

Reviw Article - Year 2013 - Volume 28 -
Body dysmorphic disorder: contributions for the plastic surgeon
Transtorno dismórfico corporal: contribuições para o cirurgião plástico
ABSTRACT
Body dysmorphic disorder (BDD) is a psychiatric condition often encountered by plastic surgeons in daily clinical practice. BDD is a body image disorder that causes patients to become preoccupied with small or imagined defects in appearance, which lead to the development of social and occupational disabilities. Individuals with BDD exhibit fears of their "defects" being noticed by others, and feel ashamed, embarrassed, and uncomfortable when physically exposed during social activities. They have delusional thoughts, develop compulsive rituals and somatic preoccupation, seek cosmetic treatments, and refuse psychological intervention. Patients with BDD are convinced that improving physical appearance alone will improve their self-esteem. These patients often undergo cosmetic surgery or other related procedures to correct their "defective" image, often consulting several health professionals, especially plastic surgeons, before finding one who will perform their desired procedure. However, surgery does not resolve these imperfections; on the contrary, the results are often poor and can cause the patient to develop violent behavior toward the surgeon and worsen the patient's condition. The aim of this review was to describe BDD and its progression and treatment, and to make recommendations that will assist plastic surgeons and facilitate diagnosis and patient management in daily clinical practice, thereby allowing patients to understand the psychogenic origin of most preoccupations with appearance and the importance of undergoing psychological/psychiatric treatment. As a result, unnecessary aesthetic procedures can be avoided.
Keywords: Plastic surgery. Body image. Body dysmorphic disorders. Somatoform disorders.
RESUMO
O transtorno dismórfico corporal (TDC) é uma doença psiquiátrica que pode ser encontrada com frequência no consultório do cirurgião plástico. Trata-se de uma desordem da imagem corporal, incapacitante social e profissionalmente, em que a pessoa tem preocupações decorrentes de defeitos mínimos ou inexistentes na aparência. Indivíduos com TDC apresentam medo de terem seus "defeitos" percebidos, sentem vergonha, embaraço e desconforto ao se exporem fisicamente em atividades sociais, têm pensamentos de desilusão e desenvolvem rituais compulsivos, preocupações somáticas, busca por tratamentos cosméticos e resistência a intervenções psicológicas. Os pacientes com TDC estão convencidos de que a única maneira de melhorar sua autoestima é aperfeiçoando sua aparência. Frequentemente esses pacientes buscam a cirurgia cosmética ou outros procedimentos relacionados para melhorar seu aspecto "defeituoso", e podem consultar vários médicos, especialmente cirurgiões plásticos, até encontrarem um profissional que realizará o procedimento desejado. No entanto, a cirurgia não cura essas imperfeições, muito pelo contrário, tem resultados pobres e pode gerar violência do paciente contra o cirurgião e piora de suas condições. O propósito desta revisão é descrever a patologia do TDC, seu desenvolvimento e tratamento, e sugerir algumas recomendações aos cirurgiões plásticos para sua prática diária, a fim de facilitar o diagnóstico do transtorno e o manuseio do paciente, contribuindo para que o portador da desordem perceba a origem psíquica da maioria de suas preocupações com a aparência e aceite se submeter a um tratamento psicológico/psiquiátrico, evitando assim o procedimento estético desnecessário.
Palavras-chave: Cirurgia plástica. Imagem corporal. Transtornos dismórficos corporais. Transtornos somatoformes.
Dissatisfaction with body image is common because of the cultural trends in society that attribute increasing importance to physical beauty, youth, and health. However, some people develop excessive preoccupation with their appearance, which causes significant distress and disability.
Although the outcomes of aesthetic surgery can improve self-esteem by correcting an undesirable physical aspect, they do not solve emotional problems or imaginary defects associated with a psychological disorder. In such cases, patients seek aesthetic surgical intervention not because they are unhappy with their body image but because a psychiatric condition called body dysmorphic disorder (BDD) compels them to do so.
BODY DYSMORPHIC DISORDER
Although BDD is often overlooked by plastic surgeons, it has been described for more than a century and reported worldwide1,2. It is one of the most common psychiatric diseases among individuals who seek plastic surgical treatments3.
Many attempts have been made to conceptualize pathological manifestations associated with physical appearance4. Dysmorphophobia, the original term for BDD, was first described in 1886 by Enrico Morselli in Genova, Italy, as the fear of ugliness1,5. In 1903 in Paris, France, Janet described it as "l'obsession de honte du corps" (obsession with shame of the body). In 1909, in Munich, Germany, Kraeplin called it "dysmorphophobic syndrome," and Japanese researchers named it shubo-kyofu1,6.
From an etymological perspective, the term dysmorphophobia is derived from the Greek word dysmorphia, which means "ugliness," particularly with respect to the face. However, the disorder is not simply characterized by the fear of having a physical flaw, as the suffix phobia might suggest. Moreover, patients manifest polarized attention (at an emotional cost) that focuses on a specific part of the body. The individual develops repulsion for that part of the body, which interferes to a varying degree with their relationships and social functioning7.
The first report in the English literature about dysmorphophobia was published only in 1970, and the essence of the disorder was described not as a fear of becoming ugly or deformed but as an irrational belief of having become abnormal, alongside the fear of other people's reactions6,8.
Although BDD was first described more than a century ago, it was not included in the diagnostic systems4 until 1980. For a long time, it was considered a symptom of psychiatric diseases such as schizophrenia, and mood or personality disorders6.
In 1987, the suffix phobia was withdrawn and the condition was described as a distinct psychiatric disorder. It was included in the Diagnostic and Statistical Manual of Mental Disorders9 as "body dysmorphic disorder," a manifestation of somatoform disorders wherein the pathological mechanism revolves around a preoccupation with a physical symptom, solely of psychogenic origin10-12.
CAUSES OF BDD
Knowing the causes of BDD contributes to its understanding, diagnosis, and differentiation from other mental disorders.
Genetic factors are among the main causes of BDD; 8% of individuals with BDD have a family member with long-term BDD, a prevalence that is 4-8 times higher than that in the general population2. BDD shares heredity with obsessive-compulsive disorder (OCD), as was shown in a family study conducted by Feusner et al.13 in which 7% of patients with BDD had a first-degree relative with OCD.
As with other OCDs, BDD is the result of a neurochemical imbalance that principally involves serotonin. This molecule acts physiologically by keeping ideas and thoughts under control14. Lesions in specific regions of the brain can cause dysfunction in many brain connectivity networks and alter the circuit function related to the pathophysiological mechanism of BDD, thus resulting in BDD symptoms and neurocognitive deficits13. Studies using structural and functional neuroimaging in individuals with BDD have suggested an asymmetry in the caudate nucleus and a higher proportion of white matter in the BDD group than in the control group15,16. However, case reports have indicated that BDD can also be triggered by inflammatory diseases caused by frontotemporal lobe damage16 or streptococcal infections, which can exacerbate symptoms17.
The psychoanalytic theory suggests that BDD is more likely to occur in individuals who are anxious, perfectionists, and distressed18. In addition, certain life experiences can create susceptible personalities with low self-esteem, insecurity, introversion, difficulty with interpersonal relationships, schizoid traits (individuals with a tendency for solitude, unsociability, introspection, and maladaptation to the social environment), neurotic traits (individuals with one or more types of emotional disorder, with anxiety being the main characteristic, and no significant distortion of reality or personality disorder), neuroses, obsessions, critical and strict parents, or childhood trauma10,19.
CLINICAL CHARACTERISTICS OF BDD
Preoccupation with Appearance
The main characteristic of BDD is "preoccupation with an imagined defect in physical appearance. If a minor physical anomaly is present, the individual's concern is markedly excessive"9.
Unlike any normal concern with appearance, preoccupation in BDD consumes all of the individual's time and causes significant distress or embarrassment in social situations6,10,20.
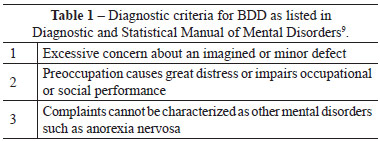
The criteria for the diagnosis of BDD listed in the Diagnostic and Statistical Manual of Mental Disorders9 are the following: excessive focus on an imagined or minor defect; profound sadness or impaired performance of occupational or social activities; and no other psychiatric disorders (Table 1).
From a theoretical perspective, patients with BDD can be distressed by any aspect of their physical appearance, even if they look normal. Some patients report vague complaints of ugliness, deformities, or strange appearance but cannot specify the nature of the defect10,20. On the contrary, some patients complain about physical characteristics or minor defects such as a large nose, asymmetrical mouth, thin or thick lips, thin hair, uneven excessively thick or thin eyebrows, acne, and scars20. However, other parts of the body can also be the focus of preoccupation, such as the breasts, buttocks, legs, hips, or even the overall size of the body or a part of the body, such as a small penis7,18,19,21.
Whereas male patients focus their anxiety on genitals, height, muscles, or excessive body hair, women mainly worry about the face, breasts, hips, and legs22. Although the main characteristic of BDD is the belief in the existence or severity of a physical defect, this distorted perception is only the first of many in a sequence of events associated with this disorder.
Cognitive and Emotional Characteristics
In general, patients with BDD use negative language to describe their appearance. Unlike normal self-perception of physical appearance, BDD involves preoccupation that is time consuming, causes suffering, and impairs occupational and social performances10,18,20,21,23,24. Although this may happen at any moment of the day, preoccupation with appearance is particularly intense in social situations, in which BDD patients feel uncomfortable and expect to be judged by other people at any moment3,20,25.
Most patients have delusions of reference; that is, they believe that other people may notice their supposed "defect" and make some kind of disparaging or mocking comment10,20,21,24. This delusion of reference leads to a state of mind that allows patients to feel anxious, embarrassed, and deeply ashamed because they believe that the "defect" will reveal some personal imperfection. This preoccupation can worsen to a point at which patients not only feel embarrassed by their unattractiveness but also afraid of disgusting and offending others14.
Some BDD patients become aggressive when they are prevented from engaging in their behavior or in stressful situations6. Suicidal thoughts are observed in 55-71% of patients with severe BDD5,10,18,24,25. Approximately 24-28% of patients with BDD attempt suicide, a rate higher than that associated with other mental disorders10,21,24,26.
Compulsive Behaviors
Although compulsive behaviors are not included in the diagnostic criteria of BDD, almost all patients with BDD exhibit one or more repetitive, compulsive, and/or time-consuming behavior21,24.
These behaviors are intended to check, improve, or hide the "defect"20. Dysfunctional body self-consciousness can make the individual spend a great amount of time in front of mirrors and other reflective surfaces such as car bumpers and the back of spoons, contemplating their reflection and focusing mainly on the perceived "defect"6,7,10,20.
In addition to checking the "defect" in the mirror, several types of body-checking behavior are common, such as washing and brushing the hair repeatedly for hours throughout the day, comparing one's appearance with that of other people, and constantly asking other people about the appearance of their "defect" for reassurance. As with a compulsion, these behaviors are difficult to resist and, in some extreme cases, can result in many wasted hours per day3,10,19-21,25.
Many patients with BDD avoid social activities because they believe that people will notice their "defect"20. A few patients shy away from social interaction, isolate themselves at home, and only going out at night, if necessary, to avoid public exposure4,6,7,25.
However, most patients van at least maintain a restricted social and professional life by camouflaging themselves to limit exposure of their features to the public, such as by wearing concealing clothes, makeup, dark glasses, hairstyles, or changing their body posture or movements to hide the "defect"4,10. Camouflaging with clothes or movements is a classic compensatory behavior in patients with real or exaggerated deformities6,20.
Some behaviors such as skin or hair touching appear to be important in BDD6. These behaviors are complex and become pathological (pathological excoriations or trichotillomania), depending on their focus and the duration and extent of the resulting problems. In some cases, individuals severely burn their skin from excessive sun tanning to avoid looking pale7,10. Although these behaviors are considered self-destructive, patients with BDD do not mean to injure themselves, but try to improve their skin appearance7,10,19,26.
It is worth noting that in many cases of BDD patients who seek reassurance from others regarding their physical appearance20, this behavior could create tension in marriage and family relationships because it places great pressure on those the individuals who are close to them; more than 70% of patients do not marry3,6,25.
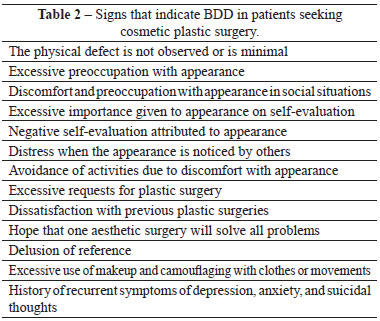
Another significantly important aspect of BDD is that individuals engage in activities such as skin or hair beauty treatments, weight loss, dental treatments, and cosmetic surgery because they believe that improving their physical appearance will also improve their self-esteem4,10,20,21,25. Regarding the latter, because the abnormality does not exist in some cases, patients remain unhappy with their appearance even after undergoing aesthetic surgical procedures. Individuals with BDD often visit several healthcare professionals, particularly plastic surgeons, even if correcting the supposed defects is impossible5. Table 2 shows a list of signs that indicate BDD in patients seeking cosmetic plastic surgery.
Demographic Characteristics
An estimated, 1-3% of the general population has BDD7,25. In the context of plastic surgery, this disorder has a higher prevalence among patients who seek plastic surgery than among the general population, with 7-15% of the patients who seek plastic surgery being diagnosed with BDD5,10,13.
BDD is a disease that usually presents during adolescence, when individuals are more preoccupied with self-image and their social lives, although its manifestation during childhood has also been reported10,25,27. The mean age of onset is 17 years, and the duration from onset to seeking specific treatment is up to 11 years4,10,18. A second incidence peak has been observed in women during menopause4,22.
There appears to be no difference between sexes, although this has not been definitely established3. Some studies have shown a higher frequency among women3,18, whereas other studies have demonstrated the opposite6,7,18. However, men and women share similarities with regard to most clinical and demographic aspects11,18,21,28.
Disease Progression
The onset is gradual, and in the beginning, patients may exhibit acceptable preoccupations with their appearance. The initial crisis can be suddenly triggered by a traumatic event such as changing residence to a distant location that entails a change in social life or the ending of a stable relationship13,20,25.
Spontaneous remission is rare. Psychotherapy can result in improvement, unlike surgical interventions, which often exacerbates symptoms7,18,25. The disease is chronic, with varying degrees of severity24,26.
DIFFERENTIAL DIAGNOSIS
BDD is classified as a somatoform disorder9. The illness is essentially a preoccupation with a physical symptom solely of psychogenic origin12. However, this classification remains controversial because many specialists currently argue that BDD should be considered a disorder of the obsessive-compulsive or affective spectrum24,28. Patients with somatoform disorders often seek complex treatments that result in long medical and surgical histories9,10.
BDD substantially overlaps with hypochondria. Both diseases involve a body defect that is disproportionately perceived and not the result of an organic abnormality. In both diseases, thoughts about the defect cause anxiety, which the patient tries to alleviate by seeking reassurance from other people and constantly checking the defect. Individuals with BDD constantly engage in beauty treatments, whereas hypochondriacs overuse medical services in search of a diagnosis or cure6,7,23.
Some characteristics of BDD are similar to those of OCD. Comorbidity between BDD and OCD exists in 12-15% of cases2,7,12,25. The difference between these patients is that individuals with BDD exhibit an obsession and compulsion with their appearance, whereas those with OCD are obsessive-compulsive with unacceptable orders or impulses6,23,24.
Eating disorders are relatively common in individuals with BDD7. Although dissatisfaction with weight and body shape is frequent, BDD is only diagnosed if the defect is imagined or exaggeratedly perceived and accompanied by debilitating preoccupation and distress. Preoccupation with weight and body shape in the course of bulimia or anorexia is not diagnosed separately as BDD6,10,24.
Patients with social phobia and those with BDD share similarities; they have profound feelings of shame and embarrassment, and are afraid of looking strange or silly to others and thus avoid situations that may draw attention to their imperfection5,7,19.
These comparisons with other disorders are useful because BDD is not well understood. However, OCDs, social phobias, eating disorders, and hypochondria do not have the essential component of BDD as a body image disorder4,7,10,24.
TREATMENT
Cosmetic Surgery
A typical BDD patient does not seek a psychotherapist or a psychiatrist but rather a plastic surgeon, because the patient is pathologically fixated on the belief that the physical defect is a real problem6. As such, cosmetic surgery to improve body image is likely to fail because of the absence of a real deformity and the fact that it cannot resolve worries that keep changing with appearance.
The most frequent recommendation is not to perform surgery on patients with BDD5. The result is usually not very productive20 and leaves the patient unhappy, which may lead to feelings of anger and even violence toward the surgeon18. In >80% of cases, the individual's psychological situation will be destabilized by the surgery or the patient will find new imperfections25.
Three groups of individuals seek aesthetic surgical treatments. The first group includes patients without deformities and have unrealistic expectations. These individuals are easily identified, and the diagnosis of BDD should be considered. In these cases, patients should be guided to understand that emotional factors may be interfering with their perception of their own bodies and could be the cause of their dissatisfaction and distress. This understanding is necessary to motivate patients to accept help from a mental health professional20.
The opposite group is composed of individuals with treatable deformities and realistic expectations and who are also easily identifiable. Surgical correction should be offered in such cases.
The greatest difficulty is to deal with an intermediate group of patients with minimal and treatable deformities who, however, exhibit inappropriate behavior and expectations3. In these individuals, feelings such as excessive sadness and worry over physical appearance do not necessarily indicate pathological behavioral changes. These symptoms are inherently subjective and can interfere with the diagnosis of BDD. These patients may exhibit subclinical BDD characteristics that mask a diagnosis of BDD3,4,6,7,28. These are true challenges from a surgical point of view. Plastic surgeons have to decide whether there is an indication for surgery and should be extremely critical about agreeing to operate on these patients. These candidates for aesthetic surgery must have the surgical indication reevaluated at least once during the preoperative period.
A second consultation is advisable, especially for those seeking secondary rhinoplasty, a type of surgery that is common among patients with BDD25. The surgeon may consider the requested surgical correction only if the patient exhibits the necessary behavior during the second clinical assessment. It is recommended that these patients receive intense psychological support20.
Pharmacotherapy
The most promising pharmacotherapy appears to be the use of serotonin reuptake inhibitors such as clomipramine and fluoxetine. These are the most commonly used antidepressants and the optimal treatment for anxiety, panic attacks, obsessive-compulsive behavior, and eating disorders4,7,10,19-21.
Serotonin reuptake inhibitors are particularly effective because they reduce obsessive thoughts (e.g., "I cannot stop thinking about my horrible acne"), compulsive behavior (e.g., looking in the mirror and camouflaging), and depression21,23,25.
Patients frequently worry that medication may alter their personality and turn them into "zombies." However, those whose conditions have improved with the use of serotonin reuptake inhibitors state that they feel like themselves again (i.e., the way they used to be or the way they would like to feel)6,7,25.
Psychotherapy
In general, psychological symptoms and self-esteem show some improvement with cognitive behavioral therapy (CBT)7,20,21,24,25. In this type of treatment, BDD is transformed by changing thoughts about physical appearance. Patients are discouraged to look for defects in their own body and encouraged to attach less importance to physical characteristics6,10. They are made to see their appearance improved by means of positive language, to minimize grooming or constant body checking behaviors, and to be able to look into mirrors and shop windows without seeing a distorted image7,18,20. Lastly, CBT encourages patients not to seek reassurances from others, encouraging them to accept compliments, and to face the social stigma when a real "defect" exists6. They will thus be dealing directly with distorted thoughts and cognitive errors; in addition, they will be replacing inappropriate behaviors with more acceptable behaviors6,10,18,20,21.
Other types of psychological therapy can be used, such as psychoanalysis, depending on the degree of psychological involvement and the social and relational limitations caused by BDD. Moreover, the patient's choice regarding mental health treatment and the availability of professionals trained to address this type of demand should be considered.
PRACTICAL RECOMMENDATIONS FOR PLASTIC SURGEONS
To allow the planning of a BDD treatment strategy with greater potential for success, the following aspects need to be discussed:
1. The importance of providing the patient with information on the disorder and guidance regarding the psychological signs and symptoms as a prophylactic addition to medication10,19,20:2. The importance of providing patients with information about the disorder and guidance regarding its signs and symptoms: In general, it is ineffective to try and dissuade patients from their preoccupations or make them stop or change their compulsive and emotional behaviors19,20.Individuals should be told that they appear to have a body image problem called BDD, which is a known and common disorder, and most importantly, that it is treatable. It is very important, at this point, not to underestimate or minimize the patient's preoccupations with appearance because their distress is real and can increase20. The patient should be encouraged to read informative materials about BDD, such as books for lay people or websites. Family should be included in the information provision and guidance activities about BDD. 3. The best option being to avoid aesthetic procedures10,19These individuals are convinced that their appearance is inadequate, and the surgeon's attempt to convince them otherwise is usually fruitless20, with the exception of a few patients who acknowledge that their perception of deformities is disproportionate or who think that their deformities are really not as bad as they imagine. In such cases, it is useful to stress that this view is correct. In general, it is more interesting to focus on the distress and/or on the low esteem caused by the problems with appearance than on the patient's appearance itself20. This approach may facilitate referral to a mental health professional. Another recommended strategy is to ask the patients what they think is the cause of their problems and to perform a clinical anamnesis that allows knowing them better. It is advisable to collect a detailed history and focus on the patients and not on their symptoms, and to offer them a chance to express their feelings. The disorder is often an escape from a situation of conflict or the result of the need to be cared for. Patients should be asked how the other organs of their body and personal and affective life are functioning, and what their leisure activities and sources of pleasure and distress are. This may help patients understand the need for psychological treatment. 4. Referring patients to psychiatric treatment19Although the scientific literature does not provide sufficient data on the results of surgical treatments in BDD and no one can predict how a patient will respond to a treatment, the available data suggest that these procedures are likely to fail and can even worsen the patient's condition1,5,7,10,18,20. In some cases, the treatments trigger psychoses, suicide, or violent behaviors25. It is recommended to tell patients that because they have BDD, there is a concern that they will not be happy with the outcome of surgery and that it may even worsen their distress20. It is also best to avoid trying to reassure the patient by performing small surgical procedures because this type of approach may be unsuccessful or even disastrous7. Instead of referring patients to another surgeon, the most sensible approach is to refer them to a psychiatrist to start pharmacotherapy25. Therefore, it is important to inform patients about the psychological symptoms. When health professionals listen to patient's emotional issues and identify some causes, they allow patients to understand that there are feelings attached to their symptoms. This approach is more likely to lead to the acceptance of the need for psychiatric treatment and psychotherapy. If the patients resist this referral because they believe that the problem is physical and not psychological, highlighting the potential of psychiatric treatment to reduce the symptoms may encourage them to consult a psychiatrist20. When patients choose psychotherapy over a drug-based treatment, it is advisable to refer them to a professional who is familiar with BDD, if possible. If the patient is severely depressed or has suicidal thoughts, pharmacotherapy with serotonin reuptake inhibitors is indicated10,20,26.
CONCLUSIONS
Although some degree of dissatisfaction with body image is common in many individuals, those with extreme unhappiness with their appearance may be experiencing a psychiatric disorder called BDD. This somatoform disorder has a long history, but only in recent years has systematic research contributed to better recognition and understanding of the illness. It is more common among individuals interested in cosmetic procedures than among the general population. Unfortunately, surgical or minimally invasive treatments do not provide a solution to the symptoms of the disorder; on the contrary, in some cases, these treatments trigger psychoses, suicide, or violent behavior toward the surgeon. For this reason, BDD is considered a contraindication to cosmetic surgery. Therefore, it is extremely important that plastic surgeons are trained to identify subclinical patients and patients with complaints that indicate the presence of BDD.
Plastic surgery clinics are privileged settings for the early identification of BDD, wherein professionals can and should contribute to reduce the distress of these patients by helping them understand that their unhappiness with their bodies is of a psychogenic, not physical, nature. Meanwhile, recognizing BDD prevents unnecessary plastic surgery and problems that may result from these procedures, both for patients (worse body image) and surgeons (patients' violent behavior toward them).
REFERENCES
1. Morselli E, Jerome L. Dysmorphophobia and taphephobia: two hitherto undescribed forms of insanity with fixed ideas. Hist Psychiatry. 2001;12(45):103-7.
2. Bienvenu OJ, Samuels JF, Riddle MA, Hoehn-Saric R, Liang KY, Cullen BA, et al. The relationship of obsessive compulsive disorder to possible spectrum disorders: results from a family study. Biol Psychiatry. 2000;48(4):287-93.
3. Crerand CE, Franklin ME, Sarwer DB. Body dysmorphic disorder and cosmetic surgery. Plast Reconstr Surg. 2006;118(7):167e-80e.
4. Pavan C, Simonato P, Marini M, Mazzoleni F, Pavan L, Vindigni V. Psychopathologic aspects of body dysmorphic disorder: a literature review. Aesthetic Plast Surg. 2008;32(3):473-84.
5. Sarwer DB, Crerand CE, Didie ER. Body dysmorphic disorder in cosmetic surgery patients. Facial Plast Surg. 2003;19(1):7-18.
6. Rosen JC. The nature of boby dysmorphic disorder and treatment with cognitive behavior therapy. Cogn Behav Pract. 1995;2(1):143-66.
7. Conrado LA. Transtorno dismórfico corporal em dermatologia: diagnóstico, epidemiologia e aspectos clínicos. An Bras Dermatol. 2009;84(6):569-81.
8. Hay GG. Dysmorphophobia. Br J Psychiatry. 1970;116(533):399-406.
9. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington: American Psychiatric Association; 1994. p. 468.
10. Ross J, Gowers S. Body dysmorphic disorder. Adv Psychiatr Treat. 2011;17:142-9.
11. Phillips KA, Dufresne RG Jr, Wilkel CS, Vittorio CC. Rate of body dysmorphic disorder in dermatology patients. J Am Acad Dermatol. 2000;42(3):436-41.
12. Brunoni AR. Transtornos mentais comuns na prática clínica. Rev Med. 2008;87(4):251-63.
13. Feusner JD, Yaryura-Tobias J, Saxena S. The pathophysiology of body dysmorphic disorder. Body Image. 2008;5(1):3-12.
14. Slaughter JR, Sun AM. In pursuit of perfection: a primary care physician's guide to body dysmorphic disorder. Am Fam Physician. 1999;60(6):1738-42.
15. Rauch SL, Phillips KA, Segal E, Makris N, Shin LM, Whalen PJ, et al. A preliminary morphometric magnetic resonance imaging study of regional brain volumes in body dysmorphic disorder. Psychiatry Res. 2003;122(1):13-9.
16. Gabbay V, Asnis GM, Bello JA, Alonso CM, Serras SJ, O'Dowd MA. New onset of body dysmorphic disorder following frontotemporal lesion. Neurology. 2003;61(1):123-5.
17. Mathew SJ. PANDAS variant and body dysmorphic disorder. Am J Psychiatry. 2001;158(6):963.
18. Veale D. Advances in a cognitive behavioural model of body dysmorphic disorder. Body Image. 2004;1(1):113-25.
19. Buhlmann U, Marques LM, Wilhelm S. Traumatic experiences in individuals with body dysmorphic disorder. J Nerv Ment Dis. 2012;200(1):95-8.
20. Veale D. Cognitive-behavioural therapy for body dysmorphic disorder. Adv Psychiatr Treat. 2001;7:125-32.
21. Phillips KA. Suicidality in body dysmorphic disorder. Prim Psychiatry. 2007;14(12):58-66.
22. Perugi G, Akiskal HS, Gianotti D, Frare F, Di Vaio S, Cassano GB. Gender-related differences in body dysmorphic disorder (dysmorphophobia). J Nerv Ment Dis. 1997;185(9):578-82.
23. Simeon D, Hollander E, Stein DJ, Cohen L, Aronowitz B. Body dysmorphic disorder in the DSM-IV field trial for obsessive-compulsive disorder. Am J Psychiatry.1995;152(8):1207-9.
24. Phillips K, Kaye W. Relationship of body dysmorphic disorder and eating disorders to obsessive compulsive disorder. In: Hollander E, Zohar J, Sirovatka PJ, Regier DA, eds. Obsessive-compulsive spectrum disorders: refining the research agenda for DSM-V. Arlington: American Psychiatric Publishing; 2011. p. 33-56.
25. Jakubietz M, Jakubietz RJ, Kloss DF, Gruenert JJ. Body dysmorphic disorder: diagnosis and approach. Plast Reconstr Surg. 2007;119(6):1924-30.
26. Phillips KA. The presentation of body dysmorphic disorder in medical settings. Prim Psychiatry. 2006;13(7):51-9.
27. Albertini RS, Phillips KA. Thirty-three cases of body dysmorphic disorder in children and adolescents. J Am Acad Child Adolesc Psychiatry. 1999;38(4):453-9.
28. Altamura C, Paluello MM, Mundo E, Medda S, Mannu P. Clinical and subclinical body dysmorphic disorder. Eur Arch Psychiatry Clin Neurosci. 2001;251(3):105-8.
1. Master in Medical Sciences by the Universidade do Estado do Rio de Janeiro (Rio de Janeiro State University - UERJ), plastic surgeon at the Hospital Universitário Pedro Ernesto/UERJ (Pedro Ernesto University Hospital/UERJ), Rio de Janeiro, RJ, Brazil
2. Doctor of Medicine, adjunct professor at the Faculdade de Ciências Médicas da UERJ (Faculty of Medical Sciences of the UERJ), Rio de Janeiro, RJ, Brazil
3. Master in Plastic Surgery, Universidade de São Paulo (University of São Paulo), coordinator and professor of Plastic Surgery at the Faculdade de Ciências Médicas da UERJ (Faculty of Medical Sciences of the UERJ), Rio de Janeiro, RJ, Brazil
Correspondence to:
Maria Lídia de Abreu Silva
Rua Nossa Senhora de Lourdes, 65 - ap. 301 - Grajaú
Rio de Janeiro, RJ, Brazil - CEP 20540-370
E-mail: lidia7abreu@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: March 21, 2012
Article accepted: April 21, 2012
This study was performed at the Universidade do Estado do Rio de Janeiro (Rio de Janeiro State University), Rio de Janeiro, RJ, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter