

Case Report - Year 2013 - Volume 28 -
Correction of sagging skin in the gluteal and lumbar regions using a fasciocutaneous local flap
Correção de flacidez de pele nas regiões glútea e lombar com retalho fasciocutâneo local em cambalhota
ABSTRACT
A major problem for patients after bariatric surgery is the excess skin in the gluteal and lumbar regions. In addition, there is a lack of available tissue to fill the gluteal region, which can be overcome by various methods, including fat grafting or even prosthesis implantation alone, in cases where no ptosis is noted. However, if this is not the case, the options become very limited and those available are not very effective. The use of a buttock lift with a fasciocutaneous flap solves the problems of sagging and excess skin with ptosis. In the present article, we aimed to demonstrate the ease of preparation and the versatility of use of the gluteal flap to correct sagging of the lumbar and gluteal regions. One patient underwent a buttock lift using a de-epidermized fasciocutaneous flap to overcome the lack of local filling. Marked improvement of the gluteal and lumbar regions was noted after removal of the excess tissue, construction of an inferior fasciocutaneous flap, and use of skin traction. In addition, rotation of the flap and its attachment to the gluteal muscle markedly improved the patient's posterior contour and postoperative comfort. With minimal morbidity, excess skin was removed and the gluteal region was concomitantly increased using an autologous flap that is neglected in many techniques; this resulted in an improved contour and a discreet scar that could be hidden by the patient's underwear.
Keywords: Buttocks/surgery. Bariatric surgery. Surgical flaps.
RESUMO
Um dos maiores problemas dos pacientes pós-cirurgia bariátrica é o excedente de pele nas regiões glútea e lombar. Somado a isso, há escassez de tecido para preencher a região glútea, que pode ser corrigida por vários métodos, entre eles a lipoenxertia ou, ainda, o implante de prótese isoladamente, nos casos em que não haja ptose. Se o contrário ocorre, essas opções tornam-se muito limitadas e pouco expressivas. O lifting glúteo com emprego de retalho fasciocutâneo em cambalhota permite resolver tanto a flacidez como o excesso de pele com ptose. Este trabalho tem por objetivo demonstrar a facilidade de confecção e a versatilidade de utilização do retalho glúteo em cambalhota para correção de flacidez das regiões glútea e lombar. Uma paciente foi submetida ao procedimento cirúrgico de lifting glúteo associado ao emprego de retalho fasciocutâneo desepidermizado em cambalhota, para correção de falta de preenchimento local. Melhora acentuada das regiões glútea e lombar foi obtida após a retirada do excesso de tecido superior, confecção de um retalho fasciocutâneo de pedículo inferior e tração da pele. Além disso, a rotação do retalho e sua fixação ao músculo glúteo melhoraram acentuadamente o contorno posterior da paciente, com pós-operatório bastante cômodo. Com morbidade mínima, foi retirado o excesso cutâneo e, concomitantemente, aumentada a região glútea com retalho autólogo, que é desprezado durante a execução de muitas técnicas, melhorando o contorno da paciente e deixando uma cicatriz discreta, que poderá ser ocultada pelas roupas íntimas.
Palavras-chave: Nádegas/cirurgia. Cirurgia bariátrica. Retalhos cirúrgicos.
Since the increase in stomach reduction surgeries and obesity control, plastic surgeons have been facing a growing demand from patients who have experienced a severe loss of body contouring. Further, such patients lack tissue nutrition and display a loss of skin tone and its fundamental substances. In such patients, elasticity is highly compromised, and it is not restored after bariatric surgery, but instead worsens with increased weight loss1.
In 1899, Kelly2 performed the resection of adipose tissue, which was considered at that time as an "insane" act. One can imagine the reaction of Kelly's co-workers when he resected a 7.450 g section of tissue. Subsequently, Babcock3 used a vertical incision resection, which was a technique that was used for a long time. Except for the positioning and shape of the incision, the surgery was still restricted to a simple dermolipectomy4.
The first navel preservation in abdominoplasty was performed in 1924 by Thorek5. Passot6 proposed a modification to Kelly's technique, which involved undermining of the tissue depending on the plane. In 1957, Vernon7 combined detachment along a plane with transposition of the umbilicus, which is a procedure currently used in miniabdominoplasties8. Callia9 introduced an innovative method that consisted of placing sutures in the aponeurosis, thereby correcting the associated diastasis.
Pitanguy10 published a series of abdominoplasty cases that drew the attention from many surgeons. Some years later, Regnault11 introduced a modified version of the Pitanguy technique9; in this modified technique, a "W"-shaped incision was made, similar to the shape of a bikini that could be hidden by the patient's underwear. Later, Grazer & Goldwyn12 verified that the abdominoplasty only slightly decreased the anterior projection. In 1978, Psillakis13, making use of this observation, noted that aponeurotic sutures were underutilized in such techniques. One of the most important aspects came with the advent of belt abdominoplasty or belt lipectomy, which was proposed by Somalo14 and Gonzalez-Ulloa15. This was a major milestone in post-obesity surgeries worldwide.
As for the lower limbs, Kelly16 and Noel17 highlighted the impact that thigh tissue excisions together with abdominoplasty had. In 1957, Lewis18 introduced the concept of the thigh lift. All previous resections were performed elliptically. In 1964, Pitanguy19 treated trochanteric lipodystrophy using local resection. However, this procedure was not well accepted due to unsightly and very apparent scarring. Several authors have proposed variations of this technique, including a 360° resection proposed by Regnault et al.20, which led to the development of circular reduction of the thighs. However, gluteal depression was one of the unacceptable outcomes of this technique. Agris21 and Aston22 solved this problem with the use of flap-shaped denuded skin. Lockwood23,24 revolutionized the field when he proposed the use of the superficial fascia to anchor tissues after excisional lifting.
However, a problem still remained - the significant and visible lack of tissue in the gluteal region. With the lifting of the thighs and the posterior region, the gluteal area became rectified without an appropriate shape. The use of silicone implants and fat grafting were valid attempts to rectify this problem. It should be emphasized that none of these methods has diminished value, but why not use tissue that would normally be discarded? This led to the development of local flaps that fill and give a more pleasing look to the gluteus in cases where they are de-epithelized and properly deployed. Sozer et al.25 contributed to the standardized use of the dermal fat flap to correct ptosis and the lack of tissue in the gluteal region in patients after massive weight loss.
In the present study, we aimed to report the case of a patient who underwent correction of sagging in the gluteal and lumbar region using a de-epidermized fasciocutaneous dermal flap.
CASE REPORT
A patient who presented with a history of gastroplasty and subsequent abdominoplasty, underwent a gluteal lift using a gluteal flap that was rotated 180° in the superficial gluteal fascia and on the muscle itself.
The criteria for the surgery were: massive weight loss after bariatric surgery, excess skin in the dorsal region, concomitant gluteal ptosis, and the patient's desire to correct sagging and excess skin.
Operative Technique
Preoperative photos were taken with the patient in a standing position (Figure 1). The patient was asked to bow in order to allow the evaluation of excess tissue in the lumbar region (Figure 2). We then proceeded to make preoperative markings (Figure 3).
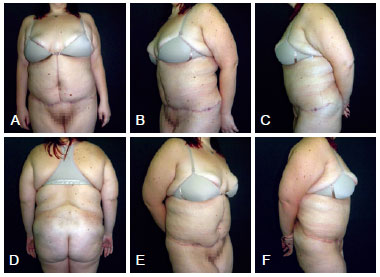
Figure 1 - Preoperative view. In A, anterior view. In B, left oblique view. In C, left side view. In D, posterior view. In E, right oblique view. In F, right lateral view.

Figure 2 - Preoperative view. Patient in flexion, left side view.

Figure 3 - Details of the preoperative markings.
The patient was placed in the prone position after anesthesia induction. General anesthesia was chosen because, although the surgical period was not very long, the patient would be in a position where there would be some breathing restriction. After asepsis and establishment of the surgical field, the previously made markings were reinforced. It is important to note that any error in this markup is impossible to be recognized with the patient lying down. We proceeded to mark the areas using bright green marker. The points marked were equally distant from the midline of the body to allow for accurate positioning of the flaps and the homogeneous removal of excess tissue.
The gluteal dermal fat flap was de-epidermized similarly to pedicles in mammoplasty (Figure 4) and incised perpendicular to the upper, lateral, and medial markings up to the fascia. The lower incision was made angled from the skin to bevel up to the level of the gluteal fascia. A compartment was then created to which the flap was subsequently fixed; this was created by suprafascial detachment to the edge of the inferior gluteal fold. The next, and more delicate step, consisted of detachment, inferior 180° rotation, and attachment of the flap to the fascia of the gluteal muscle (Figure 5). The detachment was conducted progressively so that the flap was rotated without tension.

Figure 4 - Flap executed and released for fixation.
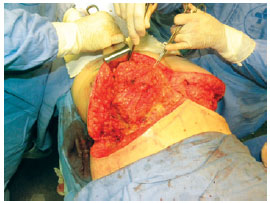
Figure 5 - Flap being fixed to the aponeurosis after being rotated 180°.
The flap was fixed with nonabsorbable monofilament nylon 2.0 stitches. This attachment was made more firmly than a breast pedicle would usually be attached, due to the movement and traction that the area requires.
The two upper and lower flaps were then stretched and anchored to the fascia on the line corresponding to the position of the final scar. The marks made previously served as a guide for the repair points. The sutures were performed with nonabsorbent monofilament nylon 3.0 in at least three places in depth, using 4.0 vicryl on the dermis (separate stitches) and 4.0 monofilament nylon, with Greek bar sutures in an effort to achieve better coaptation of the wound edges. The resulting scar looked very good, and a gluteal projection that did not exist previously as well as patient contour were achieved (Figure 6).

Figure 6 - Appearance at the end of surgery.
A large caliber suction drain was used and maintained for 5 days due to the large amount of fluid that had accumulated in flaps. The drain outlet was positioned in the inferior gluteal fold, which in turn was positioned bordering the flap on the muscles to the region close to the scar of the suture (Figure 7). No compressive dressings were implemented in the immediate postoperative period. The patient was advised not to lie down on the buttocks for at least 2 weeks.

Figure 7 - Final appearance with a suction drain already positioned.
The result was considered satisfactory since the desired contour and gluteal projection were obtained (Figures 8 and 9). The resulting scars had good quality and no complications such as dehiscence were observed. The drains were removed 5 days after the operation and demonstrated only slight sero-hematic secretion. A small amount of seroma (20 mL) was subsequently observed and then drained on the 14th postoperative day.

Figure 8 - Postoperative appearance showing contour and gluteal projection.
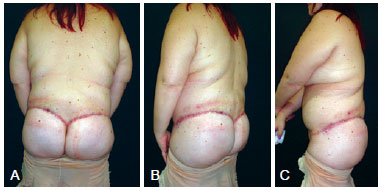
Figure 9 - Aspect 2 months postoperatively. In A, posterior view. In B, left oblique view. In C, left side view.
The duration of surgery was 3 hours, including drain insertion and fixing, creation of the final suture, and placement of the modeling belt.
There were no areas of necrosis, pain, or bruising. The patient presented with a small ecchymosis that was resolved normally in the course of the clinical consultations. The sensitivity of the area did not change and the patient reported improved quality of life.
DISCUSSION
With the increasing number of patients seeking the removal of excess skin after bariatric surgery, the development of techniques in the plastic surgeon's armamentarium is essential. The contour of the gluteus is considerably improved with the use of fat grafts, with or without centrifugation, as well as prostheses. However, it is much more sensible and rational to first use tissues that would normally be discarded during gluteal lift surgery. The feasibility of this procedure is high and necrosis is almost negligible. Moreover, blood loss is not high and, since the operative time is relatively short, morbidity is low. However, additional procedures may be required in cases where the gluteal projection obtained with the operation is deemed unsatisfactory. The resulting scar is of good quality and can be hidden under clothing. Although large, it is well accepted by the patient in the present case, who recovered her self-esteem.
There are slight differences in the preoperative marking process of female and male patients. In females, after performing the pinch test of excess tissue to be removed, the lower incision line is positioned slightly below the natural circumference of the buttocks, always arched, with the concavity facing downward (Figure 2). The reason for this is that if the incision is placed in the lower limit of the superior sulcus gluteus, the scar will end at the waistline, leaving the woman with a more "square" body. In men, this line is rectified to a greater extent, on the edge of the groove, so as not to leave them with a small waist.
Some considerations should be made as to the details of the markings. We must remember the symmetry with the patient standing and visualize the final scar position. The topmost line must be checked first. This same line, at the end of the procedure, will be lowered from its original position by 1 or 2 cm due to traction of the tissues. This line is drawn in a direction moving out of the intergluteal sulcus and proceeding in an arched form to the posterior iliac spine. The same procedure is performed on the contralateral side, resulting in a "V" labeling pattern. The bottom line is selected using the pinch test to estimate the amount of tissue to be resected. This line appears to be straighter than the top line.
The dermal fat flap is then drawn on the inside of the tissue that is to be resected. Its dimensions vary from patient to patient as well as from the amount of projection expected at the end of the procedure. The internal marking of this flap is 2-3 cm from the midline of the body, which - in the posterior region - passes through the apex of the "V" marked above. The external marking of the flap accounts for approximately three quarters of the distance from the posterior midline to the posterior axillary line.
The gluteal dermal fat flap is a randomized flap based on perforating vessels of the superior gluteal artery, while the cover flaps are based on 20 to 25 perforating vessels of the superior and inferior gluteal arteries, both of which are branches of the internal iliac artery. In addition, concomitant liposuction of the flanks and areas adjacent to the flap can be performed.
Unlike mammoplasty, in gluteoplasty with a flap, compressive dressings are not employed in the immediate postoperative period, since the flap is more delicate and cannot withstand immediate compression. The stitches are removed as late as possible because of tissue traction, usually after 21 days.
There are several options of gluteal flaps for achieving the same purpose. Our choice was based on the large vascularity of the flap, its relatively lower tension when set, the small torsion of the nourishing pedicles, and the work by Sozer et al.25.
Within the logical sequence of surgeries that ex-obese individuals are subjected to, the gluteal flap associated with lifting provides correction of various changes in a single surgical period, with low morbidity and short hospital stay, provided that all parameters of the described technique are observed and followed. There is no logical justification for the use of prostheses or fat grafting before correcting ptosis with a flap except for the lack of technical knowledge, which may very well be remedied. There is no waste of tissues and, indeed, they are almost completely reused.
The learning curve of this technique is relatively short if the plastic surgeon already has expertise in surgery after massive weight loss, and the use of this procedure in this group of patients should be encouraged.
One can correct several problems with the use of gluteal lifting associated with de-epidermized fasciocutaneous flap, such as ptosis, sagging, and excess tissue in the posterior region, as well as increasing the buttock volume with a single surgical procedure. Fat grafts or local prostheses can be used in a second procedure as needed.
REFERENCES
1. American Society of Bariatric Surgeons. Rationale for surgery. Disponível em: http://www.asbs.org. Acesso em: 8/12/2009.
2. Kelly HA. Report of gynecological cases (excessive growth of fat). Johns Hopkins Med J. 1899;10:197-201.
3. Babcock W. The correction of the obese and relaxed abdominal wall with special reference to the use of the buried silver chain. Am J Obst. 1916;1:596-611.
4. Regnault P, Daniel R. Aesthetic plastic surgery: abdominoplasty. Boston: Little Brown; 1984. p.618.
5. Thorek M. Plastic reconstruction of the female breast and abdomen wall. Springfield: Thomas; 1924.
6. Passot R. Abdominoplasty. In: Chirurgie Esthetique Pure. Paris: Doin; 1931. p.260-7.
7. Vernon S. Umbilical transplantation upward and abdominal contouring in lipectomy. Am J Surg. 1957;94(3):490-2.
8. Grazer FM. Abdominoplasty. Plast Reconstr Surg. 1973;51(6):617-23.
9. Callia WEP. Contribuição para o estudo da correção cirúrgica do abdome pêndulo e globoso: técnica original [Tese de doutorado]. São Paulo: Faculdade de Medicina da Universidade de São Paulo; 1965.
10. Pitanguy I. Abdominal lipectomy: an approach to it through an analysis of 300 cases. Plast Reconstr Surg. 1967;40(4):384-91.
11. Regnault P. Abdominoplasty by the W technique. Plast Reconstr Surg. 1975;55(3):265-74.
12. Grazer FM, Goldwyn RM. Abdominoplasty assessed by survey, with emphasis on complications. Plast Reconstr Surg. 1977;59(4):513-7.
13. Psillakis JM. Abdominoplasty: some ideas to improve results. Aesthetic Plast Surg. 1978;2:205-15.
14. Somalo M. Dermolipectomia circular del trunco. Cir Clin Exper. 1942;6:540-3.
15. Gonzalez-Ulloa M. Circular lipectomy with transposition of the umbilicus and aponeurolytic plastic technic. Cir Cir. 1959;27:394-409.
16. Kelly HA. Excision of the fat of the abdominal wall lipectomy. Surg Gynecol Obstet. 1910;10:229-31.
17. Noel A. La cirurgie esthetique: son role social. Paris: Mason; 1926.
18. Lewis Jr JR. The thigh lift. J Int Coll Surg. 1957;27(3):330-4.
19. Pitanguy I. Trochanteric lipodystrophy. Plast Reconstr Surg. 1964;34:280-6.
20. Regnault P, Baroudi R, Carvalho C. Correction of lower limb lipodystrophy. Aesthet Plast Surg. 1979;3:233-49.
21. Agris J. Use of dermal-fat suspension flaps for thigh and buttock lifts. Plast Reconstr Surg. 1977;59(6):817-22.
22. Aston SJ. Buttocks and thigh. In: Regnault P, ed. Aesthetic plastic surgery. Philadelphia: WB Saunders; 1980. p.1038-9.
23. Lockwood TE. Superficial fascial system (SFS) of the trunk and extremities: a new concept. Plast Reconstr Surg. 1991;87(6):1009-18.
24. Lockwood T. Lower body lift with superficial fascial system suspension. Plast Reconstr Surg. 1993;92(6):1112-25.
25. Sozer SO, Agullo FJ, Palladino H. Autologous augmentation gluteoplasty with a dermal fat flap. Aesthet Surg J. 2008;28(1):70-6.
1. Specialist member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery - SBCP), full member of the Colégio Brasileiro de Cirurgiões (Brazilian College of Surgeons), member of the Sociedade Latino-Americana de Queimaduras e Sociedade Brasileira de Queimaduras (Latin American Society of Burns and the Brazilian Society of Burns), resident of the Plastic Surgery Service, Hospital da Lagoa, Rio de Janeiro, RJ, Brazil; plastic surgeon, Hospital Clementino Moura, Clínica São José, Clínica Silhouette and Hospital São Domingos, São Luís, MA, Brazil
2. Full member of the SBCP, full member and founder of the Sociedade Brasileira de Cirurgia Craniomaxilofacial (Brazilian Society of Craniomaxillofacial Surgery), former chief of Plastic Surgery, Hospital da Lagoa, Rio de Janeiro, RJ, Brazil; Head of the Department of Craniofacial Plastic Surgery, Hospital São Vicente de Paulo, Rio de Janeiro, RJ, Brazil
3. Specialist member of the SBCP, plastic surgeon at the Hospital da Lagoa, Rio de Janeiro, RJ, Brazil
Correspondence to:
Guilherme Mendes Monteiro
Rua L - Quadra 17 - Casa 12 - Parque Athenas
São Luís, MA, Brazil - CEP 65072-510
E-mail: drguilhermemonteiro@hotmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: August 4, 2010
Article accepted: February 22, 2011
This study was performed at the Hospital Federal da Lagoa, Rio de Janeiro, RJ, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter