the increase in temperature was monitored by touch.

Figure 1 - Intraoperative stimulation of skin retraction ("skin tightening"), with the end of the laser cannula at the subdermal level with continuous firing only in the outward path.
After the passage of the laser cannula for lipolysis and skin retraction, conventional liposuction was performed. Straight and curved 4-mm and 3.5-mm cannulas were used. The vacuum system used was mixed, obtained by a 60 mL syringe, and with the liposuction apparatus. First, the deeper plane was aspirated, then the intermediate portion, and finally superficial liposuction was performed, always with slow movements.
RESULTS
The complications observed in this series of patients who underwent laser lipolysis are listed in Table 1.
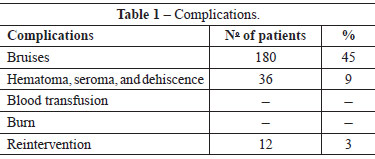
The bruises observed did not account for the total aspirated area but for 2% or more of the affected body surface area. We followed the measurement convention that the size of a palm is equivalent to 1% of the total body surface.
Hospitalization ranged from outpatient to overnight surgery. The use of non-opioid analgesics was sufficient for pain control.
The cases of reintervention were all for volume under-correction, which was performed under local anesthesia in a hospital setting, with an interval of 6 months after the first procedure.
There were cases with small areas of fibrosis, which resolved spontaneously or receded after complementary treatment with local ultrasound (Manthus®, KLD).
Figure 2 illustrates the good results obtained with the technique.
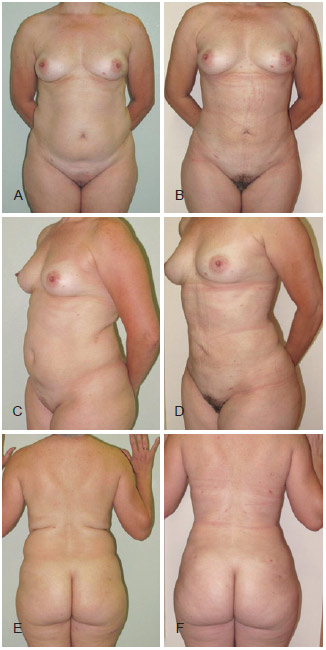
Figure 2 - In A, C, and E, preoperative pictures of the abdomen and back of a patient who underwent laser lipolysis with a 980-nm diode laser: anterior view, left oblique view, and posterior view, respectively. In B, D, and F, postoperative (1 month after the procedure) pictures: front view, left oblique view, and rear view, respectively.
DISCUSSION
Traditional liposuction performed with local infiltration and aspiration with a syringe or other equipment are established procedures. However, the search for more uniform results, with shorter postoperative recovery periods and greater stimulation of skin contraction and collagen stimulation is a challenge for all plastic surgeons.
The interaction of the laser with tissue occurs through the absorption of light energy by chromophores (structures sensitive to a specific wavelength), which produces sufficient heat to achieve thermal damage. The heat acts on fat cells, causing apoptotic cell damage and affecting the extracellular matrix. In adipose tissue, adipocytes contain > 90% of lipids, are arranged in clusters, and between them are components such as water, septa, nerves, vessels, capillaries, and connective tissue elements.
Laser lipolysis began with the use of the Nd:YAG laser (1064 nm) to produce photothermolysis. This wavelength does not have an absorption/affinity for either water or fat4,10. The laser in this wavelength has to be applied for an extended time to raise the temperature of the tissue and cause vaporization of adipocytes. The longer application time in tissue raises the skin temperature close to 40ºC. Some authors recommended this method as appropriate for skin retraction, but cases of burns led to the discredit of laser lipolysis. When the skin temperature reaches 40ºC, the temperature of the subcutaneous tissue (SCT) becomes higher than 42ºC, and because the melting temperature of fat is lower than that of the skin, we can infer that significant damage is caused to the SCT.
The diode laser (980 nm) emerged as a smaller device that is cheaper to maintain. The established chromophore for this band is intra- and extracellular water. Eventually, it was discovered that human fat has an absorption curve different from that of water upon laser exposure - that is, higher energy absorption by fat - which allows lipolysis to occur without the need for high energy11. The low power generated at 980 nm increases the adipocyte size to 100 µm. The heat generated by the laser alters the sodium and potassium balance in the cell membrane, which leads to the passage of extracellular fluid into the intracellular space4,8.
The 980-nm diode laser has an established application as an adjuvant tool in liposuction. In this system, water is the chromophore, and laser lipolysis, through photochemical effects (e.g., changes in adipocyte membrane permeability) and photothermal effects (direct adipocyte injury), has been shown to be an excellent method for uniform dissolution.
With an energy of 990 J per 10 cm2 and a depth of up to 3 cm, the laser can be used to the desired effect, eliminating the need for simultaneous control of percutaneous temperature gauges. To reduce the possibility of skin damage and prevent burn cases such as that described in the literature, in the first 25 cases, the authors performed temperature measurements with the aid of an infrared thermometer (EXTECH) (Table 1). The temperature never exceeded 32ºC; therefore, the tissues were protected from a possible burn. During the laser application, a noise could be heard during the passage of the cannula deep in the tissue, similar to the sound of hot oil in a pan, owing to the previously infused cold solution, without noticing damage to the skin. Good skin retraction was still obtained by the selective action of the 980-nm wavelength with relative water affinity/absorption. These data were important to the learning curve with the sensitive manual control of the authors.
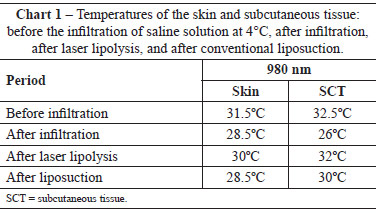
The use of cold saline infiltration before the procedure protected the surrounding tissue from inadvertent heating by the laser. The saline temperature (4ºC) showed no systemic effect, considering that the body temperature of 36.4ºC under the epidural effect decreased to 36ºC after < 10 min. The application of the laser once again increased the SCT and skin temperature to the baseline values before the infiltration. This contributed not only to the dispersion of the temperature increase in the path of the fiber but also in aiding in vasoconstriction and potentiating the desired effect with the use of epinephrine.
In the first 25 cases, tissues were also withdrawn, such as done in abdominoplasty. Slides of ex vivo materials were made for histological assessment after the passage of the laser and to visualize the changes in the adipose and connective tissues (Figures 3 and 4).
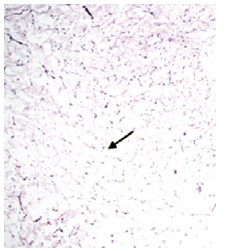
Figure 3 - Histological slide of fat tissue stained with hematoxylin and eosin, visualized under an optical microscope at 40' amplification. Note that the adipose tissue was partially conserved by 30% after the application of the 980-nm laser (arrow).
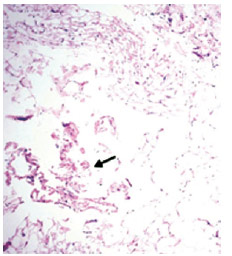
Figure 4 - Histological slide of connective tissue stained with hematoxylin and eosin, visualized under an optical microscope at 40' amplification. Note that the modified connective tissue was partially conserved at 10% after the application of the 980-nm laser (arrow).
The coagulation of the microvasculature surrounding the tunnels markedly decreased the amount of blood in the lipoaspirate, reducing not only the immediate local bruising but also the stains, which rapidly resolved postoperatively.
Postoperative analgesia was restricted to the use of anti-inflammatory analgesics for at most 3 days, without the use of opioids. Patients who had previously undergone liposuction with the conventional technique (without laser) reported less postoperative pain and a faster recovery compared with their previous experience. The action of the laser in the innervation surrounding the path of the laser fiber promotes paresthesia and even transient anesthesia, increasing patient comfort postoperatively. In the group of patients included in this study, the use of analgesics was based on the presence of pain.
The use of the same diode (980 nm) laser for "skin tightening" shows its versatility for use in complementing procedures. The subdermal stimulation, with care in speed, caused no damage to the skin. By performing a pinch test intraoperatively, the effect, triggered by collagen remodeling in the dermis, was immediately seen by the surgeon. From the first day, upon removal of the compression dressing, uniform accommodation of tissue with minimal surface irregularity was observed. There was a progressive evolution in skin retraction in the first 3 months, due to the neocollagenesis induced by the laser. This effect seemed to be more intense in the submental region, inner thighs, and inner arms, areas previously considered "taboo" but can now be treated safely and effectively.
With time and power accumulated in a particular region, the passage of the cannula with the laser fiber presents reduced resistance. In cases of secondary liposuction, in which fibrosis is intense, we observed a sustainable breach of fibrotic bands postoperatively.
CONCLUSIONS
The use of lipolysis with a 980-nm diode laser as an adjunct to liposuction was safe and reproducible. The observed results confirm that the diode laser is a reliable option with good outcome for patients undergoing liposuction.
REFERENCES
1. Illouz YG. Body contouring by lipolysis: a 5-year experience with over 3000 cases. Plast Reconstr Surg. 1983;72(5):591-7.
2. Klein JA. Tumescent technique for regional anesthesia permits lidocaine doses of 35 mg/kg for liposuction. J Dermatol Surg Oncol. 1990;16(3):248-63.
3. Weiss RA, Beasley K. Laser-assisted liposuction using a novel blend of lipid- and water-selective wavelengths. Lasers Surg Med. 2009;41(10):760-6.
4. Mordon S, Eymard-Maurin AF, Wassmer B, Ringot J. Histologic evaluation of laser lipolysis: pulsed 1064-nm Nd:YAG laser versus CW 980-nm diode laser. Aesthet Surg J. 2007;27(3):263-8.
5. Centurion P, Cuba JL, Noriega A. Liposucción con diodo laser 980-nm. (LSDL 980-nm): optimización de protocolo seguro en cirugía de contorno corporal. Cir Plást Ibero-Latinoam. 2011;37(4):355-64.
6. Goldman A. Submental Nd:Yag laser-assisted liposuction. Lasers Surg Med. 2006;38(3):181-4.
7. Apfelberg D. Laser-assisted liposuction may benefit surgeons, patients. Clin Laser Mon. 1992;10(12):193-4.
8. Anderson RR, Farinelli W, Laubach H, Manstein D, Yaroslavsky AN, Gubeli J 3rd, et al. Selective photothermolysis of lipid-rich tissues: a free electron laser study. Laser Surg Med. 2006;38(10):913-9.
9. Alexiades-Armenakas M. Combination laser-assisted liposuction and minimally invasive skin tightening with temperature feedback for treatment of the submentum and neck. Dermatol Surg. 2012;38(6):871-81.
10. Wassmer B, Zemmouri J, Rochon P, Mordon S. Comparative study of wavelengths for laser lipolysis. Photomed Laser Surg. 2010;28(2): 185-8.
11. Badin AZ, Gondek LB, Garcia MJ, Valle LC, Flizikowski FB, Noronha L. Analysis of laser lipolysis effects on human tissue samples obtained from liposuction. Aesthetic Plast Surg. 2005;29(4):281-6.
1. M.Sc. in Plastic Surgery, plastic surgeon, full member of the Sociedade Brasileira de Cirurgia Plástica/Brazilian Society of Plastic Surgery (SBCP), managing partner of the Núcleo de Plástica Avançada, São Paulo, SP, Brazil
2. Plastic surgeon, full member of the SBCP, managing partner of the Núcleo de Plástica Avançada, São Paulo, SP, Brazil
3. Plastic surgeon, specialist member of the SBCP, director of the Cosmopolitan Institute, Passo Fundo, RS, Brazil
4. Professor, Universidade Peruana de Ciências Aplicadas Laureate International Universities, plastic surgeon, full member of the Peruvian Society of Plastic, Reconstructive and Aesthetic Surgery, Lima, Peru
Correspondence to:
Rodrigo de Faria Valle Dornelles
Rua Capitão Macedo, 419 - Vila Mariana
São Paulo, SP, Brazil - CEP 04021-020
E-mail: rodrigodornelles@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article submitted: December 3, 2012
Article accepted: March 1, 2013
This study was performed at the authors' private clinic at São Paulo, SP, Brazil, and Lima, Peru.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter