

Original Article - Year 2013 - Volume 28 -
Alar cartilage deformity correction using conchal cartilage in patients with unilateral cleft lip-nose
Correção da deformidade da cartilagem alar com cartilagem conchal em pacientes fissurados unilaterais
ABSTRACT
BACKGROUND: Rhinoplasty in patients with cleft lip and palate is a challenging surgery to the plastic surgeon because it involves the correction of multiple factors associated with an altered anatomy.
METHODS: A retrospective analysis of 15 patients that were submitted to surgery performed by the author, between February 2009 and January 2012, was performed. Investigated parameters included age, gender, and type of cleft.
RESULTS: All patients were subjected to open rhinoplasty using a "folded" conchal cartilage for alar cartilage deformity correction on the cleft side, with satisfactory results. Necrosis of the columella, which healed by secondary intention, was reported in a single case (6.7%).
CONCLUSIONS: The "folded" conchal cartilage graft is a good option for correcting alar cartilage deformities in patients with cleft lip or unilateral clef lip and palate.
Keywords: Rhinoplasty. Nose/surgery. Cleft lip.
RESUMO
INTRODUÇÃO: A rinoplastia do paciente com fissura labiopalatal é uma cirurgia desafiadora, por envolver a correção de múltiplos fatores de uma anatomia alterada.
MÉTODO: Foi realizada análise retrospectiva de 15 pacientes operados pelo autor, no período de fevereiro de 2009 a janeiro de 2012. Foram analisados parâmetros como idade, gênero e tipo de fissura.
RESULTADOS: Todos os pacientes foram operados com a técnica de rinoplastia aberta utilizando-se cartilagem conchal "dobrada" para correção da deformidade da cartilagem alar do lado da fissura, com resultados satisfatórios. Houve 1 (6,7%) caso de necrose do retalho columelar, que cicatrizou por segunda intenção.
CONCLUSÕES: O enxerto de cartilagem conchal "dobrada" é uma boa opção de enxerto no tratamento da deformidade da cartilagem alar afetada do paciente com fissura labial ou labiopalatal unilateral.
Palavras-chave: Rinoplastia. Nariz/cirurgia. Fenda labial.
The rhinoplasty in patients with cleft lip and palate is a challenging surgery procedure for the plastic surgeon because it involves correcting multiple factors associated with this deformity. The altered anatomy of the cleft nose is complex and its surgical approach should aim at achieving a balance between function and aesthetics. The first cleft nose deformity was described by Blair & Brown, in 19311.
The etiopathogenesis of unilateral cleft nose is not well understood. Traditionally, correction of this nasal deformity was only approached during adolescence; however, the current trend is to correct the cleft nose during cheiloplasty. It still remains unknown whether the scars resulting from a primary rhinocheiloplasty will hinder the future procedure, besides not eliminating it.
There are several alterations associated with cleft nose, including:
Several techniques are used for secondary correction of cleft nose deformities using sutures that augment the hypoplastic cartilage on the cleft side2-4, but the long-term results are not satisfactory. An alternative approach involves using multiple tip and alar cartilage grafts with better long term results. Gelbke5 proposed the use of autologous grafts in 1956. The use of autogenous cartilage grafts have also been described by Musgrave6, Straith et al.7 and Millard8-10.Collapse and lateral displacement of the alar cartilage; Increase in the volume of the nasal vestibule on the cleft side; The short columella is deviated towards the cleft; Wide nasal base; Oblique tip-defining points; Asymmetry alar-columellar; Short nasal tip projection; Obtuse nasal-labial angle; Short nose; Asymmetric nostrils; Nasal septum deviation towards non-cleft side; Abnormal hair implant; Smooth angulation of the alar cartilage's intermediate crura on the cleft side.
There are several important anatomic deformities associated with cleft nose that have to be treated. These alterations vary with the degree of anatomical deformity of the cleft and is why several techniques exist to correct unilateral cleft nose. A unique well-established system to classify the cleft nose deformity does not exist. In Brazil, the Spina system is mostly used for the classification of cleft lip and palate11. The major drawback of the Spina system is that it does not consider the extent of the cleft in its cross-sectional orientation (only in its anterior-posterior orientation).
Corrections of the nasal tip and deviated septum are among the main objectives of rhinoplasty in patients with cleft nose.
The purpose of the present study was to use the conchal cartilage as an option in the treatment of alar cartilage deformities in patients with unilateral cleft nose.
METHODS
A retrospective cross-sectional analysis of patients whom the author performed surgery on between February 2009 and January 2012 was performed.
The parameters analyzed included gender, age and type of cleft, according to the Spina classification. All patients with unilateral cleft lip or clef lip and palate were included. Patients under 15 years of age were excluded. The author operated on all patients using the same surgical technique to reconstruct the affected alar cartilage.
Surgical Technique
The patient was placed in horizontal dorsal decubitus position, under general anesthesia. The surgical field was set up following asepsis and antisepsis.
The surgeries were performed after a local anesthetic composed of 1% xylocaine and 1% adrenaline (1:120,000) was administered by infiltration. The surgical technique involved an open rhinoplasty using a V-shaped columellar incision. Following incision, the alar cartilages were carefully exposed, the nasal dorsum was detached, and the caudal septum was exposed. Extra mucosal septoplasty was performed to correct the septum deviation and cartilage was obtained at the same time to be used in the columellar strut graft (Figure 1). The caudal septum was detached from the anterior nasal spine and re-oriented to its normal position using a 3.0 mm nylon thread.
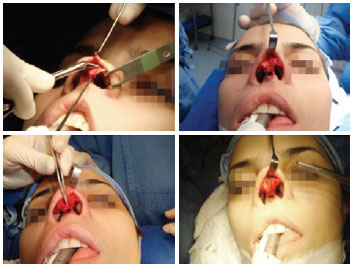
Figure 1 - Open Rhinoplasty showing asymmetry of the alar cartilages and columellar strut
The alar cartilage on the cleft side was dissected and the "folded" graft taken from the auricular concha was placed over the domus and fixed with "U" shaped sutures using a 5.0 mm nylon thread (Figure 1). The conchal grafts were sculpted with a scalpel on a metal plate. The conchal graft was obtained using an anterior incision (Figure 2). Grafts placed on the nasal tip, nasal floor and nasal dorsum were positioned as needed for each individual case. A septal cartilage strut was fixed between the medial crus of the alar cartilage using 5.0 mm nylon thread (Figures 3 and 4). After placement of the strut, nasal asymmetry was evaluated and, when necessary, resection of the skin zone in fuse of the nasal floor was performed and the cartilage graft was positioned through the same incision.
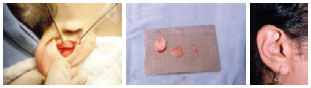
Figure 2 - Conchal cartilage graft. Graft is taken from auricular concha and scar appearance one year after the procedure.

Figure 3 - Intra-operatory view of the extra mucosal septoplasty

Figure 4 - Final placement of the "folded" conchal cartilage graft.
The columellar incision was closed in a V-Y advancement fashion using 6.0 mm nylon thread for stretching of the columella (Figure 5).

Figure 5 - Patient subjected to V-Y columellar advancement. A and C, pre-operative appearance shown from left profile and from nasal base, respectively. B and D, immediate post-operative appearance shown from left profile and from nasal base, respectively.
RESULTS
Fifteen patients were subjected to plastic surgery using the technique described above; 7 were men (46.7%) and 8 (53.3%) were women. The mean age was 23.7 years-old. Post-operative follow up periods ranged from 6 to 18 months.
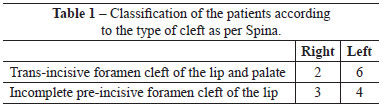
Most of the clefts were on the left side. Table 1 shows the characterization of the patients according to the Spina system. The rhinoplasty was primary in the majority of the patients (86.6%).
Necrosis of the columella, which healed by secondary intention with the use of collagenase and daily dressing changes, was reported in a single case (6.7%) (Figure 6).

Figure 6 - Complication. Necrosis of the columella graft.
Healing of the conchal and columellar scars progressed well (Figure 5). Fracture was required for only 3 (20%) patients.
Figures 7 to 14 illustrate some of the cases included in this study.
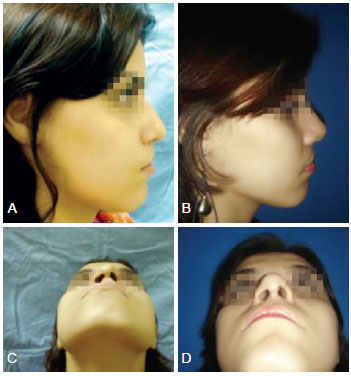
Figure 7 - Patient subjected to alar cartilage deformity correction using conchal cartilage. A and C, pre-operative appearance shown from right profile (cleft side) and from nasal base, respectively. B and D, post-operative appearance shown from right profile and from nasal base, respectively, one year after the surgery.

Figure 8 - Patient subjected to alar cartilage deformity correction using conchal cartilage. A and C, pre-operative appearance shown from left profile and from nasal base, respectively. B and D, post-operative appearance shown from left profile and from nasal base, respectively.

Figure 9 - Patient subjected to alar cartilage deformity correction using conchal cartilage. A, B and C, pre-operative appearance: anterior view (A), oblique left side view (B), and view from nasal base (C); D, E and F, post-operative appearance: anterior view (D), oblique left side view (E), and view from nasal base (F).

Figure 10 - Patient subjected to alar cartilage deformity correction using conchal cartilage. A and B, pre-operative appearance shown from nasal base and from left profile, respectively. C and D, post-operative appearance shown from nasal base and from left profile, respectively.

Figure 11 - Patient subjected to alar cartilage deformity correction using conchal cartilage. A, pre-operative appearance shown from left profile. B, post-operative appearance shown from left profile.

Figure 12 - Patient subjected to alar cartilage deformity correction using conchal cartilage. A and B, pre-operative appearance shown from left profile and from nasal base, respectively. C and D, post-operative appearance shown from left profile and from nasal base, respectively.

Figure 13 - Patient subjected to alar cartilage deformity correction using conchal cartilage. A and B, pre-operative appearance shown from right profile and from nasal base, respectively. C and D, post-operative appearance shown from right profile and from nasal base, respectively.
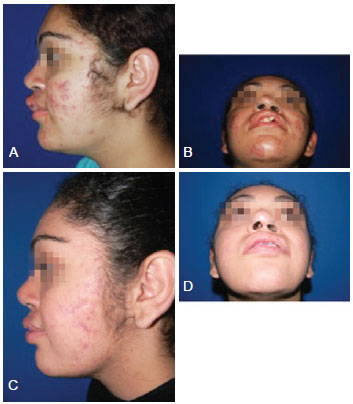
Figure 14 - Patient subjected to alar cartilage deformity correction using conchal cartilage. A and B, pre-operative appearance shown from left profile and from nasal base, respectively. C and D, post-operative appearance shown from left profile and from nasal base, respectively.
DISCUSSION
Unlike cheiloplasty and palatoplasty, secondary rhinoplasty in patients with unilateral cleft was never in the forefront of scientific publications due to the lack of encouraging results and the fact that the surgery could be delayed until patient complaints emerged. There is no consensus as to the ideal moment to perform surgery on a patient with cleft nose. Several authors including McComb3 and Skoog12, advocate that primary rhinocheiloplasty should be performed to attain less nasal deformity in the future. Other authors such as Rees et al.13 and Broadbent & Woolf14 believe that this would only lead to the formation of nose scars, which would be more difficult to treat during adult years.
Currently, the use of cartilage grafts is essential to obtain better short- and long-term results15. In the case of the patient with cleft nose, this is even more important because the alar cartilage is collapsed and the skin has no support. There is consensus that open rhinoplasty is the best approach to treat patients with cleft nose since there is more exposure of the structures under treatment and the grafts can be more easily fixed.
The objective of the surgical technique used in this study was to reconstruct the projection of the alar cartilage on the cleft side by using the conchal cartilage. One question that could be posed is: wouldn't the septal cartilage provide a better support? Surgeons often have to deal with patients who already had previous nose surgery, and as such, have no septal cartilage. Also, it would be unacceptable to create a scar in the patient's thorax just to collect some costal cartilage. The technique presented in this study, where the conchal cartilage is positioned in a "folded" fashion, provides a viable solu-tion to solve this problem. In this way, the conchal cartilage becomes stretched, changing its biomechanics and providing the needed support for the projection of the nasal tip. The columellar strut used in all rhinoplasties was useful not only for supporting the conchal graft but also to improve the projection of the nasal tip. Blackwell et al.16, in 1985, used a similar technique to perform rhinoplasty of the "bucket handle" type in 16 patients, and obtained excellent results. The reconstruction of the alar cartilage using conchal cartilage is also very common in aesthetic rhinoplasty17.
Our long-term results were satisfactory, with maintenance of the nasal tip projection and of the nose shape provided by the alar cartilage on the cleft side. It is important to note, however, that the deformity can never be fully corrected and that the stigma was improved but not fully eliminated.
CONCLUSIONS
The use of conchal cartilage graft is a good option for correcting alar cartilage deformities in patients with unilateral cleft.
REFERENCES
1. Blair VP, Brown JB. Nasal abnormalities, fancied and real surgery. Gynecol Obstet. 1931;53:797.
2. McComb H. Treatment of the unilateral cleft lip nose. Plast Reconstr Surg. 1975;55(5):596-601.
3. McComb H. Primary correction of unilateral cleft lip nasal deformity: a 10-year review. Plast Reconstr Surg. 1985;75(6):791-9.
4. Cutting CB. Secondary cleft lip nasal reconstruction: state-of the art. Cleft Palate Craniofac J. 2000;37(6):538-41.
5. Gelbke H. The nostril problem in unilateral harelips and its surgical management. Plast Reconstr Surg. 1956;18(1):65-75.
6. Musgrave R. Discussion to primary correction of unilateral cleft lip nasal deformity: a 10 year review. Plast Reconstr Surg. 1985;75:798-9.
7. Straith CL, Straith RE, Lawson JM. Reconstruction of the hairlip nose. Plast Reconstr Surg. 1957;20(6):455-65.
8. Millard DR Jr. The unilateral cleft lip nose. Plast Reconstr Surg. 1964;34:169-75.
9. Millard DR Jr. Cleft craft: the evolution of its surgery, in the unilateral deformity. Boston: Little, Brown and Co.; 1976. p. 77-139.
10. Millard DR Jr. Earlier correction of the unilateral cleft lip nose. Plast Reconstr Surg. 1982;70(1):64-73.
11. Melega JM, Zanin AS, Psillakis JM. Cirurgia plástica reparadora e estética. 2ª ed. São Paulo: Medsi; 1992.
12. Skoog T. Repair of unilateral cleft lip deformity: maxilla, nose and lip. Scand J Plast Reconstr Surg. 1969;3(2):109-33.
13. Rees TD, Guy CL, Converse JM. Repair of the cleft lip nose: addendum to the synchronous technique with full-thickness skin grafting of the nasal vestibule. Plast Reconstr Surg. 1966;37(1):47-50.
14. Broadbent TR, Woolf RM. Cleft lip nasal deformity. Ann Plast Surg. 1984;12(3):216-34.
15. Mathes SJ, Noordhoff MS, Chen PKT. Plastic surgery. 2nd ed. Vol. 4. Philadelphia: Saunders Elsevier; 2006.
16. Blackwell SJ, Parry SW, Roberg BC, Huang TT. Onlay cartilage graft of the alar lateral crus for cleft lip nasal deformities. Plast Reconstr Surg. 1985;76(3):395-401.
17. Gunter JP, Friedman RM. Lateral crural strut graft: technique and clinical application in rhinoplasty. Plast Reconstr Surg. 1997;99(4):943-52.
Plastic Surgeon, Titular Member of the Brazilian Society of Plastic Surgery, Assistant Physician of the Hospital for Facial Deformities, Assistant Physician of the Municipal Children's Hospital Child Jesus, São Paulo, SP, Brazil
Correspondence to:
Guilherme Gurgel do Amaral Teles
Rua Dr. Samuel Porto, 237 - ap. 154 - Saúde
São Paulo, SP, Brazil - CEP 04054-010
E-mail: guilhermeteles77@yahoo.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: June 21, 2012
Article accepted: November 7, 2012
Work performed at the Hospital for Facial Deformities, São Paulo, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter