

Ideas and Innovation - Year 2013 - Volume 28 -
Use of three rhomboid flaps for scalp defect coverage
Retalho romboide triplo para fechamento de defeitos em couro cabeludo
ABSTRACT
Full-thickness scalp defects exposing the skull can be challenging for plastic surgeons. Scalp skin has low elasticity, so a large flap is necessary to cover even a small defect. This article presents 9 cases in which 3 rhomboid flaps were used for the closure of scalp defects. One patient experienced flap necrosis and required reoperation. Two other patients had minor complications treated with dressing. The method presented herein allows the harvest of 3 small flaps that collectively cover the defect as well as the primary closure of the donor area. This technique does not require the creation of a large flap or skin graft from the donor. Thus, the technique described herein is suitable for medium-thickness scalp defects and is a good alternative to large rotation flaps and skin grafts.
Keywords: Scalp/surgery. Scalp/injuries. Surgical flaps.
RESUMO
Defeitos no couro cabeludo podem ser um desafio para os cirurgiões plásticos quando afetam sua espessura total e deixam o crânio exposto. O couro cabeludo tem pouca elasticidade, assim um grande retalho é necessário para cobrir um defeito pequeno. O objetivo deste artigo é apresentar 9 casos em que 3 retalhos romboides foram utilizados para o fechamento de defeitos no couro cabeludo. Um paciente apresentou necrose do retalho e foi necessária reoperação. Dois outros pacientes tiveram complicações menores, que foram tratadas com curativos. O método apresentado permite a confecção de 3 pequenos retalhos que em conjunto cobrem o defeito, e as áreas doadoras são fechadas primariamente. Com a utilização da técnica descrita, a confecção de um retalho grande e a enxertia de pele da área doadora não são necessárias. Neste artigo é descrita uma técnica para fechamento de defeitos de tamanho moderado no couro cabeludo, que é uma boa alternativa a grandes retalhos de rotação ou enxerto de pele.
Palavras-chave: Couro cabeludo/cirurgia. Couro cabeludo/lesões. Retalhos cirúrgicos.
Scalp defects affecting the full thickness of the scalp and/or exposing the skull can be challenging for plastic surgeons. Although a series of algorithms exists for the treatment of such defects1,2 that share the same principles, none are widely accepted by surgeons.
Small defects (< 2 or 10 cm2 depending on the algorithm) can be primarily closed, whereas larger defects require more sophisticated closure techniques1.
Cases involving medium defects (i.e., 2-25 or 10-50 cm2) usually require a local flap1,2. Because of the low elasticity of the scalp skin, a large flap must be produced to cover even a small defect (Figure 1).
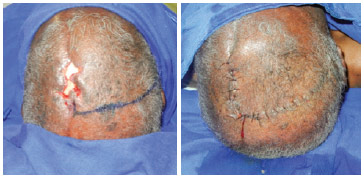
Figure 1 - Traditional flap. A large flap is required to cover a small defect.
Larger defects must be reconstructed through a combination of axial flaps and free flaps or with the use of a skin graft1,2.
Rhomboid flaps are very useful for defects on several body parts3. However, rhomboid flaps are not a viable option for the correction of scalp defects3, because it is impossible to primarily close the donor area; therefore, the donor graft would lead to a new defect without pilous follicles.
Here, we report 9 cases treated with a technique consisting of 3 rhomboid flaps for the closure of full-thickness scalp defects.
METHODS
The surgical technique described herein was performed on 9 patients; 2 illustrative cases are presented as examples.
Case 1
The patient was 73 years old and had a squamous cell carcinoma that was resected, resulting in a defect approximately 5 cm in diameter (Figure 2). The defect was divided into thirds with a "Y" mark with 120º angles. Three rhomboid flaps were demarcated and raised for the closure of the defect. The defect and flap donor areas were subsequently closed.
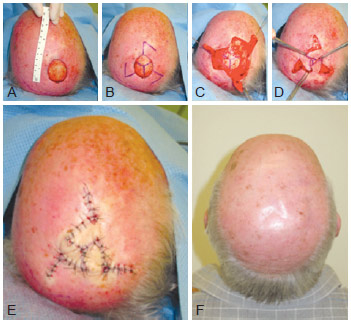
Figure 2 - Patient 1. In A, B, C, and D, intraoperative appearance of the correction of the scalp defect after resection of squamous cell carcinoma. In E, appearance immediately after surgery. In F, appearance 1 year postoperatively.
Case 3
The patient was 81 years old and had a 3.5 × 3.5-cm defect, formed after the resection of a scalp fibroxanthoma. Figure 3 shows the flap marking as well as the scalp appearance at 10 days and 2 months postoperatively.

Figure 3 - Patient 3. In A, flap marking for the correction of a scalp defect following fibroxanthoma resection. In B, appearance 10 days postoperatively. In C, appearance 2 months postoperatively.
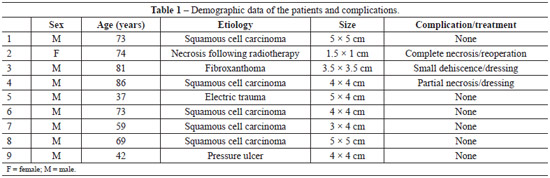
One patient had flap necrosis and required reoperation. Two other patients had minor complications treated with dressing. Table 1 summarizes the patients' demographic data and complications. All patients were followed for at least 2 months.
DISCUSSION
Full-thickness scalp defects exposing the skull can have various etiologies including tumor resection, burns, electric or mechanical traumas, radiotherapy-induced necrosis, etc.1,2,5.
Depending on their size, such defects can be treated with free flaps6, perforation or removal of the external layer for granulation and grafting7, or even with dermic substitutes8. Free flaps are associated with complex surgeries and consequently a risk of death. Furthermore, the wait for granulation and grafting can be weeks, and dermic substitutes are expensive. In addition, all of these closure methods induce alopecia in the reconstructed area. Therefore, local flaps are preferable9.
Moreover, the low elasticity of the tissue hardens the primary closure of the flap donor areas. Therefore, large rotation flaps or skin grafts should be considered.
The method described herein allows the elaboration of 3 smaller flaps that collectively cover the defect, allowing the primary closure of the donor areas. Demir et al.10 report a similar procedure using the V-Y-S technique.
This technique avoids the need to make a large flap and graft.
In conclusion, the technique described herein for closing medium scalp defects is a good alternative to large rotation flaps and skin grafts
REFERENCES
1. Leedy JE, Janis JE, Rohrich RJ. Reconstruction of acquired scalp defects: an algorithmic approach. Plast Reconstr Surg. 2005;116(4):54e-72e.
2. Newman MI, Hanasono MM, Disa JJ, Cordeiro PG, Mehrara BJ. Scalp reconstruction: a 15 year experience. Ann Plast Surg. 2004;52(5):501-6.
3. Alvarez GS, Laitano FF, Siqueira EJ, Oliveira MP, Martins PDE. Aplicações do retalho romboide em reparações cutâneas. Rev Bras Cir Plást. 2012;27(1):102-7.
4. Ahuja RB. Geometric considerations in the design of rotation flaps in the scalp and forehead region. Plast Reconstr Surg. 1988;81(6):900-6.
5. Dalay C, Kesiktas E, Yavuz M, Ozerdem G, Acarturk S. Coverage of scalp defects following contact electrical burns to the head: a clinical series. Burns. 2006;32(2):201-7.
6. Chang KP, Lai CH, Chang CH, Lin CL, Lai CS, Lin SD. Free flap options for reconstruction of complicated scalp and calvarial defects: report of a series of cases and literature review. Microsurgery. 2010;30(1):13-8.
7. Muhlstadt M, Thome C, Kunte C. Rapid wound healing of scalp wounds devoid of periosteum with milling of the outer table and split-thickness skin grafting. Br J Dermatol. 2012;167(2):343-7.
8. Corradino B, Di Lorenzo S, Leto Barone AA, Maresi E, Moschella F. Reconstruction of full thickness scalp defects after tumour excision in elderly patients: our experience with Integra dermal regeneration template. J Plast Reconstr Aesthet Surg. 2010;63(3):e245-7.
9. Blackwell KE, Rawnsley JD. Aesthetic considerations in scalp reconstruction. Facial Plast Surg. 2008;24(1):11-21.
10. Demir Z, Velidedeoglu H, Celebioglu S. V-Y-S plasty for scalp defects. Plast Reconstr Surg. 2003;112(4):1054-8.
1. Plastic Surgeon, Associate Member of the Brazilian Society of Plastic Surgery (Sociedade Brasileira de Cirurgia Plástica, SBCP), Preceptor MD at the Hospital das Clínicas, Faculty of Medicine of the University of São Paulo (HCFMUSP), São Paulo, SP, Brazil
2. Plastic Surgeon, Associate Member of the SBCP, Assistant MD of the Institute of Cancer of the State of São Paulo (Instituto do Câncer do Estado de São Paulo, ICESP) and the Plastic Surgery Service of the Hospital do Servidor Público Estadual of São Paulo (HSPE-SP), São Paulo, SP, Brazil
3. Resident MD in Plastic Surgery of the HSPE-SP, Trainee and Aspiring Member of the SBCP, São Paulo, SP, Brazil
4. Resident MD in General Surgery of the HSPE-SP, São Paulo, SP, Brazil
5. Plastic Surgeon, PhD, Titular Member of the SBCP, Assistant MD of the ICESP, HCFMUSP and HSPE-SP, São Paulo, SP, Brazil
6. Titular Professor of Plastic Surgery of the Faculty of Medicine of the University of São Paulo, Titular Member of the SBCP, Director of the Division of Plastic Surgery and Burns of the HCFMUSP, São Paulo, SP, Brazil
7. Titular Member of the SBCP, Director of the Service of Plastic Surgery of the HSPE-SP, São Paulo, SP, Brazil
Correspondence to:
Lincoln Saito Millan
Av. Dr. Enéas de Carvalho Aguiar, 255 - 8o andar - sala 8128 - Cerqueira Cesar
São Paulo, SP, Brazil - CEP 05403-900
E-mail: lincolnsaito@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: 28/8/2012
Article accepted: 20/11/2012
Work performed in the Hospital das Clínicas, Faculty of Medicine of the University of São Paulo - Henri Friedhofer, São Paulo, SP, Brazil


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter