

Original Article - Year 2013 - Volume 28 -
Anatomical basis for the use of the fibularis tertius muscle in myocutaneous flaps
Bases anatômicas para utilização do músculo fibular terceiro em retalhos miocutâneos
ABSTRACT
BACKGROUND: Myocutaneous flaps have been increasingly used in surgical reconstruction of the lower limbs, requiring the use of muscles that result in less functional and esthetic damage as flaps. This study aimed to evaluate the use of the fibularis tertius muscle (in terms of frequency and anatomy) as flaps in this procedure.
METHODS: Sixty-four lower limbs from preserved cadavers were dissected and evaluated based on the following parameters: proximal insertion, distal insertion, syntopy, morphology, and morphometry.
RESULTS: The fibularis tertius muscle was detected in 96.9% of the study cases. Most proximal insertions (96.8%) were found at the interosseous membrane, anterior border of the fibula, and anterior intermuscular septum. Most distal insertions (77.4%) were found at the lateral and dorsal sides of the 5th metatarsal. Mean value of muscle belly length was 17.89 cm and width was 1.95 cm. The mean length of the distal tendon with no muscle fibers was 1.2 cm, and the mean width was 0.45 cm.
CONCLUSIONS: The fibularis tertius muscle is frequent and has a distinct morphology, making it a viable option for the repair of lower limb (distal segment) defects.
Keywords: Surgical flaps. Plastic surgery. Lower extremity.
RESUMO
INTRODUÇÃO: A utilização de retalhos miocutâneos é cada dia mais frequente nas cirurgias plásticas reconstrutoras de membros inferiores, tornando-se essencial a utilização de músculos que denotem menor prejuízo tanto funcional como estético. Foram estudados a frequência e os aspectos anatômicos do músculo fibular terceiro, com o intuito de avaliar, sob esses aspectos, a possibilidade de seu uso nesses procedimentos.
MÉTODO: Foram dissecados 64 membros inferiores de cadáveres fixados e verificadas as seguintes características: inserção proximal, inserção distal, sintopia, morfologia e morfometria.
RESULTADOS: A presença do músculo foi constatada em 96,9% dos casos, sendo analisados os aspectos supracitados. A inserção proximal mais frequente (96,8%) ocorreu na membrana interóssea, na margem anterior da fíbula, e no septo intermuscular anterior. A inserção distal mais comum (77,4%) foi nas faces dorsal e lateral do 5º metatarsiano. O valor médio do comprimento e da largura do ventre muscular foi, respectivamente, de 17,89 cm e 1,95 cm, enquanto a média do comprimento do tendão distal livre de fibras musculares foi de 1,2 cm e a largura média do tendão distal, de 0,45 cm.
CONCLUSÕES: O músculo fibular terceiro é frequente, de morfologia distinta, que, sob aspectos morfométricos, se constitui em opção viável para um estudo mais específico de seu uso no reparo de defeitos no segmento distal do membro inferior.
Palavras-chave: Retalhos cirúrgicos. Cirurgia plástica. Extremidade inferior.
Injuries of the leg and dorsal foot associated with soft tissue loss are common in emergency rooms1. Plastic surgeons use a range of surgical approaches to treat these lesions to ensure sufficient coverage and preservation of the structure, and to avoid complications and long hospital stays, especially in small or medium urban centers with a lack of skilled surgeons or the infrastructure for conducting microsurgery2. Soft tissue reconstruction of the lower limbs is particularly challenging with the small amount of subcutaneous tissue and the lack of muscle protection for the osteotendinous and neurovascular structures, so it often requires several surgical interventions using myocutaneous flaps3.
For moving tissue from the donor site to the grafting site, the following should be considered: distance between the donor site and the injured site, size of the flap available for the transplant conditions of the implant area, and presence of an adequate supply of tissue1,4-6. The ideal flap yields the best esthetic and functional results with minimal sequelae1,4.
Advantages of using myocutaneous flaps include the following: presence of various planes (skin, subcutaneous, fascia, and muscle) that provide volume, a donor site located far from the radiation field, and the reliability provided by the vascular pediculum4,5. Studies report the use of the soleus muscle1, anterior tibial muscle, gastrocnemius muscle1, and extensor digitorum muscle5,7 as flaps for the distal third of the lower limb. However, using these muscles can be detrimental to the motor function of the foot and to patient quality of life5,8,9.
In this study, the fibularis tertius muscle was investigated as an alternative source of flaps for the repair of injuries of the leg and dorsal foot. This muscle has proximal insertion at the lower half of the anterior side of the fibula and distal insertion occurs at the bottom of the 5th metatarsal10. Blood supply is provided by 1 to 3 branches of the anterior tibial artery, which irrigate the anterior section of the leg, and the deep fibular nerve provides innervation to the muscle11. The fibularis tertius muscle is an appendage of the extensor digitorum muscle, so it does not have an anatomical identity12. The negligible function of the fibularis tertius muscle means it can be used in myocutaneous flaps without compromising motor function and esthetics in the area. Thus, we analyzed the anatomy of the fibularis tertius muscle in terms of frequency, morphology, morphometry, proximal and distal insertion, and syntopy (position in relation to other muscles), and investigated the use of this muscle for reconstruction of the leg and dorsal foot.
METHODS
We received institutional approval and adhered with Brazilian Law 8501, of November 30, 1992, which rules on using non-reclaimed cadavers in scientific research and studies performed at medical schools. We dissected 64 connected and unconnected lower limbs (32 from the left side and 32 from the right side) from male and female cadavers. Cadavers, preserved in 5% formaldehyde, were of adult Brazilian subjects from the Sector of Human Anatomy, Institute of Health and Biological Sciences of the Federal University of Alagoas.
Dissections were performed using the naked eye, and incisions were made to expose the anterior section of the leg, and dorsum of the foot, while analyzing the muscles and tendons. The fibularis tertius muscle was identified in 62 of the dissected lower limbs and was analyzed for the following characteristics: proximal insertion, distal insertion, syntopy, morphology, and morphometry.
The muscle belly was evaluated both for total length and width (after calibration at the medial point of the muscle belly) - Figure 1. Three parameters were evaluated during tendon analysis: total extension, extension of the tendon section without muscle fibers, and width.

Figure 1 - Morphometric analysis of the muscle. Black dotted line = length of the tendon without fibers; red dotted line = tendon width; blue dotted line = length of the tendon with muscle fibers; yellow dotted line = muscle length; and green dotted line = muscle width.
RESULTS
Frequency
Of the 64 dissected lower limbs, the fibularis tertius muscle was found in 62 (96.9%), and could not be found in both limbs of 1 cadaver (Figures 2 and 3).
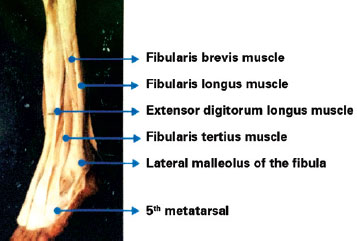
Figure 2 - Presence of the fibularis tertius muscle in the lower limb.
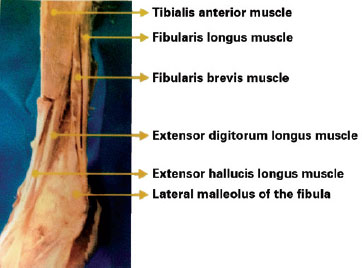
Figure 3 - Single case of absence of the fibularis tertius muscle.
Morphology
In all of the cases where it was located (62 limbs), the fibers of the fibularis tertius muscle were lying at an oblique angle to the insertion tendon in the craniocaudal direction. This muscle was characterized as unipennate with gradual broadening.
Morphometry
The mean length of the muscle belly was 17.89 cm, and the mean width was 1.95 cm. The total extension of the muscle with the tendons had a mean of 20 cm. The mean length of the distal tendon with no muscle fibers was 1.2 cm, and the mean width was 0.45 cm.
Muscle Insertion
Proximal Insertion
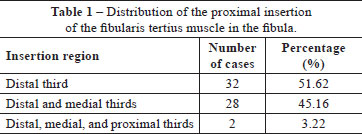
The interosseous membrane, the anterior intermuscular septum, and the anterior border of the fibula were the proximal insertion points in 60 (96.8%) of the cases (Figure 4). For proximal insertion to the anterior border of the fibula, insertion to the distal third of this muscle occurred in 32 (51.6%) cases. In only 2 (3.2%) lower limbs, the insertion occurred at the entire border of the fibula including the distal, medial, and proximal thirds (Table 1).
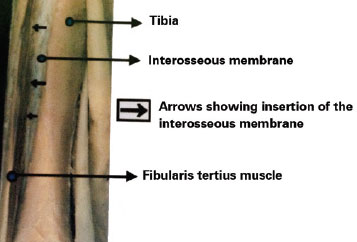
Figure 4 - Anterior view of the proximal insertion.
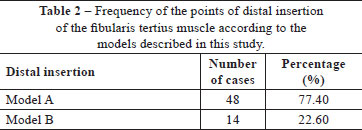
Distal Insertion
The following distal insertion patterns were detected:
model A - the tendon was inserted to the dorsal and lateralsides of the5th metatarsal in 48 (77.4%) cases; model B (Figure 5) - the tendon was inserted to the dorsal and lateral sides of the 5th metatarsal and to the dorsum of the base and proximal third of the 4th metatarsal in 14 (22.6%) cases (Table 2).
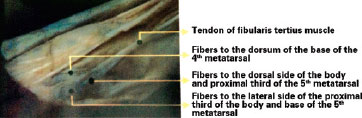
Figure 5 - Model B of distal insertion.
Syntopy
The fibularis tertius muscle was found at the most lateral and inferior sections of the anterior compartment of the leg. The superior and medial thirds of the muscle belly were posterior and lateral to the anterior border of the fibula and the anterior intermuscular septum, and continuous with the lateral compartment of the leg. The posterior medial location of the fibularis tertius muscle set it near the lateral part of the interosseous membrane, the medial side of the fibula, and the extensor digitorum and extensor hallucis longus muscles. These muscles were intimately associated and often consisted of intercrossing fibers of both muscles with the fibularis tertius muscle at the proximal insertion level.
The fibularis tertius muscle and the extensor digitorum muscle were found adjacent to one another and located such that intercrossing of fibers of these muscles were observed. However, the direction of the cluster of muscle fibers from the fibularis tertius muscle formed an acute angle with the fiber path headed for the extensor digitorum muscle.
The lower third of the muscle belly was posterior to the lateral malleolus, and medial to the tendons of the extensor digitorum and extensor hallucis longus muscles. The distal insertion tendon of the fibularis tertius muscle passed over the proximal end of the retinaculum of the extensor muscles and moved posterior over the short extensor finger muscle in the direction of the distal insertion point.
DISCUSSION
Reconstruction surgery of the distal extremities of the lower limbs is technically challenging due to the shortage of subcutaneous tissue, absence of intense vascularization, presence of bony prominences and, most importantly, the few options for generating myocutaneous flaps9.
The ideal muscle, with negligible function and minimal esthetic aspect, provides for use as a myocutaneous flap10. Moreover, our results confirmed a high frequency (96.9%) of the fibularis tertius muscle, demonstrating that these findings are statistically significant. Our results are in agreement with those from Le Double11, who reported a frequency of 91.2%, demonstrating that the presence of this muscle is almost constant.
Few studies have investigated the morphology of the fibularis tertius muscle, and it has been variably classified as long, thin12, flat13,14, shaped as a long band15, long and thin16, and strip-shaped17. This classification does not concur with our findings, as it refers to muscles displaying longitudinal fiber orientation. In our study, we found that the fibularis tertius muscle broadened towards the craniocaudal direction and displayed oblique orientation of fibers to the tendon. Fibers were inserted to one side of the tendon, defining the muscle as unipennate. This morphological classification (unipennate) was not used by any previous authors.
Muscle's fibers become increasingly flat as they approach insertion so this favors use in myocutaneous flaps, because it permits the use of greater muscle thickness in the reconstruction of complex injuries of the lower limb5.
No consensus exists in the literature for proximal insertion with no previous description of simultaneous insertion at 3 points, particularly, insertion into the anterior border of the fibula. In a few studies, proximal insertion was to the distal third of the anterior surface of the fibula, adjacent to the interosseous membrane and the anterior intermuscular septum17-18. In these cases, there was no detailed description of the point of insertion to the fibula.
Many studies report distal insertion at the dorsal side of the 5th metatarsal10,12-16,18,19. However, in this study, we found distal insertion to the base of the 4th metatarsal, even though it occurred at a lower frequency (22.58% of the cases).
The length and width of the muscle belly of the fibularis tertius muscle was compatible with use in myocutaneous flaps, even though no previous research provides similar analysis.
The syntopy analysis of the fibularis tertius muscle showed that this muscle is independent of other leg muscles found in the anterior compartment of the leg. Although intimately associated with the extensor digitorum and extensor hallucis longus muscles, they are not continuous and their fibers display a completely different orientation, diverging towards their own tendons. Thus, we disagree with the theory that the fibularis tertius is a lateral section of the extensor digitorum muscle15,17,18.
Based on the results of this study and the ease of access by longitudinal incision on the anterior-lateral side of the leg, the fibularis tertius muscle can be used to prepare lower limbs grafts.
CONCLUSIONS
The fibularis tertius muscle is frequent, which is a fundamental attribute for its potential use as a source of local flaps, and it has distinctive features, including morphometric ones, which allows for its use in reconstruction surgery of the lower limb. In most cases, this muscle is of adequate length for use in a wide variety of grafts.
REFERENCES
1. Bacelar TH. Utilização do músculo sóleo para perdas musculocutâneas de terço médio da perna. Rev Bras Cir Plást. 2011;26(2):211-20.
2. Civantos FJ, Netterville JL. Complications of myocutaneous flap surgery. In: Eisele DW, ed. Complications in head and neck surgery. St. Louis: Mosby; 1993. p. 733-42.
3. Visweswar B, Partha SB, Saurabh R, Gaurab RC, Neeraj KA, Siddhartha B, et al. Cadaveric study and clinical application of turnover fascial flap for lower-limb defects. Eur J Plast Surg. 2011;34(5):387-94.
4. Geddes CR, Morris SF, Neligan PC. Perforator flaps: evolution, classification and applications. Ann Plast Surg. 2003;50(1):90-9.
5. Mélega JM, Silvio AZ, Psillakis JM. Cirurgia plástica reparadora e estética. Rio de Janeiro: Médica e Científica; 1988.
6. Mathes SJ, Nahai F. Clinical applications for muscle and musculo-cutaneous flaps. St. Louis: Mosby; 1982.
7. Bloch RJ, Andrews JM, Chem RC, Azevedo JF, Psillakis JM, Santos IDAO. Atlas anatômico dos retalhos musculares e miocutâneos. São Paulo: Roca; 1984.
8. Hallock GG. Utility of both muscle and fascia flaps in severe lower extremity trauma. J Trauma. 2000;48(5):913-7.
9. Garcia AMC. Retalho sural reverso para reconstrução distal da perna, tornozelo, calcanhar e do pé. Rev Bras Cir Plást. 2009;24(1):96-103.
10. Moore KL. Anatomia orientada para a clínica. 3ª ed. Rio de Janeiro: Guanabara Koogan; 1994.
11. Le Double AF. Traité dês variations du systéme musculaire de l'homme. 2ª ed. Paris: Schleicher Fréres; 1897.
12. Testut L, Latarjet A. Compêndio de anatomia descritiva. 22ª ed. Barcelona: Salvate Editores; 1959.
13. Latarjet M, Liard AR. Anatomia humana. 2ª ed. São Paulo: Panamericana; 1993.
14. Lockhart RD, Hamilton GF, Fyfe FW. Anatomia humana. Rio de Janeiro: Interamericana; 1994.
15. Gardner WD, Osburn WA. Anatomia do corpo humano. 2ª ed. São Paulo: Atheneu; 1980.
16. Romanes CBE. Cunningham manual de anatomia prática. São Paulo: Atheneu; 1976.
17. Woodburne RT. Anatomia humana. 6ª ed. Rio de Janeiro: Guanabara Koogan; 1984.
18. Gray H, Goss CM. Anatomia. 29ª ed. Rio de Janeiro: Guanabara Koogan; 1977.
19. Ferner H, Staubesand J. Sobotta atlas de anatomia humana. 19ª ed. Rio de Janeiro: Guanabara Koogan; 1993.
1. M.Sc. and Ph.D. in Human Anatomy, associate professor of the Universidade Federal de Alagoas (Federal University of Alagoas), Maceió, AL, Brazil
2. M.Sc. in Human Anatomy, assistant professor of the Universidade Federal de Alagoas (Federal University of Alagoas), Maceió, AL, Brazil
3. Physician specialized in Endocrinology, Maceió, AL, Brazil
4. Medical student and Human Anatomy Tutor of the Universidade Federal de Alagoas (Federal University of Alagoas), Maceió, AL, Brazil
Correspondence to:
Anderson Gonçalves de Farias Souto
Rua Capitão Bernardino Souto, 303 - Centro
Marechal Deodoro, AL, Brazil - CEP 57160-000
E-mail: andersongfarias@hotmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: March 9, 2013
Article accepted: May 19, 2013
This study was performed at the Universidade Federal de Alagoas (Federal University of Alagoas), Alagoas, Maceió, AL, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter