

Case Report - Year 2013 - Volume 28 - Issue 1
Lower lip reconstruction using the Karapandzic technique
Reconstrução do lábio inferior pela técnica de Karapandzic
ABSTRACT
Reconstruction of extensive labral lesions has always been a challenge for plastic surgeons. Thus far, an optimal lip reconstruction technique has not yet been established. This report includes 2 cases of large lower lip defects, affecting 80% and 60% of the surface structure that resulted from laceration/contusion trauma and epidermal tumor resection, respectively. The patients underwent lip reconstruction using the Karapandzic technique, which was first described in 1974. In the first case, the result was considered unfavorable because of dehiscence. In the second case, good functional and aesthetic results were obtained without from the patchwork or bruises. The Karapandzic technique is easy to perform and may be considered a reproducible option for lip reconstruction with good functional and aesthetic results.
Keywords: Lip/surgery. Surgical flaps. Reconstructive surgical procedures.
RESUMO
Lesões labiais extensas sempre representaram um desafio para a cirurgia plástica. Não existe técnica ideal para reconstrução labial. Neste artigo são relatados os casos de 2 pacientes que apresentavam grandes defeitos no lábio inferior, acometendo 80% e 60% da superfície dessa estrutura, após traumatismo lacerocontuso e ressecção de tumor epidermoide, respectivamente. Esses pacientes foram submetidos a reconstrução labial pela técnica de Karapandzic1, descrita em 1974. No primeiro caso, o resultado foi considerado desfavorável, em decorrência da presença de deiscência. No segundo caso, foi obtido bom resultado estético e funcional, sem sofrimento dos retalhos ou hematomas. A técnica de Karapandzic constitui uma opção de fácil execução e reprodutível, apresentando bons resultados estéticos e funcionais.
Palavras-chave: Lábio/cirurgia. Retalhos cirúrgicos. Procedimentos cirúrgicos reconstrutivos.
In terms of aesthetics and functionality, the face is an important human attribute, being the most visible portion of the body with delicate and complex structures. The upper and lower lips constitute the oral orifice and are responsible for a number of bodily functions such as speech articulation, mastication, facial mimicry, and salivary continence. The performance of these functions can be compromised by structural defects of the lips that result from trauma, infections, congenital malformations, and tumoral lesions.
Since the early nineteenth century, several techniques have been described for lower lip reconstruction. Defects that affect less than one third of the length of the lip are usually treated with primary closure. However, few methods are described for treating defects that affect more than two thirds of the lip, among which are the remnants of Karapandzic1 and Webster-Bernard2. Each procedure has its advantages and the technique of choice should consider both the size of the defect and the availability of adjacent tissue.
The Karapandzic technique was introduced in 1974 for lower lip reconstruction. It is a modification of the Gillies fan flap3, which is best indicated for the reconstruction of central defects. The advantage of the technique is that restoration of the orbicularis oris muscle is possible in a single surgery, restoring lip functionality and aesthetics. In addition, it involves the use of a neurovascular flap to maintain total lip innervation for which dissection is critical to prevent nerve severance and to preserve sensation and motor function of the reconstructed lip. Semicircular flap incisions are made to connect the inferior margin of the defect to the nasal ala and separate the orbicularis oris muscle from the other structures involved in facial mimicry, with the use of the skin, and subcutaneous and muscular tissues. However, when used for reconstruction of large defects, in particular, the Karapandzic technique has a major drawback, microstomia, albeit responsive to physical therapy and dilation.
The objective of this study was to report 2 patients who underwent reconstruction of large lesions of the lower lip, using the Karapandzic technique.
CASE REPORT
Case 1
A 24-year-old male patient was hospitalized with laceration/contusion trauma to the face sustained in a car crash, with avulsion of 80% of the lower lip, mostly to the left (Figure 1). In the initial treatment, debridement of devitalized tissue and hemostasis of the perioral region were performed, followed by suturing of associated lesions on the face. Furthermore, the patient underwent lower lip reconstruction using the Kara-pandzic technique at the Hospital Santo Amaro (Guarujá, São Paulo, Brazil; Figures 2 and 3).
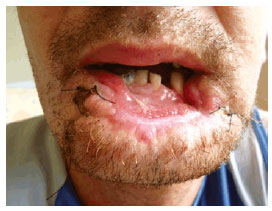
Figure 1- Case 1: Preoperative view of the patient with 80% loss of the lower lip after laceration/contusion trauma.

Figure 2 - Case 2: Aspect on postoperative day 3 with evidence of small dehiscence at the junction of the flaps.

Figure 3 - Case 1: Aspect on the postoperative day 7 indicating an unsatisfactory result.
Case 2
A 53-year-old male albino patient who was a construction worker and a social drinker with a 15 -year history of smoking, presented with lesions crusted in the middle one third of his lower lip, which progressed to bleeding, pain, and local swelling, giving rise to rapidly growing ulcerous oral lesions that had been developing for 3 months (Figure 4). Based on biopsy results, the patient was diagnosed with moderately invasive squamous cell carcinoma. At the Hospital Ana Costa (Santos, São Paulo, Brazil), the patient underwent lesion resection with surgical margins and plastic reconstruction in a single surgical procedure using the Karapandzic technique (Figures 5 to 8).

Figure 4 - Case 2: Preoperative view of the patient with squamous cell carcinoma of the lower lip.

Figure 5 - Case 2: Large lip defect after resection of the squamous cell carcinoma with surgical margin.

Figure 6 - Case 2: Patchwork preserving the neurovascular network.

Figure 7 - Case 2: Postoperative aspect after lip reconstruction.

Figure 8 - Case 2: 15 postoperative days after lip reconstruction.
Surgical Technique
The patients were placed in a supine position under general anesthesia induced via local infiltration with a lidocaine solution containing 1% adrenalin at a 1:200,000 dilution. Based on a previously described procedure of the Karapandzic technique1, marking for the right flap was performed using the nasolabial fold line as reference, obtaining a lateral flap from adjacent tissue. The same was performed for the left flap. In case 2, the squamous cell carcinoma was resected with surgical margins (Figure 5) followed by careful incision and dissection of the myocutaneous flaps. During dissection of the orbicularis muscle with the aid of delicate scissors, the arterial and venous branches (upper and lower lips) (Figure 6), as well as the nerve branches were identified and preserved. The 2 flaps were easily mobilized and advanced to the midline. Careful hemostasis was maintained via bipolar electric cautery, followed by muscle and mucosa syntheses and skin closure using simple interrupted sutures with 3-0 catgut, and 5.0 and 6.0 monofilament nylon threads, respectively. The procedure was well tolerated without adverse events during the postoperative period.
The patient in case 1 developed labial dehiscence at the junction of the flaps on postoperative day 3 and underwent an additional procedure to refine the aesthetic result (Figures 2 and 3). In contrast, the outcome in case 2 was considered good in terms of aesthetics and functionality, with neither pain from the patchwork nor bruises.
The pathological examination in case 2 revealed a 3-1.5-cm squamous cell carcinoma that was moderately differentiated (stage II) and invading the chorion at a 0.8-cm tumor-free margin. The patient was referred for outpatient treatment (Figures 7 and 8).
DISCUSSION
Lips play a role in oral competence, swallowing, articulation, and emotional expression besides aesthetics. In particular, the lower lip controls motility and acts as a leakage barrier. The main goal of lip reconstruction is to restore functionality, symmetry, and contour.
An optimal method for lip reconstruction has not yet been established4-16. In cases where the lesion affects less than one third of the lip, direct closure may be performed; otherwise, valvuloplasty is performed. When the lesion affects > 35% of the lip, graft implantation is required, with the use of the skin from adjacent areas such as the unaffected lip (Abbe type), cheek (Gillies- or Estlander- type), or chin (Bernard type).
The advantages of the Karapandzic technique include the single surgical procedure required, its quick execution once learned, and preservation of the important vascular/nerve network, ensuring safety and maintenance of lip mobility and sensation.
Semicircular flap incisions are made to connect the inferior margin of the defect to the nasal ala and separate the orbicularis muscle from the other muscles of facial expression, with the use of the skin and subcutaneous tissue. Best results are obtained when the lesion is located in the median region of the lips; however, outcomes are not as satisfactory when symmetry is affected. The main adverse effect associated with the Karapandzic technique is microstomia. In approximately 12-15% of patients, reintervention to improve microstomia using commissuroplasty is required.
Therefore, lip reconstruction using the Karapandzic technique may be considered an alternative procedure for large lesions, particularly in the lower lip, because it can be completed in a single procedure and is fast and safe to perform. In addition, the technique allows preservation of the neurovascular pedicle, providing good results from functional and aesthetic perspectives. However, its main drawback is the development of microstomia in the early stages, although this gradually improves over time.
REFERENCES
1. Karapandzic M. Reconstruction of lip defects by local arterial flaps. Br J Plast Surg. 1974;27(1):93-7.
2. Webster RC, Coffey R, Kelleber RE. Total and partial reconstruction of the lower lip with innervated muscle-bearing flaps. Plast Reconstr Surg Transplant Bull. 1960;25:360-71.
3. Gillies HD, Millard R. Principles and art of plastic surgery. Boston: Little, Brown & Co; 1957. p.507-8.
4. Jabaley ME, Orcutt TW, Clement RL. Applications of the Karapandzic principle of lip reconstruction after excision of lip cancer. Am J Surg. 1976;132(4):529-32.
5. Matos da Fonseca A, Gómez García F. Reconstrucción de labio con técnica de Karapandzic. Cir Plást Iberolatinoam. 2007;33(1):57-62.
6. Nzakamwita M, Linker M, Gitani J, Piert R. Repair of tissue loss of the lips. Acta Stomatol Belg. 1995;92(4):159-69.
7. Abulafia AJ, Edilberto L, Fernanda V. Reconstruction of the lower lip and chin with local flaps. Plast Reconstr Surg. 1996;97(4):847-9.
8. Calhoun KH. Reconstruction of small- and medium-sized defects of the lower lip. Am J Otolaryngol. 1992;13(1):16-22.
9. Kroll SS. Staged sequential flap reconstruction for large lower lip defects. Plast Reconstr Surg. 1991;88(4):620-5.
10. Jabaley ME, Clement RL, Orcutt TW. Myocutaneus flaps in lip reconstruction. Applications of the Karapandzic principle. Plast Reconstr Surg. 1977;59(5):680-8.
11. Hills RJ. Innervated musculocutaneous lip flap (Karapandzic technique). Australas J Dermatol. 1998;39(3):190-1.
12. ClairmontAA. Versatile Karapandzic lip reconstruction. Arch Otolaryngol. 1977;103(11):631-3.
13. Smith PG, Muntz HR, Thawley SE. Local myocutaneous advancement flaps. Alternatives to cross-lip and distant flaps in the reconstruction of ablative lip defects. Arch Otolaryngol. 1982;108(11):714-8.
14. Rashid M, Hanif MS, Illahi I, Aslam R, Hameed S, Masood T. Reconstruction of lip defects with the Karapandzic technique. J Coll Physicians Surg Pak. 2003;13(4):219-22.
15. Tai-Fung C, Wen-Shyan H, Shyi-Gen C, Shou-Liang C, Tim-Mo C, Hsian-Jenn W, et al. Karapandzic flap for reconstruction of large lower lip defects: a case report. J Med Sci. 2000;20(6):316-20.
16. Mélega JM. Cirurgia plástica: fundamentos e arte. Cirurgia reparadora de cabeça e pescoço. Rio de Janeiro: Medsi; 2002. p.939.
1. Plastic surgeon, associate member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery - SBCP), with specialization in plastic surgery in the Department of Plastic Surgery; Dr. Ewaldo Bolívar de Souza Pinto, Universidade Santa Cecilia (UNISANTA), Santos, SP, Brazil
2. Plastic surgeon, full member of the SBCP, preceptor of the Department of Plastic Surgery; Dr. Ewaldo Bolívar de Souza Pinto, UNISANTA, Santos, SP, Brazil
3. Plastic surgeon, full member of the SBCP, preceptor of the Plastic Surgery; Dr. Ewaldo Bolívar de Souza Pinto, UNISANTA, Santos, SP, Brazil
4. Plastic surgeon, full member of the SBCP, regent of the Department of Plastic Surgery; Dr. Ewaldo Bolívar de Souza Pinto, UNISANTA, Santos, SP, Brazil
5. Plastic surgeon, full member of the SBCP, director of the postgraduate course in plastic surgery, Universidade Santa Cecilia UNISANTA, Santos, SP, Brazil
Correspondence to:
Osvaldo Ribeiro Saldanha
Av. Washington Luiz, 142 - Vila Mathias
Santos, SP, Brazil - CEP 11050-200
E-mail: clinica@clinicasaldanha.com.br


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter