

Original Article - Year 2013 - Volume 28 -
Cutaneous sensitivity after reduction mammaplasty
Sensibilidade cutânea após mamoplastia redutora
ABSTRACT
INTRODUCTION: Understanding how to preserve the sensitivity of the nipple-areola complex with different reduction mammaplasty procedures is essential in order to provide better postoperative guidance to patients.
METHOD: Thirty women were selected to undergo reduction mammaplasty and were subsequently evaluated at three different time points: preoperatively, on postoperative day 30, and on postoperative day 180. To assess sensitivity, each areola was divided into four quadrants (P1-P4), with the nipple excluded (P5); therefore, five regions were evaluated. Four sensory tests were performed for each region: superficial touch, temperature (heat and cold), vibration, and pressure.
RESULTS: Compared with the preoperative evaluation, the evaluation performed on postoperative day 30 revealed a significant decrease in sensitivity to vibration in P5, to cold and heat in all regions, and to superficial touch in P3 and P5. On postoperative day 180, a significant decrease in sensitivity to cold was observed in P1, P2, and P5, and to heat in all regions except in P5, when compared with the preoperative period. A significant decrease in sensitivity to pressure in all regions was detected in the preoperative period when compared with postoperative day 30. On postoperative day 180, a significant decrease in sensitivity to pressure was observed in P2, P4, and P5 when compared with the preoperative period.
CONCLUSIONS: Superior medial pedicle reduction mammaplasty decreased the sensitivity of the nipple-areola complex to all sensory tests on postoperative day 30; however, on postoperative day 180, the sensitivity to temperature and pressure returned to normal. The nipple presented a more significant change in sensitivity than did the areolar region.
Keywords: Breast. Hypertrophy. Mammaplasty. Touch perception. Touch.
RESUMO
INTRODUÇÃO: O conhecimento sobre a preservação da sensibilidade do complexo areolopapilar da mama nas diversas técnicas de mamoplastia redutora é essencial para melhor orientar as pacientes sobre o pós-operatório.
MÉTODO: Foram selecionadas 30 mulheres submetidas a mamoplastia redutora, avaliadas em três tempos: pré-operatório e pós-operatórios de 30 dias e de 180 dias. Para avaliação da sensibilidade, as aréolas foram divididas em quatro quadrantes, além da papila, totalizando cinco regiões. Em cada região, foram testadas quatro modalidades sensoriais: toque superficial, temperatura (quente e fria), vibração e pressão.
RESULTADOS: Na avaliação no 30º dia, houve diminuição significante, em relação ao pré-operatório, da percepção à vibração em P5, ao frio em todos os pontos, ao calor em todos os pontos e ao toque superficial em P3 a P5. No pós-operatório de 180 dias, observou-se diminuição significante, em relação ao pré-operatório, da percepção ao frio em P1, P2 e P5 e ao calor em todos os pontos, exceto P5. Quanto à sensibilidade à pressão, notou-se diminuição significante em todos os pontos quando se compararam os períodos pré e pós-operatório de 30 dias. Na avaliação no pós-operatório de 180 dias, houve diminuição significante da sensibilidade à pressão em P2, P4 e P5, em relação ao pré-operatório.
CONCLUSÕES: A mamoplastia redutora com pedículo súpero-medial causou diminuição da sensibilidade do complexo areolopapilar no pós-operatório de 30 dias em todas as modalidades sensoriais, e no pós-operatório de 180 dias manteve-se para temperatura e pressão. A papila foi o ponto com maior alteração da sensibilidade.
Palavras-chave: Mama. Hipertrofia. Mamoplastia. Percepção do tato. Tato.
Breast hypertrophy is defined as an increase in breast size beyond the physiological limits, for reasons other than tumors, hemorrhages, inflammatory processes, and pregnancy1,2. It is characterized by a usually bilateral volumetric expansion of the breasts due to a predominant increase of adipose tissue and stroma, and partly of glandular parenchyma. Breast hypertrophy is the most common body contour deformity3,4.
Therefore, it is commonly associated with chronic physical, and sometimes disabling, disorders such as neck, back, shoulder, and breast pain; bad posture; appearance of grooves on the breasts from wearing a bra; skin problems; and difficulty in performing physical exercises. Breast hypertrophy is also often associated with psychological symptoms, arising, for instance, from changes in body contour, difficulty in dressing up, and having a low self-esteem2,5.
Without a symptomatic evaluation, the occurrence of mammary hypertrophy could be assessed through objective criteria that measure the average distance between the nipple and the inframammary fold, as well as between the nipple and the external lateral margin of the sternum. In a previous study, these measurements were taken separately to calculate the size of each breast, which was categorized as small when the average was < 9 cm, normal between 9.1 and 11 cm, and large at > 11.1 cm6.
One of the main aims of plastic surgery concerning reduction mammaplasty is to develop a surgical technique that will satisfy the patient requirements in terms of shape and size, in addition to maintaining the ability to breastfeed, avoiding visible scars, and preventing complications related to the nipple-areola complex (NAC) circulation, as well as the partial or complete loss of breast sensitivity7,8. Several factors are associated with changes in breast sensitivity after surgery, including the volume resected, excessive detachments, and resections in the lateral quadrants and at the base of the breasts9,10.
Breast sensitivity arises from the expression of cutaneous receptors, commonly localized throughout the skin and divided into three groups: free nerve endings, sensitive to pain and temperature, rapidly adapting receptors (Pacinian and Meissner's corpuscles); receptors sensitive to touch and movement; and slowly adapting receptors (Merkel and Ruffini cell-neurite complexes), to perceive the duration of the stimulus applied11. Breast innervation derives from the lateral and medial cutaneous branches of the second to the sixth intercostal nerves. NAC sensitivity is mostly due to a deep branch of the anterior division deriving from the lateral branch of the fourth intercostal nerve12.
Previously, postoperative breast sensitivity was evaluated by subjective methods, as it is difficult to quantify potential changes. Nowadays, several methods allow to quantitatively evaluate breast sensitivity, such as the use of a pressure-specified sensory device (PSSD); dermatomal somatosensory evoked potentials11,13; and simpler instruments such as Semmes-Weinstein monofilaments (for pressure), tuning forks, water at different temperatures, and cotton balls5.
Many studies about preoperative and postoperative cutaneous sensitivity, analyzing the different techniques of reduction mammoplasty, could be found in the literature. However, studies referring to the superior medial pedicle technique are rare. The superior medial pedicle technique was designed from the superior pedicle, aiming to reduce the tension and increase the arc of rotation to transpose the flap containing the NAC upward, without causing major impairments of blood supply. This technique may be applied to breasts presenting different levels of hypertrophy and ptosis, and may be performed within a reasonable surgical time8,14,15.
Therefore, this study aims to evaluate cutaneous sensitivity before and after a superior medial pedicle reduction mammaplasty.
METHOD
The study design was approved by the ethics research committee of our institution, and all patients involved in the study signed the informed consent form.
A total of 30 consecutive patients > 18 years old, with a body mass index (BMI) between 19 and 30 kg/m2, and presenting breast hypertrophy were included in this study. Therefore, all of them were candidates for a bilateral reduction mammaplasty. Patients who had previously undergone different surgical repairs or breast aesthetic procedures, those with other diseases affecting the breasts, those who were smokers or had stopped smoking for < 1 month, those with a history of childbirth or breast feeding of < 1 year, and those with uncontrolled chronic comorbidities were excluded. The selected patients were evaluated preoperatively and on postoperative days 30 and 180.
The night before the surgery, after the sensitivity tests, the patients were photographed while in a standing position, capturing frontal and lateral views at 45º and 90º angles, thus obtaining images of the trunk corresponding to the distance from the sternal notch to the umbilical scar. Then, also with the patient in the orthostatic position, we proceeded in marking the area where an inverted T-shaped scar would develop (Figure 1).
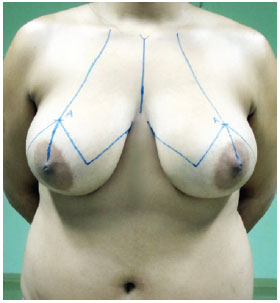
Figure 1 - Preoperative marking for reduction mammaplasty that would result in an inverted T-shaped scar.
During surgery, carried out under general anesthesia and with cephalothin (2 g) as antibiotic prophylaxis, we marked the NAC and decorticated the area of the pedicle with the patient in supine position (Figure 2). We then proceeded with suprafascial glandular detachment, delimitation, and preparation of the superior medial pedicle. The breast tissue was removed according to the presurgical cutaneous marking (Figure 3). Then, the pedicle containing the NAC was rotated by 90º toward point A (Figure 4). The breast was assembled by using nylon threads (Mononylon 3.0 Ethicon, Johnson & Johnson), and once the area in which the NAC would be externalized was demarcated and decorticated, the NAC was sutured (Mononylon 5.0 Ethicon, Johnson & Johnson) at isolated points. Sutures were performed in planes (subcutaneous with separate points and skin with intradermic sutures) by using absorbable threads (Monocryl 4.0 Ethicon, Johnson & Johnson) (Figure 5). The sterile gauze and micropore dressing were replaced after 24 hours. Cefadroxil (500 mg) was prescribed every 12 hours for 7 days. The points used for the NAC sutures were removed after 5 days, and the patients were instructed to wear a bra and to rest for 1 month.
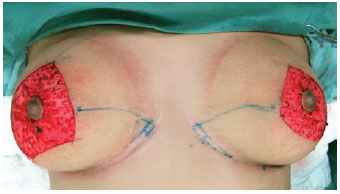
Figure 2 - Marking and decortication of the pedicle area.

Figure 3 - A, suprafascial dissection of the breast tissue. B, marking of the superior-medial pedicle. C, preparation of the pedicle and resection of the breast tissue.
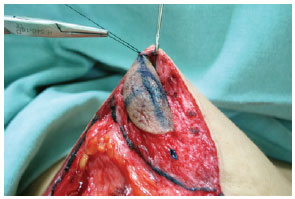
Figure 4 - Upward rotation of the nipple-areola complex by 90° toward point A.
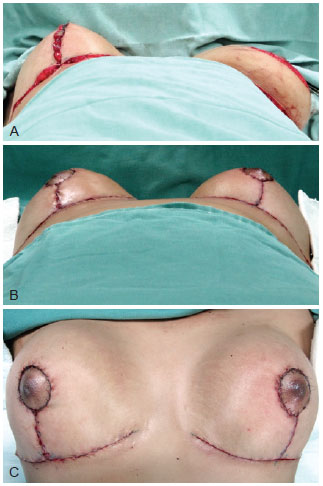
Figure 5 - A, Breast assembly. B and C, final appearance.
Sensitivity was assessed in the NAC, bilaterally, in the standardized superolateral, superior-medial, inferior medial, and inferior-lateral quadrant regions of the breast (P1-P4, respectively) and in the nipple (P5) (Figure 6).
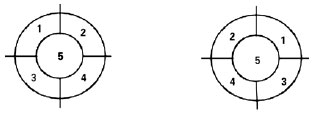
Figure 6 - Representation in quadrants of the location of the standardized points corresponding to the nipple and the areola.
In each region, four sensory tests were carried out: superficial touch, temperature (heat and cold), vibration, and pressure. Sensitivity to superficial touch was tested by gently passing a hydrophilic cotton ball over the skin, contacting the breast. Sensitivity to temperature (cold and heat) was tested by using tubes containing crushed ice (0ºC) and water heated at 60ºC, respectively. The tubes were gently placed on the skin and maintained there for 2 seconds. Sensitivity to vibration was evaluated by placing a vibrating tuning fork, with a frequency of 128 vibrations per second, in contact with the skin (Figure 7).

Figure 7 - Instruments used in the study (from left to right): test tube for hot water and crushed ice, thermometer for autoclave temperature measurement, tuning fork, cotton ball, and Semmes-Weinstein monofilaments.
For the superficial touch, hot and cold temperature, and vibration tests, the responses were recorded as positive if the patients perceived the stimulus and negative otherwise.
The sensitivity to pressure was measured by using Semmes-Weinstein aesthesiometer monofilaments16 of different calibration diameters. Up to six monofilaments were placed on the skin at each time evaluating each topographic region. These filaments correspond to 300 g, 10 g, 4 g, 2 g, 0.2 g, and 0.05 g threshold/potential skin pressure, respectively. Enough pressure was exerted until the monofilament placed over the skin was bent. Thereafter, the pressure was removed and, after 5 seconds, the monofilaments were removed from the skin17. The response was considered positive when the patients perceived the touch/skin pressure and negative otherwise.
After all evaluations were performed in all patients, we decided to use a random side (left or right) to analyze the data. This randomization was performed by using the Bioestat 5.0 software.
McNemar's test was used to compare the time points evaluated in relation to sensitivity to superficial touch, temperature, and vibration, whereas Friedman's analysis of variance was used to compare the time points evaluated in relation to pressure. Wilcoxon test was used to compare the dry weight of the right and left breasts.
RESULTS
The age of the patients varied between 18 and 54 years (average: 34 years) and their BMI from 20.8 to 28.7 kg/m2 (average: 25.1 kg/m2). The total weight of breast tissue removed varied between 250 and 1.930 g (average: 837.5 g). No statistical difference was observed between the dry weight of the right and left breasts (p = 0.21).
When compared with the preoperative period, the evaluation on postoperative day 30 revealed a significant decrease in sensitivity to vibration in P5 (p = 0.000), to cold in all points (p = 0.000 for P1, P2, P4, and P5 and p = 0.03 for P3), to heat in all points (p = 0.01 for P1 and P4 and p = 0.000 for P2, P3, and P5), and to superficial touch in P3 to P5 (p = 0.000 for P3, p = 0.01 for P4, and p = 0.03 for P5). Concerning sensitivity to pressure, we noticed a significant decrease in all points when comparing the preoperative and 30-day postoperative periods (p < 0.05).
When compared with the preoperative period, the evaluation on postoperative day 180 showed a significant decrease in sensitivity to cold in P1, P2, and P5 (p = 0.03 for all points), and to heat in all points except in P5 (p = 0.01 for P1 and p = 0.03 for all other points). We also observed a significant decrease in sensitivity to pressure in P2, P4, and P5, when compared with the preoperative period (p < 0.05).
No statistical difference was observed between the evaluation on postoperative days 30 and 180 in all points and for all sensory tests.
DISCUSSION
Previous studies described that hypertrophic breasts are less sensitive than normotrophic breasts. Those studies associated this condition to the neuropraxia caused by the stretching and prolonged traction of sensory branches as well as the increased skin coverage because of the bigger breast volume9,18. Anatomical studies revealed that the deep branch of the fourth intercostal lateral nerve is mainly responsible for NAC sensitivity12.
The number of publications referring to potential changes in breasts sensitivity after a reduction mammoplasty has recently increased, thus reinforcing the importance of the choice of the surgical technique for this procedure and the tools for evaluating sensitivity10,11,19.
The clinical impression is that after an initial decrease in breast sensitivity, normal sensitivity is recovered a few months after surgery. However, the literature presents contradictory data and lacks detailed studies on the subject10,11.
Several tools are available for assessing skin sensitivity; however, there are discrepancies about their reproducibility and accuracy9,11,13,17.
We decided to use Semmes-Weinstein monofilament testing, as this is an objective and quantitative method for a controlled evaluation of pressure and is already used by other authors for assessing breast skin sensitivity10,16. The other instruments used in this study have been previously used and also proven to efficiently assess the sensory tests described herein16,20.
Currently, in reduction mammoplasty, it is essential to understand how to preserve NAC and breast skin sensitivity with the different techniques used, to allow better education of patients about the postoperative outcome10.
Among the studies that used monofilaments, none was found to assess hypertrophic breasts treated with the technique described herein; the most similar works were those that used the superior pedicle for the NAC5,10,19. Furthermore, no studies evaluated specific regions of nipple quadrants, as we did in our study; previous studies used nipple cardinal points5,10,11,19.
Only one prospective study that used the superior medial pedicle was found in the literature, which showed a decreased sensitivity in all regions. Moreover, this study evaluated only sensitivity to pressure, by using another instrument (PSSD). This means that further and more comprehensive studies would be required11.
Other studies that were reviewed and that used the same instruments, although with different pedicles, revealed different results concerning sensitivity to either hot or cold temperature. Different sensitivities to pressure (reduced, similar, and increased) were observed in all regions5,10,19.
The method used in this study was efficient and may be used to evaluate breast skin sensitivity with different techniques of reduction mammaplasty, among other surgeries.
Further investigations on breast sensitivity after a superior-medial pedicle reduction mammaplasty would be required, considering the broad use of this technique.
CONCLUSIONS
Superior-medial pedicle reduction mammaplasty decreased NAC sensitivity to all sensory tests evaluated in a postoperative period of 30 days, whereas this reduction was maintained for temperature and pressure sensory tests at 180 days after surgery. The nipple was the region that presented more changes in sensitivity.
REFERENCES
1. Foged J. Symptomatology of breast hypertrophy. Ugeskr Laerger. 1953;115(12):439-51.
2. Freire M, Sabino Neto M, Garcia EB, Quaresma MR, Ferreira LM. Functional capacity and postural pain outcomes after reduction mammoplasty. Plast Reconstr Surg. 2007;119(4):1149-56.
3. Cruz-Korchin N, Korchin L, González-Keelan C, Climent C, Morales I. Macromastia: how much of it is fat? Plast Reconstr Surg. 2002;109(1):64-8.
4. Tafuri LSA, Gobbi H. Epithelial hyperplasia in specimens from bilateral reduction aesthetic mammaplasty and reduction mammaplasty contralateral to breast cancer. J Bras Patol Med Lab. 2005;41(2):1-8.
5. Gonzales F, Brown FE, Gold ME, Walton RL, Shafer B. Preoperative and postoperative nipple-areola sensibility in patients undergoing reduction mammaplasty. Plast Reconstr Surg. 1993;92(5):809-18.
6. Sacchini V, Luini A, Tana S, Lozza L, Galimberti V, Merson M, et al. Quantitative and qualitative cosmetic evaluation after conservative treatment for breast cancer. Eur J Cancer. 1991;27(11):1395-400.
7. Serletti JM, Reading G, Caldwell E, Wray RC. Long-term patient satisfaction following reduction mammoplasty. Ann Plast Surg. 1992;28(4):363-5.
8. Orlando JC, Guthrie RH Jr. The superomedial dermal pedicle for nipple transposition. Br J Plast Surg. 1975;28(1):42-5.
9. Spear ME, Nanney LB, Phillips S, Donahue R, Rogers KM, Wendel JJ, et al. The impact of reduction mammoplasty. Ann Plast Surg. 2012;68(2):142-9.
10. Chiari A Jr, Nunes TA, Grotting JC, Cotta FB, Gomes RC. Breast sensitivity before and after the L short-scar mammoplasty. Aesthetic Plast Surg. 2012;36(1):105-14. Epub 2011 Jun 3.
11. Ferreira MC, Costa MP, Cunha MS, Sakae E, Fels KW. Sensibility of the breast after reduction mammaplasty. Ann Plast Surg. 2003;51(1):1-5.
12. Würinger E, Mader N, Posch E, Holle J. Nerve and vessel supplying ligamentous suspension of the mammary gland. Plast Reconstr Surg. 1998;101(6):1486-93.
13. DelVecchyo C, Caloca J Jr, Caloca J, Gómez-Jauregui J. Evaluation of breast sensibility using dermatomal somatosensory evoked potentials. Plast Reconstr Surg. 2004;113(7):1975-83.
14. Foustanos A, Panagiotopoulos K, Skouras G. Intraoperative modification of Pitanguy technique of reduction mammoplasty for elevation of the nipple-areola complex in case of severe breast ptosis. Aesthetic Plast Surg. 2011;35(1):55-60. Epub 2010 Aug 20.
15. Landau AG, Hudson DA. Choosing the superomedial pedicle for reduction mammoplasty in gigantomastia. Plast Reconstr Surg. 2008;121(3):735-9.
16. Spear SL, Hess CL, Elmaraghy MW. Evaluation of abdominal sensibility after TRAM flap breast reconstruction. Plast Reconstr Surg. 2000;106(6):1300-4.
17. Vilet V, Novak CB. Duration of contact time alters cutaneous pressure threshold measurements. Ann Plast Surg. 1993;31(4):335-9.
18. Godwin Y, Valassiadou K, Lewis S, Denley H. Investigation into the possible cause of subjective decreased sensory perception in the nipple-areola complex of women with macromastia. Plast Reconstr Surg. 2004;113(6):1598-606.
19. Schlenz I, Rigel S, Schemper M, Kuzbari R. Alteration of nipple and areola sensitivity by reduction mammaplasty: A prospective comparison of the five techniques. Plast Reconstr Surg. 2005;115(3):743-51.
20. Farah AB, Nahas FX, Ferreira LM, Mendes JA, Juliano Y. Sensibility of the abdomen after abdominoplasty. Plast Reconstr Surg. 2004;114(2):577-82.
Plastic Surgeon, Residency Program Preceptor at the Plastic Surgery Service of Clínicas Samuel Libânio Hospital, University of Vale do Sapucaí, and Member of the Brazilian Society of Plastic Surgery, Pouso Alegre, MG, Brazil
Correspondence to:
Edgard da Silva Garcia
Rua Dr. Raimundo Alves Chaves, 17 - Santa Lúcia
Pouso Alegre, MG, Brazil - CEP 37550-000
E-mail: edgard.garcia@uol.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: 26/7/2012
Article accepted: 15/12/2013
Work was performed at Hospital Universitário de Pouso Alegre, Pouso Alegre, MG, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter