

Original Article - Year 2013 - Volume 28 -
Romberg's syndrome: a series of cases
Síndrome de Romberg: uma série de casos
ABSTRACT
BACKGROUND: The Romberg's syndrome is a disease that was first described more than a century ago, and during this period had several names. It is characterized by a slow and progressive atrophy of the tissues of a hemiface, can affect all tissues and can also display neurological and ocular manifestations. The aim of this study is to report a series of patients with progressive hemifacial atrophy, addressing treatment options for each individual case.
METHODS: Was conducted a retrospective, descriptive and analytic study of the patients treated in our service, Plastic Surgery at the Hospital de Clinicas - Universidade Federal do Paraná, and the Centro de Atendimento Integral ao Fissurado Lábio Palatal (CAIF), at Curitiba, PR, Brazil.
RESULTS: Were analyzed 13 patients, 10 (76.9%) female and 3 (23.1%) male. The age of onset of symptoms ranged from 2 to 15 years. The first medical consultation with an specialist occurred at 11.7 years. The left hemiface was most commonly affected. Seven (53.8%) patients underwent surgery.
CONCLUSIONS: The Romberg's syndrome is a rare disorder, devastating to facial appearance, and it has been widely studied. Despite great advances in medicine, its etiology definition and the treatment directed to its cause is still only a wish.
Keywords: Facial hemiatrophy. Face/surgery. Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: A síndrome de Romberg é uma moléstia descrita há mais de um século e, nesse período, recebeu várias denominações. É caracterizada por lenta e progressiva atrofia dos tecidos de uma hemiface, podendo acometer todos os tecidos e apresentar, também, manifestações neurológicas e oculares. O objetivo deste estudo é relatar série de casos de pacientes com atrofia hemifacial progressiva, abordando as opções terapêuticas individualizadas para cada caso.
MÉTODO: Foi realizado estudo retrospectivo, descritivo e analítico de pacientes atendidos nos ambulatórios de Cirurgia Plástica no Hospital de Clínicas da Universidade Federal do Paraná e no Centro de Atendimento Integral ao Fissurado Lábio Palatal (CAIF), em Curitiba, PR, Brasil.
RESULTADOS: Foram analisados 13 pacientes, sendo 10 (76,9%) do sexo feminino e 3 (23,1%) do sexo masculino. A idade de início dos sintomas variou de 2 anos a 15 anos. A primeira consulta ocorreu, em média, aos 11,7 anos. A hemiface mais frequentemente afetada foi a esquerda. Sete (53,8%) pacientes foram submetidos a cirurgia.
CONCLUSÕES: A síndrome de Romberg é uma entidade rara, devastadora na aparência facial, que tem sido muito estudada. Apesar dos grandes avanços da medicina, a definição de sua etiologia e um tratamento direcionado a sua causa ainda são apenas um desejo.
Palavras-chave: Hemiatrofia facial. Face/cirurgia. Procedimentos cirúrgicos reconstrutivos.
The progressive hemifacial atrophy was first described by Parry, in 1825, and later by Romberg, in 1846, receiving different names such as: Parry-Romberg syndrome, prosopodismorfia and trofoneurose1.
It is characterized by slow and progressive atrophy of the tissues of a hemiface initially affecting soft tissue, but it can affect all tissues including bone. May also occur: cerebral involvement, the carrier may have seizures2, intracranial vascular malformations3, alterations in cranial nerves, peripheral and autonomic nervous system involvement4, as well as ocular involvement (which occurs in 10%-15% of cases)5.
Symptoms usually begin between the first and second decades of life, progresses for a few years and then become stationary6. Some authors advocate more common occurrence in females, a ratio of 3:2 men7, while others consider the same rate between genders8. The left hemiface is the most commonly affected.
Its etiology remains controversial, several theories were suggested, such as angiogenic entrapment, trauma, infection, trigeminal neuritis, among others6,9.
The treatment consists in controlling the symptoms (neurological and ocular) while the disease is active. After the atrophy stabilization, the aesthetic treatment can be started. For the treatment of facial asymmetry can be used many alternatives, including dermal, bone and fat grafts, flaps rotation as well as the use of alloplastic products.
The objective of this study is to report cases of progressive hemifacial atrophy treated in our service, Plastic Surgery at the Hospital de Clinicas - Universidade Federal do Paraná, and the Centro de Atendimento Integral ao Fissurado Lábio Palatal (CAIF), in the period 2000 to 2012.
METHODS
A retrospective, descriptive and analytic study of patients treated in the service of Plastic Surgery at the Hospital de Clinicas - Universidade Federal do Paraná, UFPR-PR and Centro de Atendimento Integral ao Fissurado Lábio Palatal (CAIF), at Curitiba, Brazil, was performed. The medical records of patients with Romberg's syndrome who were treated in these hospitals during the period 2000 to 2012 were accessed.
The data included: age of onset of symptoms, age at first examination, gender, affected hemiface, family history, other comorbidities, number, age and type of surgical procedure.
RESULTS
Were analyzed 13 patients, 10 (76.9%) female patients and 3 (23.1%) males.
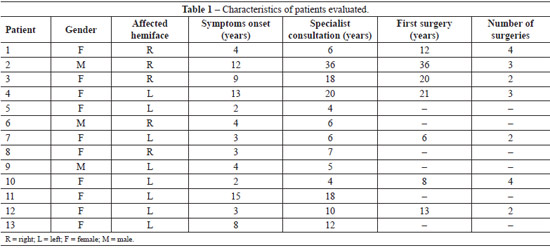
The age of onset of symptoms ranged from 2 to 15 years, with an average of 6.3 years. The first consultation with a specialist took place with 11.7 years (ranging from 4 to 36 years). The delay in seeking medical care was 5.4 years (Table 1).
The most affected hemiface was the left, corresponding to 61.5% of the total. No patient had family history of facial hemiatrophy. The associated diseases were vitiligo (n = 2), strabismus (n = 2)attention deficit disorder and hyperactivity (n = 1) and inguinal hernia (n = 1).
In our series the patients had involvement of multiple regions simultaneously, with an average of 3.6 affected regions in each case (range 2-6). The most commonly region affected was the upper lip (n = 11), followed by: cheek (n = 9), lower lip (n = 6), jaw (n = 5), nose (n = 4), forehead (n = 4 -included 3 patients with deformity coup de sabre), maxilla (n = 2), scalp alopecia (n = 2), lower eyelid (n = 1), neck (n = 1), eyebrow alopecia (n = 1) and important localized skin atrophy (n = 1). In all cases of atrophy of the cheek, the upper lip was involved, as in all cases of nasal involvement upper lip was also affected. In 5 of 6 patients with atrophy of the lower lip, jaw also was affected.
Seven (53.8%) patients underwent surgery. Were performed 2.8 procedures per patient among these patients, ranging from 2 to 4. The surgeries performed: cartilage graft for nasal region (n = 2), temporal fascia graft (n = 1), fat grafting (n = 16), cranioplasty (n = 1), piecemeal resection of scar (n = 1), rhinoplasty (n = 1), and 3 patients submitted to associate procedure.
The volume of fat grafting ranged from 5 to 55 ml per procedure, with an average of 20 ml per session. Four (57.1%) patients showed significant absorption of the fat graft, and was necessary to repeat the procedure. Three patients had good graft integration with no significant fat resorption.
Figures 1 and 2 illustrate some cases in this series.

Figure 1 - In A, patient before the beginning of aesthetic treatment. In B, patient after 3 sessions of fat grafting, with aesthetic treatment in progress.

Figure 2 - In A, patient before the beginning of aesthetic treatment. In B, patient after 4 sessions of fat grafting.
DISCUSSION
Romberg syndrome is a rare disease and its pathogenesis remains unknown. Despite multiple theories attempting to explain it, none is universally accepted. Clinical presentation is very inconstant notably in the onset of symptoms. The ectoscopy is the main element in the diagnosis of this disease. The facial hemiatrophy in our series affected predominantly female patients, as consistent with other studies7.
The initial symptoms vary: trigeminal paresthesias, seizures, hypo- or hyperchromic spots. As the disease progresses, become more apparent the alterations of skin, subcutaneous tissue and later muscle, cartilage and bone. Manifestations progress at a slow pace and tend to become stationary after some years of activity6.
The manifestation begins on the first or second decades of life6, from 2 to 15 years in our sample. The bone changes tend to be more severe as younger the patient is at the onset of symptoms10.
The long period between onset of symptoms and demand for the specialized center may be due to poor knowledge of this syndrome by physicians in general or for the delay to obtain an expert consultation in our health system.
The therapeutic approach of these children can be the use of medications or surgical. The clinical treatment of disease with immunosuppressant (methotrexate) or other medications, such as chloroquine and calcipotriol, is discussed by several authors; however, there is no scientific evidence for the use of this kind of medication11.
Surgical treatment is delayed until stabilization of the disease. The soft tissues can be treated earlier, however the correction of the osteocartilaginous structures must await the complete facial growth.
Surgical treatment of facial defect can be performed using different techniques12-15. Structural defects can receive alloplastic materials such as silicon and porous polyethylene, while soft tissue defects can be reconstructed with autologous dermal fat grafts, sequential fat grafts, and transfer of vascularized tissue (direct or microsurgical).
Mordick et al.14 and Roddi et al.15 conducted studies comparing the two main techniques: the fat grafting and vascularized tissue transfer. These studies showed that fat grafts are simple, affordable, with low risk of complications and good cosmetic results, especially for mild to moderate defects. However, for most severe atrophy, the transfer of vascularized tissue is more effective, due to the low vascular supply. Pieces of omentum, muscle and fasciocutaneous flaps, having great divergence in indications, can be used.
We used several techniques for cosmetic improvement of our patients. The indication depends primarily on the degree and location of the defect, and its indication should be individualized. The approach to the frontal region, we chose to implant a surgical cement (n = 2) and in 1 case associated with fat grafting. There were two patients who underwent conchal cartilage graft for nasal ala, one of whom later received a temporal fascia tissue to increase coverage, and erase the edges of the graft. Other procedures were piecemeal resection of scar, and rhinoplasty.
The method of choice, cause of its easy implementation and low morbidity, regardless of the result we obtained, was the fat grafting. This technique allows increase in soft tissues, corrections of other procedures that may have been insufficient, and it's easy to be repeated. The fat grafting leads to improvement in the texture of the atrophied tissue, followed by increased local blood supply.
The fat grafting technique has recently evolved in a new research on stem cells that can be isolated from lipoaspirate material in large numbers and its easily grow under standard tissue culture conditions. Because of this, there are excellent prospects for its use in plastic surgery for the treatment of congenital and acquired deformities with aesthetic or restorative purpose16.
CONCLUSIONS
Romberg syndrome is a rare disorder, devastating in facial appearance, which has been widely studied due to the potential therapeutic improvement with the use of stem cells. Despite great advances in medicine in all its fields, the etiology and treatment directed at its cause is still only a wish. While we do not have enough knowledge to treat the cause, we improve techniques for the treatment of its consequences.
REFERENCES
1. Melega JM. Cirurgia plástica: fundamentos e arte. Rio de Janeiro: Guanabara Koogan; 2004.
2. Duro LAA, Lima JMB, Reis MM, Silva CV. Atrofia hemifacial progressiva (doença de Parry-Romberg): estudo de um caso. Arq Neuropsiquiatr. 1982;40(2):193-200.
3. Miedziak AI, Stefanyszyn M, Flanagan J, Eagle RC Jr. Parry-Romberg syndrome associated with intracranial vascular malformations. Arch Ophthalmol. 1998;116(9):1235-7.
4. Brito JCF, Holanda MMA, Holanda G, Silva JAG. Hemiatrofia facial progressiva (doença de Parry-Romberg): relato de dois casos associados a trigeminalgia e câimbras. Arq Neuropsiquiatr. 1997;55(3A):472-7.
5. Muchnick RS, Aston SJ, Rees TD. Ocular manifestations and treatment of hemifacial atrophy. Am J Ophthalmol. 1979;88(5):889-97.
6. Duymaz A, Karabekmez FE, Keskin M, Tosun Z. Parry-Romberg syndrome: facial atrophy and its relationship with other regions of the body. Ann Plast Surg. 2009;63(4):457-61.
7. Boer RM. Síndrome de Parry-Romberg. Rev Bras Neurol. 1990;26(1):71-2.
8. Creus L, Sanchez-Regaña M, Salleras M, Chaussade V, Umbert P. Parry-Romberg syndrome associated with homolateral segmental vitiligo. Ann Dermatol Venereol. 1994;121(10):710-1.
9. Abele DC, Bedingfield RB, Chandler FW, Given KS. Progressive facial hemiatrophy (Parry-Romberg syndrome) and borreliosis. J Am Acad Dermatol. 1990;22(3):531-3.
10. Spraker M. Sclerosing and atrophying conditions. In: Schachner LA, Hansen RC, eds. Pediatric dermatology. New York: Churchill Livingstone; 1988. p. 925-6.
11. Alencar JCG, Andrade SHC, Pessoa SGP, Dias IS. Lipoenxertia autóloga no tratamento da atrofia hemifacial progressiva (síndrome de Parry-Romberg): relato de caso e revisão da literatura. An Bras Dermatol. 2011;86(4 Supl 1):S85-8.
12. Iñigo F, Rojo P, Ysunza A. Aesthetic treatment of Romberg's disease: experience with 35 cases. Br J Plast Surg. 1993;46(3):194-200.
13. Morais-Besteiro J, Aki FE, Mendes JA, Ferreira MC. Microsurgical transplants for facial depressions. Rev Hosp Clin Fac Med Sao Paulo. 1992;47(6):271-5.
14. Mordick TG 2nd, Larossa D, Whitaker L. Soft-tissue reconstruction of the face: a comparison of dermal-fat grafting and vascularized tissue transfer. Ann Plast Surg. 1992;29(5):390-6.
15. Roddi R, Riggio E, Gilbert PM, Hovius SE, Vaandrager JM, van der Meulen JC. Clinical evaluation of techniques used in the surgical treatment of progressive hemifacial atrophy. J Craniomaxillofac Surg. 1994;22(1):23-32.
16. Gomes RS. Perspectivas do uso de células-tronco em Cirurgia Plástica. Rev Bras Cir Plást. 2011;26(1):151-9.
1. Resident physician, Department of Plastic and Reconstructive Surgery, Hospital de Clínicas da Universidade Federal do Paraná (Federal University of Paraná - UFPR), Curitiba, PR, Brazil
2. Specialization in the Service of the Hospital of Plastic and Reconstructive Surgery at UFPR, Curitiba, PR, Brazil
3. Plastic surgeon at Service of the Hospital of Plastic and Reconstructive Surgery at UFPR, Curitiba, PR, Brazil
4. Plastic surgeon, doctor, head of the Department and associate professor of the Department of Plastic Surgery UFPR, craniomaxillofacial surgeon at Centro de Atendimento Integral ao Fissurado Lábio Palatal (Comprehensive Care Center of Cleft Lip and Palate), Curitiba, PR, Brazil
Correspondence to:
Renato da Silva Freitas
Rua General Carneiro, 180- 9º andar
Curitiba, PR, Brazil - CEP 80060-900
E-mail: dr.renato.freitas@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: January 30, 2012
Article accepted: May 16, 2012
This study was performed at the Hospital de Clínicas da Universidade Federal do Paraná, Curitiba, PR, Brasil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter