

Original Article - Year 2013 - Volume 28 -
Lifting of the mons pubis after massive weigth loss
Lifting do púbis após grande perda ponderal
ABSTRACT
INTRODUCTION: This article describes the surgical planning, conducts pre and post operatively, results in the Lifting Pubic ex-obese patients submitted to gastroplasty or not, that feature large sagging skin and excess fat from the pubis.
METHOD: Two hundred and eighteen patients underwent surgery from May 2005 to August 2012. The pubic lifting was held in conjunction with the Anchor Adbominoplasty. The pubis was raised through points positioned 2-3 cm above its original position in the aponeurosis of the muscles rectus abdominis. Traction lines were directed from the center to up and the sides of the pubis and abdominal flaps were pulled to the midline of the abdomen No significant complication was observed, which could compromise the final result.
RESULTS: The elevation of the pubis, the correct shape and resection of excess adipocutâneos were achieved in all cases, bringing satisfaction to patients. Conclusion: Considering the pubic deformity after massive weight loss, and the results obtained, the procedures adopted proved to be safe, easily reproducible and stable over the long term.
Keywords: Pubic Bone/Surgery. Reconstructive Surgical Procedures. Obesity, Morbid. Surgical Flaps.
RESUMO
INTRODUÇÃO: O presente artigo descreve o planejamento cirúrgico, as condutas de pré e pós-operatório, e os resultados do lifting púbico em pacientes ex-obesos, submetidos ou não à Gastroplastia, que apresentavam grande flacidez cutânea e excesso adiposo do púbis.
MÉTODO: Duzentos e dezoito pacientes foram submetidos à cirurgia no período de maio de 2005 a agosto de 2012. O Lifting pubiano foi realizado conjuntamente com a Abdominoplastia em âncora. O púbis foi elevado por meio de pontos posicionados 2 a 3 cm acima de sua posição original, na aponeurose dos retos abdominais. Vetores de tração foram direcionados do centro do púbis para cima e para os flancos e os retalhos abdominais foram tracionados para a linha média do abdome. Nenhuma complicação significativa foi observada que pudesse comprometer o resultado final.
RESULTADOS: A elevação do púbis, a correção do formato e a ressecção, dos excessos adipocutâneos, foram alcançadas em todos os casos, trazendo satisfação aos pacientes.
CONCLUSÃO: Considerando-se a deformidade pubiana após grandes perdas ponderais e os resultados obtidos, os procedimentos adotados mostraram-se seguros, facilmente reproduzíveis e estáveis a longo prazo.
Palavras-chave: Púbis/Cirurgia. Procedimentos Cirúrgicos Reconstrutivos. Obesidade Mórbida.
Patients submitted to gastroplasty1 or strict dietary regimens exhibit significant body deformities after weight loss, such as ptosis of the mons pubis; this deformity presents as significant excess skin and increased adipose tissue as well as ptosis of both components, resulting in the loss of the body's natural shape (Fig. 1).

Figure 1 - Ptosis of the mons pubis after weight loss.
This deformity frequently disrupts patients' lives because of the exaggerated exposure of the pubis when wearing fitted clothing, resulting in difficulties in social and professional activities and intimate relationships. A few studies have focused on this anatomical region and the treatment of this condition2-4.
Other authors describe the treatment of the post-gastroplasty abdomen, but there are few references specifically regarding the treatment of the pubic area5-15. We defined the ideal shape of the mons pubis as a V shape or inverted delta shape with a moderate adipose cushion without scars (Fig. 2). Herein, we describe our routine for the treatment of this body deformity to achieve the idea shape.

Figure 2 - Natural shape of the mons pubis.
METHOD
A total of 218 patients underwent surgery, including 7 men and 211 women. Among them, 207 underwent Fobi-Capella gastroplasty via the open route; 11 achieved weight loss after a strict diet. The patients were photographed pre and postoperatively to evaluate and compare their body shapes. The patients exhibited a variety of mons pubis shapes. As mentioned above, we aimed to create an ideal V shape or inverted delta shape. The distances from the frenulum of the labia minora to the abdominal suprapubic fold (10-12 cm) and suprapubic abdominoplasty scar after lifting of the mons pubis (7-8 cm) were measured preoperatively.
All procedures strictly followed the department's protocol.
Preoperative procedure and department protocol
We adopted the following criteria for post-gastroplasty plastic surgery. Patients were only scheduled for plastic surgery after having been cleared by a multidisciplinary team including a bariatric surgeon, psychologist, nutritionist, endocrinologist, hematologist, and anesthesiologist.
Patients were required to have undergone gastroplasty at least 1 year previously, BMI < 30, stable weight for 6 months, and normal laboratory test results.
The laboratory assessment was thorough; complete blood count included EO. > 3,000, Hgb > 10, hematocrit > 30, albumin > 3, ferritin > 50, prothrombin > 70%, normal renal function, ECG. We did not perform surgery on patients who are known smokers because of the increased risk of necrosis in the extremities of the flaps.
Surgical technique
Marking of the resection of excessive adipocutaneous tissue and pubis elevation was performed in the perioperative period of abdominoplasty according to the observed excess tissue (Fig. 3A, B). The abdominal flap was pulled and fixated at the median of the abdomen. The mons pubis was pulled cranially and towards the sides. A line was marked in methylene blue to elevate the mons pubis 2-3 cm above its original position in the aponeurosis of the rectus abdominis (Fig. 4).
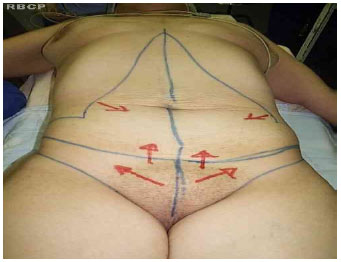
Figure 3 - Traction vectors of the abdominal flap and mons pubis.

Figure 4 - Marking of the resection of excess mons pubis tissue.
Inverted stitches were anchored in the aponeurosis of the rectus abdominis, and the pubis was fixated in a higher position, cranially and to the sides (Fig. 5). The target distance from the frenulum of the labia minora to the inferior abdominal scar was 7-8 cm (Figs. 6 and 7).

Figure 5 - Line of mons pubis suspension, 3 cm above the original position.

Figure 6 - Pubis elevated and fixated at the aponeurosis of the rectus abdominis.

Figure 7 - - Distance from the frenulum of the labia minora to the inferior abdominal scar.
In some cases, sagging of the mons pubis was so significant that additional V-shaped skin resection was necessary at the groin line. In cases presenting with significant excess adipose tissue, we performed liposuction to reduce the anteroposterior projection of the pubis. Surgical suturing was performed in 3 planes: depth, dermal, and cutaneous sutures were made using 3-0 monofilament nylon, 4-0 monofilament nylon, and 3-0 Monocryl, respectively. Vacuum suction and Penrose drains were used in all cases (Fig. 8). The wound was covered with antibiotic cream, and dressed with gauze and micropore tape. Peridural, rachidian, and general anesthesia were used in 191, 20, and 7 cases, respectively.

Figure 8 - Completed sutures and drainage.
Postoperative procedures
The following prophylactic antibiotic regimen was routinely adopted: cefazolin 2 g intraoperatively, which was continued for 2-3 days during hospitalization, followed by cephalexin 2 g/day for 5 days after hospital discharge. A vesical catheter was placed for 24 hours. Patients were allowed and encouraged to walk on the first day postoperatively. Vacuum suction drains were removed when daily flow was less than 50 mL, and Penrose drains were removed simultaneously. No anticoagulant agents were routinely used; however, they were indicated for cases at risk for PTE and DVT in accordance with current protocols. Dressings were changed daily during hospitalization and every 3 days after hospital discharge. Dressings were kept for 60 days, using only microporous tape.
Patients were advised to rest for 30 days and continue using compression bands or macaquinhos elásticos for up to 90 days. They were allowed to do more intense physical activity after 60 days.
RESULTS
The overall results were satisfactory: pubis deformities were corrected by fixating the mons pubis at a higher position as well as resecting the excess skin and adipose tissue. Improvements in pubic shape and its elevation relative to its original position were confirmed by comparing pre- and postoperative photographs. In addition, we compared the distance from the frenulum of the labia minora to the abdominoplasty inferior scar with its preoperative position. The mean pre and postoperative distances from the vulvar rim to the suprapubic fold were 10 and 7-8 cm, respectively.
The patients were satisfied with the final results (Figs. 9-15). Regarding complications related to the major surgery (i.e., anchor-shaped abdominoplasty), there were 25 cases of seroma; 5 cases of hypertrophy, scar enlargement, or keloid scar; 4 cases of partial necrosis of the abdominal flap extremity; and 4 cases of partial suture dehiscence (Fig. 16A, B). There were no infections.

Figure 9A - Preoperative appearance. Figure 9B - Preoperative appearance.

Figure 10A - Preoperative appearance. Figure 10B - Two-year postoperative appearance.

Figura 11A - Preoperative appearance. Figura 11B - Sixty-day postoperative appearance.
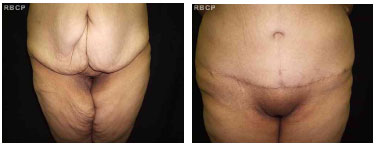
Figure 12A - Preoperative appearance. Figure 12B - One-year postoperative appearance.
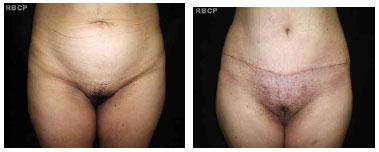
Figure 13A - Preoperative appearance. Figure 13B - Sixty-day postoperative appearance.

Figure 14A - Preoperative appearance. Figure 14B - Two-year postoperative appearance.

Figure 15A - Preoperative appearance. Figure 15B - Three-year postoperative appearance.

Figure 16A - Partial suture dehiscence. Figure 16B - Partial suture dehiscence.
DISCUSSION
Ptosis of the mons pubis is a common body deformity following gastroplasty and weight loss. Few articles have specifically addressed this topic with reference to the mons pubis2-4. Faced with patients' complaints, we developed a solution. After unsatisfactory results regarding the shape of the mons pubis with anchor-shaped abdominoplasty, we developed some modifications to the planning of anchor-shaped abdominoplasty that could help achieve an appearance of the pubis that was pleasing to the patients. The main changes are the traction vectors of the abdominal flap and mons pubis; these traction vectors should have opposite directions, and the pubis should be fixated at a higher position in the rectus abdominis. The traction vectors of the abdominal flaps and mons pubis should be towards the central portion of the abdomen and towards the head and the sides of the abdomen, respectively, thus forming a V shape or inverted delta shape. However, excess adipose tissue in the mons pubis sometimes required further refinements such as additional liposuction and/or resection of the skin excess in the lateral extremities of the pubis towards the inguinal fold. A second surgical procedure may be necessary to resect remaining excess tissue. However, it is inconvenient to perform vertical skin and adipose tissue resections in the central portion of the mons pubis.
CONCLUSION
The approach described herein successfully corrected the significant pubic deformities frequently exhibited by formerly obese patients. The technique achieved a satisfactory V shape or inverted delta shape of the pubis, with the reduction of excess skin and adipose tissue. Our technique proved to be safe, effective, easily reproducible, and long lasting.
REFERENCES
1. Capella JF, Capella RF. The weight reduction operation of choice: vertical banded gastroplasty or gastric bypass? Am J Surg. 1996;171(1):74-9.
2. Kaluf R, Araujo GAZ, Martins DL, Campos LCB, Magalhães RC, Santos Júnior AJ. Tratamento da região pubiana na abdominoplastia de pacientes após grande perda ponderal. Rev Bras Cir Plást. 2008;23(4):302-4.
3. Alter GJ. Management of the mons pubis and labia majora in the massive weight loss patient. Aesthet Surg J. 2009;29(5):432-42.
4. Nóbrega SS, Silva HLA. Rejuvenescimento da região pudenda, associada ou não à dermolipectomia abdominal. Rev Bras Cir Plast. 2009;24(3):351
5. Baroudi R, Ferreira CA. Seroma: how to avoid it and how to treat it. Aesthet Surg J. 1998;18(6):439-41.
6. Bozola AR, Psillakis JM. Abdominoplasty: a new concept and classification for treatment. Plast Reconstr Surg. 1988;82(6):983-93.
7. Soundararajan V, Hart NB, Royston CM. Abdominoplasty following vertical banded gastroplasty for morbid obesity. Br J Plast Surg.1995;48(6):423-7.
8. Pitanguy I, Gontijo de Amorim NF, Radwanski HN Contour surgery in the patient with great weight loss. Aesthetic Plast Surg. 2000;24(6):406-11.
9. Roxo CDP, Pinheiro O, Almeida D. Abdominoplastia multifuncional. Rev Bras Cir Plast. 2004;19(3):64-74.
10.Borud LJ, Warren AG. Modified vertical abdominoplasty in the massive weight loss patient. Plast Reconstr Surg. 2007;119(6):1911-21.
11.Hurwitz DJ, Zewert T. Body contourning after bariatric surgery. Op Tech Plast Surg. 2002;(1):87-97.
12.Cintra W Jr, Modolin ML, Gemperli R, Gobbi CI, Faintuch J, Ferreira MC. Quality of life after abdominoplasty in women after bariatric surgery.Obes Surg. 2008;18(6):728-32.
13.Wallach SG. Abdominal contour surgery for the massive weight loss patient: the fleur-de-lis approach. Aesthet Surg J. 2005;25(5):454-65.
14.Savage RC. Abdominoplasty following gastrointestinal bypass surgery. Plast Reconstr Surg. 1983;71(4):500-9.
15. Ramirez O. U-M abdominoplasty. Aesthetic Surg J. 1999;19(4):279-86.
1. Full Member of the SBCP and FILACPS; Coordinator of Plastic Surgery at the HRHDS, Joinville, SC
2. Resident Physician R2; General Surgery HRHDS, Joinville, SC; Resident Physician
3. Third-year Medicine Student, Period; Faculdade Evangélica de Medicina de Curitiba, PR; Medicine Student
Fernando Sanfelice André
Rua Osvaldo Cruz, 128, Bairro Boa Vista
CEP: 89205-240 - Joinville, SC, Brasil
Article recceived: 01/08/2013
Article acceted: 01/09/2013
Study conducted at the Department of Obesity Plastic Surgery, Hospital Regional Hans Dieter Schmidt - Joinville, SC, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter