

Original Article - Year 2013 - Volume 28 -
Evaluation of laser lipolysis: 10 years of experience with 766 patients
Avaliação de 10 anos de laserlipólise em 766 pacientes
ABSTRACT
BACKGROUND: Laserlipolisis is a surgical procedure that uses a Nd:YAG laser for treatment of localized lipodistrophies as an isolated or associated method. The present study aims to evaluate the results of laserlipolisis with Nd:YAG laser based on a retrospective survey.
METHOD: Retrospective evaluation with 766 patients in 792 procedures from August 2001 to August 2011.
RESULTS: Mean follow-up was 6.5 years (78 months). The most frequent indication was lipodistrophy of abdomen, flancs and dorsum. A satisfaction questionnaire showed 96% of patients satisfied.
CONCLUSIONS: Laserlipolisis brought several benefits to obtained results as better accomodation of skin, skin retraction, less edema and bleeding, favoring treatment of more extensive areas as well as more complex regions as gynecomastias, secondary liposuction and dorsal regions, with better postoperative recovery.
Keywords: Nd:Yag laser. Laserlipolisis. Laser-assisted liposuction. Nd:Yag laser.
RESUMO
INTRODUÇÃO: A técnica de lipoaspiração a laser (laserlipólise) é um procedimento cirúrgico que se utiliza de um aparelho de laser do tipo Nd:YAG (neodymium-doped:yttrium-aluminum garnet) para o tratamento de adiposidades localizadas, seja como método isolado ou associado a outros procedimentos tradicionais de cirurgia plástica. Este estudo teve por objetivo avaliar os resultados do uso da lipoaspiração com laser Nd:YAG no tratamento das lipodistrofias, baseado em avaliação retrospectiva de 10 anos.
MÉTODO: Estudo retrospectivo, que avaliou 766 pacientes (792 cirurgias) submetidos ao procedimento entre agosto de 2001 e agosto de 2011.
RESULTADOS: O seguimento médio dos pacientes foi de 6,5 anos (78 meses). A indicação mais frequente para o procedimento foi para o tratamento das regiões de abdome, flancos e dorso. O resultado do questionário de satisfação demonstrou que 96% dos pacientes consideraram o resultado satisfatório
CONCLUSÕES: Aaplicação da laserlipólise trouxe vários benefícios adicionais aos resultados, como a constatação de melhor acomodação e retração da pele, menor edema e sangramento, possibilidade de tratamento de áreas de maior complexidade para a lipoaspiração convencional, como ginecomastia, dorso e lipoaspiração secundária, além de melhor recuperação pós-operatória.
Palavras-chave: Laserlipólise. Lipoaspiração a laser. Laser Nd:Yag.
Since the publication by Fischer & Fischer1, in 1976, describing the first liposuction, which was subsequently popularized by Illouz2, modern plastic surgery has witnessed the evolution, consolidation, and global dissemination of this surgical technique. Various existing techniques allow the removal of significant volumes of localized fat via small incisions and have been improved to minimize trauma and produce better and more reproducible results. Improvements include the introduction of thinner and less traumatic cannulas, the infiltration of subcutaneous vasoconstrictive solutions, and liposuction techniques at various depths (i.e., intermediate and superficial).
Liposuction and its variants are currently among the most performed plastic surgical procedures worldwide. In the USA, the American Academy of Cosmetic Surgery reported that 959,787 liposuctions were performed in 20093. According to the American Society of Plastic Surgeons, in 2010, its associates performed 203,106 procedures4. Furthermore, according to a study by DATAFOLHA5 requested by the Brazilian Society of Plastic Surgery in 2009, k liposuction was the second most performed surgery in Brazil.
With the evolution of technology, new methods including approaches, materials, and techniques for the removal of adipose tissue have been developed and added to existing ones. The techniques of body fat contouring and removal have evolved since the advent of the method by Illouz in 19796 using aspiration with syringes in dry liposuction7. Developments include the use of tumescent solution8, superficial liposuction9, and combination with techniques utilizing compressed air or electric motors, such as in vibroliposuction10, ultrasound-assisted liposuction11, liposuction with pressure water jets12, and laser-assisted liposuction13.
Despite such progress in liposuction, major concerns include safe control of the total aspirated volume to avoid compromising the viability of the adjacent skin as well as the control of clinical and hemodynamic repercussions. The aim remains satisfactory body contours with minimum edema and short recovery time.
New technologies such as laser-assisted liposuction, also called laser lipolysis, mainly aim to increase benefits and safety. The possibility of reduced intraoperative bleeding in the procedure, allowing the removal of larger volumes of fat more safely while reducing postoperative edema offers many advantages to patients.
The use of lasers as an adjuvant in liposuction was first described in 1994 by Apfelberg et al.13, who reported a series of results from a study that included 5 plastic surgery centers and was approved by the FDA. In that study, the liposuction cannula used had a thin optical fiber inside that pulses the energy from a 40-W Nd:YAG laser beam. The laser acts only on the already aspirated adipose tissue through the orifice of the cannula, simultaneously coagulating the blood vessels. In 1996, Apfelberg14 updated and expanded this study; although the results were not completely conclusive, less blood loss, shorter recovery time, and fewer complaints of pain, edema, ecchymosis, and discomfort in the immediate postoperative period were observed. However, the study was discontinued. In 1997 and 1999, Cook15,16 reported experience with vaporization of the subcutaneous tissue of the face using an Nd:YAG laser. Blugerman17 in 2000 and Schavelzon et al.18 in 2001 reported good results using the actual laser lipolysis technique. In 2001, Neira19,20, Neira & Zúñiga21 and Neira & Isaza22 reported experience with an external laser acting on adipose tissue as well as the hemodynamic variables and lidocaine levels associated with the procedure. In Brazil, Goldman et al.23,24 were the first to utilize this technology and was followed by Badin et al.25, who described the effect of laser treatment on flaccidity.
Based on the literature and our interest in the new technologies, we began performing laser lipolysis with the aim of providing better results in liposuction procedures.
We assessed the results of liposuction by using a Nd:YAG laser for the treatment of lipodystrophy in a 10-year retrospective study.
METHOD
From August 2001 to August 2011 (120 months), 766 patients with lipodystrophy were treated by a total of 792 surgical procedures by the author at his private clinic. All procedures were performed in a surgical environment with the assistance of an anesthesiologist. There were 561 (70.9%) women and 231 (29.1%) men. Age ranged between 17 and 72 years, with a mean of 38 years.
The technique was indicated for the treatment of localized lipodystrophy and adipose tissue irregularities in healthy patients, whose weight was close to ideal and body mass index (BMI) was less than 30.
The following preoperative tests were ordered in all cases: complete blood count, complete coagulogram, glucose, urea, creatinine, HIV, beta hCG (for women of reproductive age), and routine urine test. Patients aged > 40 years were systematically evaluated by a cardiologist to determine surgical risk.
All patients underwent pre-anesthesia evaluation by an anesthesiologist.
Surgical Technique
The patients were measured, weighed, and photographed in a standardized manner (i.e., always against a uniform and opaque sky-blue background) on the evening of the surgery. The areas to be treated were marked the day before or before anesthesia, with the patient standing in front of a mirror, actively participating and pointing out their dissatisfaction. By using an appropriate pen, markings of circles and symbols identifying the areas with excess and insufficient fat accumulation, deformities, and asymmetries were identified.
Prophylactic antibiotic therapy (cefazolin 2 g, intravenously) was administered approximately 20 minutes before the start of the procedure; cefazolin 1 g was routinely administered 2 hours after the start of surgery. The patients received a permanent vesical catheter to monitor urine output and for postoperative comfort, except for patients with local anesthetic blockade. Routine antisepsis was performed using iodopovidone.
The patients were in the supine or prone position, which was not changed during laser passage or aspiration. For protection, foam was placed under the heels and pillows under the knees when patients were in the supine position as well as under the feet when they were in the prone position. From 2009 onwards, all patients routinely wore compressive elastic stockings using a pneumatic compression system (SCD SEQUEL® System) and were up by an average of 6 hours after the end of the procedure to prevent venous thromboembolism.
Once the patient was anesthetized, a peristaltic infusion pump was used with solution containing 1 mg adrenalin for every 500 mL saline solution in the infiltration process. The volume of injected solution varied according to the amount and location of fat being treated. In cases in which local anesthesia was used, the solution also contained xylocaine and naropin. The procedure was initiated approximately 20 minutes after infiltration by applying the microcannula with the laser fiber and subsequently performing aspiration.
In laser lipolysis, we used Nd:YAG laser DEKA LASER equipment (SmartLipo®, Deka, Calenzano, FI, Italy) with a wavelength of 1064 nm associated with a helium-neon (HeNe) laser source for external visualization of the Nd:YAG laser by the operator. The laser beam was conveyed to the adipose tissue via a 300-µm optical fiber fitted inside a stainless steel microcannula 1 mm in diameter (Figure 1) and 25 cm long. A 2-3-mm segment of exposed optical fiber was exteriorized relative to the distal microcannula of the cannula; the laser only targets this site (Figure 2). Although the effect of the laser is internal, adequate protection of the patient and surgical team was ensured with the use of special glasses to avoid accidental exposure to the beam.

Figure 1 - Microcannula to which the optical fiber is coupled.
Figure 2 - Optical fiber exteriorized, and pulsing of the laser in the extremity of the 1-mm cannula.
Small 3-mm incisions were made depending on the areas to be treated, and the microcannula was inserted. Reciprocating fan-like movements were performed at different levels of depth, similar to the movements performed during liposuction; these movements are significantly facilitated by the laser, and it is possible to monitor the laser's action by the light beam of the HeNe laser (Figure 3). The color of the HeNe laser on the skin was observed as transillumination; the surgeon operated the equipment by using a pedal. Light in the operating room was reduced to allow visualization of the transillumination effect.

Figure 3 - Visualization of the laser by transillumination.
The laser action time as well as the energy produced and subsequently accumulated in the treated area were measured in Joules; the amount of energy was checked constantly during the control of the microcannula via the equipment's control panel. The area being treated was assessed by transoperative palpation performed constantly during the passage of the cannula with the laser fiber.
The oily solution that remains dispersed in the treated areas was definitively drained by suction using thin 2-, 3-, or 4-mm multi-perforated cannulas coupled to the aspirator. Using a negative pressure < 650-700 mmHg, the final product of laser lipolysis was gently removed from the treated areas without excessive physical effort required from the surgeon. The subsequent routine is similar to that in conventional liposuction, with suturing using mononylon 6-0 and occlusive dressing with Opsite® or Sterilstrip®.
Before the procedures, we determined the maximum aspirated volume in this sample would not exceed 7% of body weight as recommended for infiltrative techniques in article 9 of the guideline of the Federal Council of Medicine (CFM Resolution 1711 of 10 December 2003) and the SBCP.
The average preoperative hydration of patients was 500 mL per surgical hour, and there was no need for hypervolemic therapy26,27.
We applied compressive dressings with box-like polyethylene pyramid foam with a density of 23 only to the abdominal area and removed them after 48 hours, followed by the immediate placement of elastane girdles. We only prescribed analgesics or anti-inflammatory drugs in addition to guidance on general care.
Manual lymphatic drainage was initiated during the first postoperative week usually on the fifth day postoperatively. All patients underwent 1-hour lymphatic drainage sessions 2-3 times per week for an average of 15 sessions.
Postoperative follow-up was performed at 24 and 48 hours, and weekly thereafter until 2 months postoperatively; thereafter, monthly follow-up was performed until 1 year. During follow-up, the patients were reassessed, weighed, measured, and photographed.
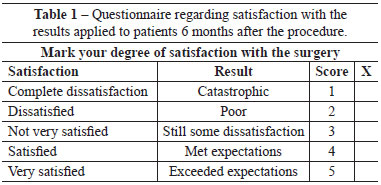
A questionnaire regarding satisfaction with the results (Table 1) was conducted after 6 months. The patient scored the results from 1-5: 1, complete dissatisfaction (catastrophic result); 2, dissatisfied (poor result, did not meet expectations); 3, not very satisfied (some dissatisfaction); 4, satisfied (met expectations); and 5, very satisfied (exceeded expectations).
RESULTS
The mean follow-up was 6.5 years (78 months).
The most frequent indication for the procedure was the treatment of the abdomen, flanks, and back, accounting for 645 cases (81.4%). Some areas were treated in an isolated procedures, such as gynecomastia in 64 cases (including 39 cases with local anesthesia) and trochanteric regions (including 21 cases with local anesthesia).
Regarding anatomical location, the areas treated were as follows: abdomen (n = 681), flanks (n = 670), back (n = 653), inner thighs (n = 503), gynecomastia (n = 76), trochanteric regions (n = 52), arms (n = 34), chin (n = 27), knees (n = 25), and axilla (n = 14); n indicates the number of treated areas, adding 2 areas per bilateral procedure with the exception of the abdomen (Figure 4). The total number of treated areas was 2735.
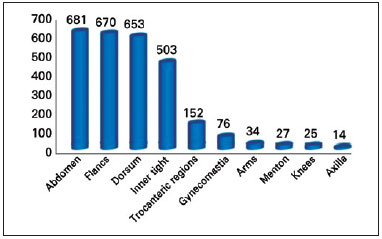
Figure 4 - Treated areas.
The procedures were performed under general anesthesia (35.4%) or sedation assisted by an anesthesiologist (64.6%) (Figure 5). Peridural blockade was used in 682 cases (86.1%). In 50 cases, peridural blockade was not performed either because of technical difficulty or a patient-surgeon joint decision. Sixty-one surgeries (7.7%) were performed with local anesthesia and sedation only (Figure 6).
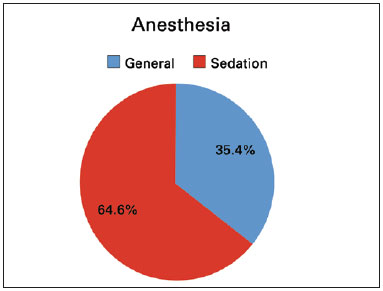
Figure 5 - Anesthesia.

Figure 6 - Blockade.
The mean aspirated volume was 2650 mL (range: 350-7200 mL), and the mean volume of infiltrated solution was 1466 mL (range: 300-3500 mL). Furthermore, 740 patients (96.6%) had a BMI < 30; mean weight was 58.7 kg (range: 49-132 kg), and mean height was 1.60 m (range: 1.48-2.01 m).
The total aspirate was placed in a graduated container for observation after decantation of the lipid and blood components.
Laser lipolysis was associated with breast surgery in 168 cases (30% of female cases); it was also associated with the resection of a small spindle of abdominal skin in 223 cases (28.1%) including 24 in nulliparous women - most of whom lost significant weight and gained abdominal flaccidity as a result. Among these 223 cases, only 5 cases were male for the same reasons mentioned earlier.
A second intervention for complementation or revision was performed in 26 cases (3.28%); in 6 cases, the second procedure was planned during the first surgery. No cases received a third intervention.
Among all procedures, 95.08% were ambulatory surgical procedures, with patients being discharged on the same day; only 39 patients (4.92%) stayed in the hospital overnight.
Moreover, 84.6% of patients (670 procedures) returned to routine activities after the second postoperative day; restricted physical activity was recommended for at least 15 days depending on the surgical combination.
Postoperative complaints of pain were deemed discrete. Most patients were successfully medicated with oral non-opiate analgesics.
The satisfaction questionnaire showed that 96% of patients were satisfied with the results (Figure 7).
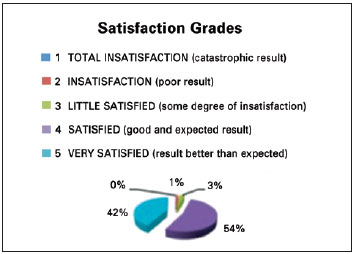
Figure 7 - Patient satisfaction.
Lymphatic drainage was performed on 657 patients (83%) under our supervision and by a physiotherapist indicated by us. For the remaining 17%, lymphatic drainage was performed by other professionals because of logistic issues or because they did not reside near the hospital.
Among the 766 patients treated, there were 27 cases of asymmetry (3.4%), 188 cases of seroma (23.7%), and 4 cases of infection (0.5%, all Staphylococcus epidermides), which were treated by re-hospitalization and intravenous antibiotic therapy.
Figures 8 to 13 illustrate some clinical cases of this study.
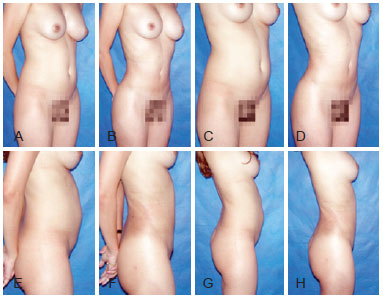
Figure 8 - Preoperative and 6-month postoperative photographs of a 31-year-old with lipodystrophy of the abdomen, flank, and back.

Figure 9 - Preoperative and 6-month postoperative photographs of a 35-year-old patient with lipodystrophy of the abdomen, flank, and back.

Figure 10 - Preoperative and 7-month postoperative photographs of a 28-year-old patient with lipodystrophy of the abdomen, flank, and back.
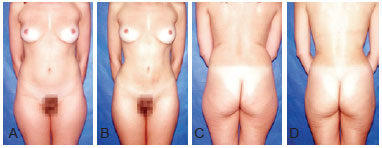
Figure 11 - Preoperative and 6-month postoperative photographs of a 42-year-old patient with lipodystrophy of the abdomen, flank, back, inner thigh, and trochanteric region.
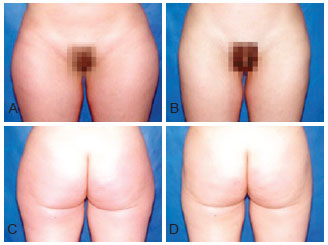
Figure 12 - Preoperative and 6-month postoperative photographs of a 23-year-old patient with lipodystrophy of the trochanteric region.
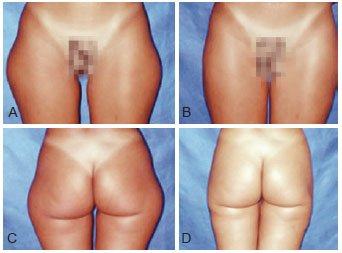
Figure 13 - Preoperative and 6-month postoperative photographs of a 37-year-old patient with lipodystrophy of the trochanteric region.
DISCUSSION
New medical equipment and techniques that provide significant benefits to patients are developed continuously. However, conventional lipoplasty methods have a critical limitation related to the amount of fat removed because of the associated blood loss and its consequences on safety and patient recovery in the immediate postoperative period.
Laser lipolysis and ultrasound-assisted liposuction28 treat fat in a manner different from conventional liposuction; fat is removed via a process called cavitation, which involves the implosion of adipose cells followed by lysis and emulsification29-33.
The use of lasers with specific wavelengths on adipose tissue produces a photohyperthermic effect in which light energy is transformed into heat via interaction with the proteins present on the surface of adipocytes. This causes the adipocyte to implode, definitively destroying it; the subsequently leaked the fatty acid content of adipocytes23 is aspirated, making the procedure less traumatic.
There are 2 important points for preventing thermal injury when using this technique. First, the laser energy should only be applied in a wet environment, i.e., after adequate subcutaneous infiltration of the solution described above. Gingrass & Kenkel34 demonstrate significant temperature elevation (as high as 50ºC) in experimental models using ultrasound-assisted liposuction when the subcutaneous tissue is not infiltrated34,35. We decided to follow this principle in laser lipolysis as well.
Second, the cannula must be maintained with the laser fiber in constant movement during its passage through the fatty tissue. The surgeon's non-dominant hand should be permanently flattened to palpate the skin and feel the tip of the cannula as in conventional liposuction; this is always guided by the transillumination provided by the HeNe laser.
The continuous visualization of the red light emitted by the HeNe laser as a result of transillumination through the skin allows the surgeon to know exactly where the tip of the microcannula laser beam is, thus ensuring safety. The amount of energy applied is constantly checked on the equipment's panel during the handling of the microcannula and directly depends on the amount of fat, tissue resistance, and extent of the area to be treated. These measures allow the delivery of consistent amounts of energy to bilateral areas such as the flanks, trochanteric regions, inner thighs, etc. The average amount of energy is 2000 J, for example, to treat the abdomen36. Controlling and monitoring of these values through the equipment's monitor are also extremely important for symmetric execution of the technique in bilateral areas and at the end of laser application.
Some key elements should be taken into consideration for finishing laser treatment. In particular, the loss fatty tissue resistance while the cannula is moving and the presence of a large amount of blood observed in the subsequently aspirated fluid through the transparent tube should be kept in mind37,38.
The role of wet solutions in the evolution of both the conventional and other liposuction techniques is worth mentioning. In the early days of liposuction in 1983, Fournier39 used the dry method, i.e., without any subcutaneous infiltration. In 1980, Illouz2, the pioneer of modern liposuction, had already introduced the use of cannulas with round tips and infiltration with hyaluronidase. The technique of super wet infiltration, i.e., the use of 1.5 mL solution for every 1 mL aspirated fat was first described by Fodor & Watson40. In 1993, Klein41 reported the technique of tumescent infiltration, which involves the infiltration of a large volume of solution into the subcutaneous tissue, significantly facilitating the execution of liposuction. Blood loss was partially controlled with the advent of tumescent infiltration; this abundant infiltration of fluids into the adipose tissue using a solution containing mainly saline, adrenaline, bicarbonate, and lidocaine allowed for larger amounts of fat to be removed more safely with less trauma regardless of the choice of anesthesia.
The advent of laser lipolysis allowed the treatment of areas that were traditionally more difficult to aspirate, such as the dorsal region or breasts including cases of gynecomastia42; this is because the microcannula containing the laser fiber is only 1 mm in diameter and its penetration is considerably facilitated by the energy generated by the laser, thereby requiring less effort by the surgeon. This satisfactory facilitation is also observed in areas previously operated on. Interesting results have been obtained with regard to flaccidity. Moreover, the technique results in satisfactory results and fast recovery. With conventional liposuction, the treatment of these areas would still be difficult to perform43,44.
The laser creates small tunnels in the fat, and the delicate protein-rich membranes of adipocytes are photothermally disrupted, releasing their oily content (Figure 14). Histological analyses show significantly positive effects such as coagulation of the small vessels of adipose tissue (Figure 15), adipocyte disruption, reticular dermis reorganization, and coagulation of adipose tissue collagen (Figure 16). Vessel coagulation decreases the blood loss and the occurrence of ecchymosis. Collagen coagulation and dermal reorganization, which have been observed with other types of lasers, promote adequate tissue retraction45-49.
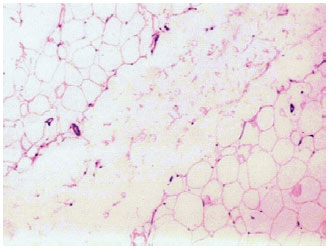
Figure 14 - Tunnel produced by the action of the Nd:YAG laser, showing disruption of adipocyte structure and fragments of adipose cell capsules (H&E stain, 32× magnification). (Courtesy of Dr. Alberto Goldman)
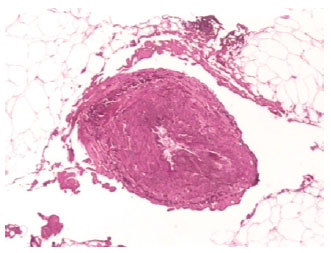
Figure 15 - Coagulation of a small vessel in adipose tissue after laser treatment (orcein stain, 32× magnification). (Courtesy of Dr. Alberto Goldman)
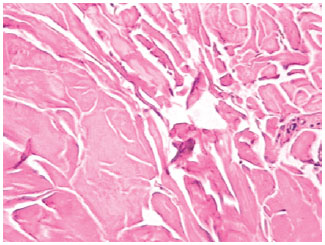
Figure 16 - Coagulation of collagen after laser treatment. (Courtesy of Dr. Alberto Goldman)
Because of the low rate of ecchymosis, which is easily observed in the treated areas in the immediate postoperative period, and the little or almost no postoperative discomfort, the need for stronger analgesics has been practically nonexistent; this demonstrates that this technique is less traumatic, i.e., less painful for patients.
The most important benefit of the technique is the high satisfaction with the surgery; the satisfaction questionnaire given 6 months postoperatively showed more than 93.2% of patients were satisfied (Figure 7). Therefore, this technique met the proposed treatment objectives.
Despite its advantages, laser-assisted liposuction has some disadvantages. First, surgery is slightly longer as a result of laser application in the areas to be treated, which is approximately 20 minutes on average. Furthermore, the surgeon must be trained to perform the technique and use the equipment, which has a learning curve. In addition, the equipment is quite expensive. In our experience with laser lipolysis, 188 cases of seroma were observed. This is explained by the use of tumescent infiltration and irritation of fatty acid residue that was not evacuated through aspiration. Despite these disadvantages, body contour improved markedly in the immediate and late (6-month) postoperative periods compared to the results of conventional liposuction alone. In addition, edema regressed rapidly, and strong pain and extensive areas of ecchymosis in the immediate postoperative period were almost nonexistent. These positive results are probably attributable to the more homogeneous fat removal, increased temperature in the deep dermis, which stimulates collagen contraction and subsequent skin retraction, and the removal of more fat owing to less vascular lesions and bleeding25,49.
Liposuction is currently one of the methods most used by plastic surgeons. Furthermore, the increasing literature on the subject has strengthened the foundations of this technique. Thus, this retrospective study adds data to the literature on the use of laser lipolysis50.
CONCLUSIONS
The results obtained with laser lipolysis are similar to those obtained with traditional liposuction methods. When used alone or as an adjuvant to conventional liposuction, laser lipolysis is an invaluable technique for the treatment of lipodystrophy. When used alone, this technique has some advantages, particularly improved patient recovery. Laser lipolysis has proven to be effective for the treatment of body contour irregularities after liposuction treatment.
REFERENCES
1. Fischer A, Fischer G. First surgical treatment for molding body's cellulite with three 5 mm incisions. Bull Int Acad Cosmet Surg. 1976;3:35.
2. Illouz Y. Body contouring by lipolysis: a five years experience with over 3000 cases. Plast Reconstr Surg. 1983;72:591-7.
3. American Academy of Cosmetic Surgery. 2009 Procedural Census. AACS, Chicago; 2010.
4. American Society of Plastic Surgeons. Report of the 2010 plastic surgery statistics. ASPS, Arlington Heights; 2010.
5. Sociedade Brasileira de Cirurgia Plástica. Cirurgia Plástica no Brasil. Pesquisa Datafolha 2009. Disponível em: http://www2.cirurgiaplastica.org.br/images/Docs/pesquisa2009.pdf.
6. Illouz YG. Une nouvelle technique pour les lipodystrophies localisées. Rev Chir Esth Franc. 1980;6(9).
7. Avelar J, Illouz YG. Lipoaspiração. São Paulo: Hipócrates; 1986.
8. Klein JA. Principles and tumescent technique. Cosmetic Surgery of the Skin. 1987;(4):263.
9. Bolivar de Souza Pinto E, Erazo IPJ, Prado Filho FS, salazar GH. Superficial liposuction. Aesth Plast Surg. 1996;20(2):111-12.
10. Fodor P. Power-assisted lipoplasty. Aesth Surg J. 2001;21(1):90-2.
11. Zocchi M. Ultrasonic-assisted lipoplasty. Clin Plast Surg. 1996;23(4):575-98.
12. Man D, Meyer H. Water jet-assisted lipoplasty. Aesth Surg J. 2007;27(3):42-6.
13. Apfelberg DB, Rosenthal S, Hunstad JP, Achauer B, Fodor PB. Progress report on multicenter study of laser-assisted liposuction. Aesth Plast Surg. 1994;18(3):259-64.
14. Apfelberg DB. Results of multicentric study of laser-assisted liposuction. Clin Plast Surg. 1996;23(4):713-9.
15. Cook WR. Laser neck and jowl liposculpture including platysma laser resurfacing, dermal laser resurfacing and vaporization of subcutaneous fat. Dermatol Surg. 1997;23(12):1143-8.
16. Cook WR. "Cook Weekend Alternative to the Facelift". Liposculpture of the face, neck, and jowls with laser dermal resurfacing and platysmal plication. Dermatol Clin. 1999;17(4):773-82.
17. Blugerman G. Laserlipolisys for the treatment of localized adiposity and "cellulite". Abstracts of the World Congress on Liposuction Surgery - 2000. Dearborn, Michigan, USA.
18. Schavelzon D, Blugerman G, Goldman A. Laser lipolysis. Abstracts of the 10th International Symposium on Cosmetic Laser Surgery - 2001. Las Vegas, USA.
19. Neira R. Laser Lipolysis. Lipoplastia asistida con laser. Anais do Congreso Colombiano de Cirugía Plástica - 2001. Cali, Colômbia.
20. Neira R. Reportaje clínico de 700 pacientes practicados con técnica lipoescultura laser. Anais do Congreso Colombiano de Cirugía Plástica - 2001. Cali, Colômbia.
21. Neira R, Zúñiga E. Niveles sanguíneos de lidocaína y variables hemodinámicas en lipoescultura laser. Anais do Congreso Colombiano de Cirugía Plástica - 2001. Cali, Colômbia.
22. Neira R, Isaza C. Efectos del laser de díodo eléctrico en adipositos humanos cultivados in vitro. Anais do Congreso Colombiano de Cirugía Plástica - 2001. Cali, Colômbia.
23. Goldman A, Schavelzon D, Blugerman G. Laser lipolysis: liposuction using Nd:YAG laser. Rev Soc Bras Cir Plást. 2002;17(1):17-26.
24. Goldman A, Schavelzon D, Blugerman G. Liposuction using neodymium: Yttrium-aluminium-garnet laser. Plast Reconstr Surg. 2003;111(7):2497.
25. Badin A, Moraes L, Godek L, Chiaratti MG, Canta L. Laser lipolysis: flaccidity under control. Aesthetic Plast Surg. 2002;26(5):335-59.
26. Nahai F. Positioning for ultrasound-assisted lipoplasty. Clin Plast Surg. 1999;26:235-43.
27. Rao RB, Ely SF, Hoffman RS. Deaths related to liposuction. N Engl J Med. 1999;340:1471-5.
28. Nahas FX, Barbosa MVJ, Ferreira LM. Liposculpture. In: Guyuron B, Eriksson E, Persing JA, Chung KC, Disa J, Gosain A, et al., eds. Plastic surgery: indications and practice. New York: Saunders; 2009. p. 1603.
29. Zochi M. Ultrasonic liposculpturing. Aesth Plast Surg. 1992;16:287-98.
30. Bruno G, Amadei F, Abbiati G. Liposculpture with ultrasound: biomedical considerations. Aesth Plast Surg. 1998;22:401-3.
31. Grippaudo FR, Matarese RM, Macone A, Mazzocchi M, Scuderi N. Effects of traditional and ultrasonic liposuction on adipose tissue: a biochemical approach. Plast Reconstr Surg. 2000;106:197-9.
32. Wilkinson TS. External ultrasound-assisted lipoplasty. Aesth Surg. 1999;19:124-9.
33. Zocchi ML. Basic physics for ultrasound-assisted lipoplasty. Clin Plast Surg. 1999;26:209-20.
34. Gingrass M, Kenkel J. Comparing ultrasound-assisted lipoplasty with suction-assisted lipoplasty. Clin Plast Surg. 1999;26:283-8.
35. Mateo M, Pérez V. Systematic procedure for ultrasonically assisted lipoplasty. Aesth Plast Surg. 2000;24:259-69.
36. Badin AZ, Gondek LB, Garcia MJ, Valle LC, Flizikowski FB, de Noronha L. Analysis of laser lipolysis effects on human tissue samples obtained from liposuction. Aesthetic Plast Surg. 2005;29(4):281-6. Epub 2005 Jul 19.
37. Rohrich R, Beran SJ, Fodor PB. The role of subcutaneous infiltration in suction-assisted lipoplasty: a review. Plast Reconstr Surg. 1997;99:514-9.
38. Wong L, Vasconez HC. Patient satisfaction after Nd:YAG laser-assisted lipolysis. Ann Plast Surg. 2011;66(5):561.
39. Fournier P. Liposculpture. Ma technique. Paris: Arnette; 1989.
40. Fodor PB, Watson J. Wetting solutions in ultrasound-assisted lipoplasty. Clin Plast Surg. 1999;26:289-93.
41. Klein JA. The tumescent technique. Dermatol Clin. 1990;8:425.
42. Trelles MA, Mordon SR, Bonanad E, Moreno Moraga J, Heckmann A, Unglaub F, et al. Laser-assisted lipolysis in the treatment of gynecomastia: a prospective study in 28 patients. Lasers Med Sci. 2013;28(2):375-82.
43. Grotting J, Beckenstein M. The solid-probe technique in ultrasound-assisted lipoplasty. Clin Plast Surg. 1999;26:245-54.
44. Rohrich RJ, Beran SJ, Kenkel JM, Adams WP, Dispaltro F. Extending the role of liposuction in body contouring with ultrasound-assisted liposuction. Am Soc Aesth Plast Surg. 1988;101(4):1090-102.
45. Brow S, Rohrich R, Kenkel J, Young VL, Hoopman J, Coimbra M. Effect of low-level laser therapy on abdominal adipocytes before lipoplasty procedures. Plast Reconstr Surg. 2004;113(6):1796-804.
46. Dang YY, Ren QS, Liu HX, Ma JB, Zhang JS. Comparison of histologic, biochemical, and mechanical properties of murine skin treated with the 1064-nm and 1320-nm Nd:YAG lasers. Exp Dermatol. 2005;14(12):876-82.
47. Goldman A, Gotkin RH. Laser-assisted liposuction. Clin Plastic Surg. 2009;36:241-53.
48. Goldman A, Gotkin RH, Sarnoff DS, Prati C, Rossato F. Cellulite: a new treatment approach combining subdermal Nd:YAG laser lipolysis and autologous fat transplantation. Aesthetic Surg J. 2008;28(6):656-62.
49. Goldman A, Wollina U, de Mundstock EC. Evaluation of Tissue Tightening by the Subdermal Nd:YAG Laser-Assisted Liposuction Versus Liposuction Alone. J Cutan Aesthet Surg. 2011;4(2):122-8.
50. Chia CT, Theodorou SJ. 1,000 consecutive cases of laser-assisted liposuction and suction-assisted lipectomy managed with local anesthesia. Aesthetic Plast Surg. 2012;36(4):795-802.
Full Member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery - SBCP), American Society for Aesthetic Plastic Surgery, and International Society of Aesthetic Plastic Surgery, Plastic Surgeon at Hospital Israelita Albert Einstein, São Paulo, SP, Brazil
Correspondence to:
Alexandre Braga Senra
Rua Joaquim Floriano, 413 - 4º andar - Itaim
São Paulo, SP, Brazil - CEP 04534-011
E-mail: clinic@alexandresenra.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: 25/7/2012
Article accepted: 15/12/2013
This work was performed at the author's private clinic, São Paulo, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter