

Original Article - Year 2013 - Volume 28 -
Association of sociodemographic effects and injury to feelings of powerlessness and hope in individuals with venous ulcers
Associação dos fatores sociodemográficos e da lesão relacionados ao sentimento de impotência e esperança em indivíduos com úlcera venosa
ABSTRACT
OBJECTIVE: This study's objective was to evaluate feelings of powerlessness and hope in patients with venous ulcers and identify sociodemographic characteristics in the studied population.
METHODS: A clinical, descriptive, analytical and prospective study. 40 patients with venous ulcers participated. We used 3 instruments: a questionnaire that assessed demographic and clinical data, an Instrument for Measuring feelings of impotence and Herth Hope Index.
RESULTS: At Feelings of Impotence Scale patients scored a mean of 34.3 and at Herth Hope Index 27.50, revealing that these individuals feel powerless and hopeless that the wound can heal. Individuals aged between 50 and 59 years had an average of 39.00 at Feelings of Powerlessness Scale (P 0.120). At Herth Hope Index the average was 14.20 (P=0.508). Male, in both scales, had mean changes, with average of 36.00 at Feelings of Powerlessness Scale (P=0.068) and 26.70 as median at Herth Hope Index (P=0.332). Regarding the time of the injury, the average score was 39.00 at Feelings of Impotence Scale (p = 0.251) and 27.10 in Herth Hope Index, showing changes in patients over 1 to 2 years with injury. Patients who presented odor scored a high mean (36.10 /P=0.155) at Feelings of Impotence Scale and low mean at Herth Hope Scale (26.80).
CONCLUSION: Results have revealed that the subjects with venous ulcers in this study feel helpless and hopeless about the possibility of wound healing.
Keywords: Varicose Ulcers. Emotions. Quality of life.
RESUMO
OBJETIVO: Este estudo teve como objetivo avaliar o sentimento de impotência e esperança em pacientes com úlcera venosa e identificar características sociodemográficas nesta população.
MÉTODO: Estudo clínico, descritivo, analítico, prospectivo. Participaram 40 pacientes com úlcera venosa. Foram utilizados três instrumentos: um questionário que avaliou dados demográficos e clínicos, o Instrumento de Medida dos Sentimentos de Impotência e a Escala de Esperança de Herth.
RESULTADOS: Na Escala de Sentimentos de Impotência, os pacientes pontuaram escore médio de 34,3 e na Escala de Esperança de Herth 27,50, revelando sentimentos de impotência e pouca esperança de cicatrização. Os indivíduos entre 50 e 59 anos apresentaram a média total de 39,00, na Escala de Sentimentos de Impotência (p=0,120). Já na Escala de Esperança de Herth, a média foi de 14,20 (p=0,508). O gênero masculino, em ambas as escalas, apresentou média alterada, sendo 36,00 a média da Escala de Sentimentos de Impotência (p=0,068) e 26,70 a mediana na Escala de Esperança de Herth (p=0,332). Quanto ao tempo da lesão, o escore médio foi de 39,00 na Escala de Sentimentos de Impotência (p=0,251) e de 27,10 na Escala de Esperança de Herth, mostrando alteração em pacientes com mais de 1 até 2 anos com a lesão. Os pacientes que apresentaram odor pontuaram o escore médio alto (36,10/p=0,155) na Escala de Sentimentos de Impotência e escore médio baixo na Escala de Esperança de Herth (26,80).
CONCLUSÃO: Os resultados permitem afirmar que os indivíduos com úlcera venosa avaliados sentem-se impotentes e sem esperança quanto à cicatrização da lesão.
Palavras-chave: Úlcera Varicosa. Emoções. Qualidade de Vida.
Venous ulcers are the most common skin lesions of the lower limbs. They constitute the most severe manifestations of chronic venous insufficiency. As such, chronic wounds are a serious public health problem, with the associated clinical and surgical procedures costing more than one billion dollars per year in the United States of America (USA) 1,2. In industrialized countries, it is estimated that approximately 1% of the population will develop ulcers in the lower limbs at a certain stage in their lives, with the main cause being disturbances in the vascular-venous system3. Studies have shown that in the USA, the incidence of venous ulcer ranges from 500,000 to 800,000 cases. It is believed that this high prevalence is due to the aging of the population. In Europe and Australia, the incidences vary between 0% and 1% of the entire population. When considering open and healed wounds, the incidences vary between 1% and 1.3%4.
In Brazil, the data concerning ulcer incidence is limited. One study focused on the epidemiological aspects and determined the incidence of chronic venous insufficiency and varicose veins in a sample of 1,755 patients in the municipality of Botucatu-SP; the results showed that varicose veins were present in 47.6% of the cases, with severity associated with 21.2% of cases. In the sample, 3.6% of patients had venous insufficiency with either open or healed wounds5. The treatment of leg ulcers requires a long, complex, and varying course of approaches, with adequate, continuous, holistic care needed2. Alterations in health, with both chronic and acute homeostatic implications, raise contradictory feelings, which can perturb and discourage the patients; the pathological manifestations and the proposed therapies can have similar effects6.
Feelings can be reflections of mental capacity in the manifestation of traits and behaviors towards a specific life context, along with joy and sadness7,8. Psychoemotional responses are connected to diverse factors that determine and/or restrict the behavior of the individuals in relation to a particular problem, such as culture, personality traits, life experiences, frustrated expectations, among others6.
Powerlessness can be defined as: "the perception that one action from the self will not have a significant impact on the result obtained; lack of control as perceived over a present situation or an immediate event," and was identified and recognized in 1982 by the North American Nursing Diagnosis Association-International (NANDA)9. This Association describes the powerless patient as the one that shows weakness and incapacity that leads to inability at the level of decision-making6,9,10. These studies highlight the need to present this type of diagnosis in a delicate way, as expressions such as powerlessness, helplessness, abandonment, and inadequacy can be misunderstood in daily nursing practice6,10.
Hope is a subtle way to declare therapeutic power in relation to a severe case, the mechanisms of action, the positive reaction concerning something that is believed by the self, and the direct interference of holistic aspects (physical, mental and spiritual) in the quality of life11.The feeling of hope can be a tool for dealing with disease or with any other problem, for its capacity to translate a bad prognosis, associated with suffering, into a context characterized by the constant search for improvement and resolution of the specific problem11,12.
Lack of skin integrity can compromise quality of life directly due to a variety of reasons, as this condition leads to significant changes for the individual and family; these can be limiting, often difficult to understand, and incompatible13.This work is based on daily empirical observation of signs of fatigue, dismay, and hopelessness in individuals with wounds who give up instead of concentrating their efforts on cicatrization. These signs may lead to permanent restrictions and to limited improvement of the quality of life at various levels, which can go from compromising a simple walk to preventing the demonstration of appreciation. Thus, the patients were followed at the clinical-assistance level in a holistic context, with the objective of evaluating feelings of powerlessness and hope in patients with venous ulcers and to identify the sociodemographic data of the studied population.
OBJECTIVES
The objective of this study was to evaluate feelings of powerlessness and hope in patients with venous ulcers and to identify the sociodemographic characteristics of this population.
METHODS
This was a descriptive, analytical, prospective, and non-randomized primary clinical study. This study was performed at the Center of Nursing Assistance and Teaching.
The sample was composed of 40 patients with venous ulcers. Data collection was performed after the approval of the project by the Research Ethics Committee of the Faculty of Health Sciences "Dr. José Antônio Garcia Coutinho" with project number 23,240 from March to December of 2012. Consecutive patients were included in the study. The inclusion criteria were older than 18 years old and index ankle/arm ulcers between 0.8 and 1.0. The exclusion criteria were patients with mixed ulcers, arterial ulcers, and/or diabetic ulcers. Three instruments were used for data collection: first, the questionnaire concerning demographic and clinical data; second, the Powerlessness Assessment Scale; and finally, the Herth Hope Index.
The Powerlessness Assessment Scale was validated and its confidence was evaluated a posteriori. With 210 patients, a five-point Likert-type frequency scale format was used, ranging from never to always. The scoring of powerlessness was as follows: 1 = never; 2 = rarely; 3 = sometimes; 4 = frequently; and 5 = always. For the items scoring the absence of powerlessness, the scale was inverted: 5 = never; 4 = rarely; 3 = sometimes; 2 = frequently; 1 = always. The total possible score was 120 points. There are three components to the scale measurements: behavioral performance capacity (Cronbach's a = 0.845); perception of decision-making capacities (Cronbach's a = 0.834); and emotional response to situational control (Cronbach's a = 0.578). This instrument's scores can be summed in each domain; overall, the higher the score, the more intense was the powerless-ness feeling10,14.
The Herth Hope Index used in this study, an adaptation from the original Herth Hope Index, is an instrument that comprises 12 items with a total score ranging from 12 to 48 points; the answers are Likert-type with four levels, and the higher the score, the higher the hope was. Items three and six have inverted scores15,16. For statistical analysis, the following tests were used: Mann-Whitney and chisquare test of independence. In all statistical tests, the significance level was 5% (p < 0.05).
RESULTS
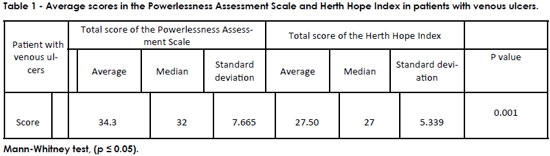
From Table 1, it can be observed that the average score of the Powerlessness Assessment Scale was 34.3 and that of the Herth Hope Index was 27.50. Both results show that individuals with venous ulcers feel powerless toward their lesion and have low hope concerning wound healing. The difference between groups was statistically significant.
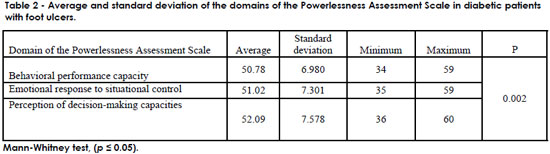
Table 2 shows that the average for the domain "Behavioral performance capacity" was 50.78. For "Emotional response to situational control," the average was 51.02, and for "Perception of decision-making capacities," it was 52.09. These results highlighted the fact that the participants in this study felt powerless.
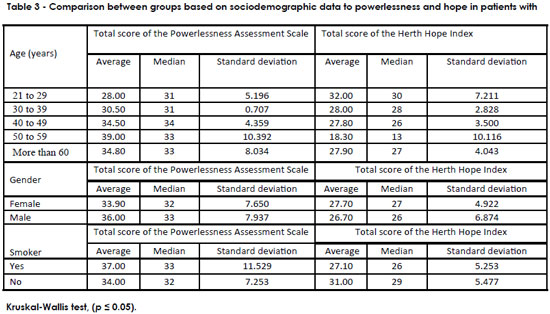
Table 3 shows that patients between 50 and 59 years old had a total average of 39.00 in the Powerlessness Assessment Scale (p = 0.120). Concerning the Herth Hope Index, the average was 14.20 (p = 0.508), which demonstrated that these patients feel powerless with low hope in a cure. The difference was not statistically significant. In both scales, men had altered scores, with an average of 36.00 in the Powerlessness Assessment Scale (p = 0.068) and an average of 26.70, a low score, in the Herth Hope Index (p = 0.332), thus showing that despite feeling powerless, men hope for the cure. The differences were not statistically significant. Concerning smoking patients, the average score was 37.00 on the Powerlessness Assessment Scale, which can be considered a high score (p = 0.535); however, the average score for smoking patients on the Herth Hope Index was 27.10 (p = 0.090). This result indicated that these individuals feel significant powerlessness, but hope for the cure. There was no statistical significance.
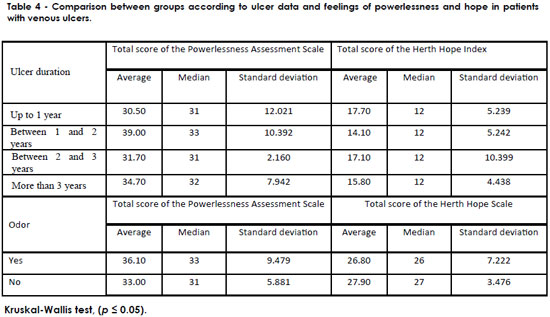
Table 4 shows that, regarding the duration of the ulcer, individuals with more than one and up to two years of lesions had an average score of 39.00 on the Powerlessness Assessment Scale (p = 0.251) and an average of 27.10 on the Herth Hope Index. Such findings indicate that individuals who have had wounds for more than one year and up to two years have higher powerlessness feelings, but maintain hope in the cure. Individuals with malodorous wounds had high average scores on the Powerlessness Assessment Scale (36.10, p = 0.155) and low average scores on the Herth Hope Index (26.80). These results show that these patients feel strongly about their powerlessness but hope for the cure. There were no statistically significant differences for these variables.
DISCUSSION
Venous ulcer is a chronic disease, characterized by periods of exacerbation and remission. The long cicatrization process leads to physical, emotional, and psychological discomfort. Treatment restricts the life style of the patients and interferes with the daily activities of the individuals. For these reasons, there is a need for emotional support and specific mechanisms to deal with this situation, as this population feels powerless and hopeless concerning the possibility of wound healing.
In this study, participants had an average score of 34.3 on the Powerlessness Assessment Scale and of 27.50 on the Herth Hope Index. Both results indicated that the individuals with venous ulcers feel powerless toward their lesions and have diminished hope that the wounds will heal17-21. Feelings such as fear, regret, and powerlessness are common in patients with wounds that are difficult to heal, and these feelings tend to worsen when the lesion is malodorous or with exudate. Because of these symptoms, the patient may lose hope that the wound will ever heal. To depend on others can generate fear and frustration in a society where independence is highly valued. Fear is part of the lives of human beings and can worsen when a person is sick. It leads to emotional instability, with conflicts, doubts, and unexpected reactions.
For Carpenito-Moyet22, feelings of power-lessness reflect a state where the individual or group faces a lack of control or interpersonal authority concerning events or situations that interfere with their way of living, as well as with their aims and plans for the future. In a study describing the powerlessness of patients during cardiac post-surgery that compared patients with heart valve surgery with patients with coronary surgery, 44 (58.7%) patients felt powerless. These patients had doubts concerning plans for the future and the establishment of objectives (75.0%), expressed doubts about role fulfillment (63.6%), and displeasure and frustration due to the inability to perform tasks and/or personal activities (56.8%)23.
A study was designed to evaluate hope in three different groups and their sociodemographic and clinical variables, which correlated hope with those variables, with a sample of 131 individuals-47 cancer patients, 40 diabetic patients, and 44 care-takers/family-who answered the Herth Hope Index, the Rosenberg Self-esteem Scale, the Beck Depression Inventory, and a personal data form. There was no difference between groups in the hope scores. Hope positively correlated with self-esteem and negatively with depression. For cancer patients, the hope score did not correlate with any of the clinical variables. For diabetic patients, the different treatments, as well as other co-morbidities, did not influence hope. The study concluded that patients with chronic diseases and their families had high hope scores. The measurement of hope can improve nursing care16.
In addition, lack of hope can be described as "a subjective state in which an individual cannot envision alternatives or available personal choices, or envisions the alternatives but is incapable of mobilize energy in his direction" 9. Carpenito-Moyet agreed with the NANDA definition and highlights that this describes an individual that is at the stage of not being able to understand or influenced by signs of life improvement 22. Hope for a cure remains in the individual, in the belief that, at a given time, the disease will disappear and a miracle will happen. In some situations, that is the source of strength that leads the individual to continue with treatment24.
From the analysis of the results concerning the sociodemographic data, there was a prevalence of powerlessness (39%) in the group aged 50 and 59; however, the average hope was 18% in the same group. In this study, male participants felt powerless but with hope in a cure. Studies have revealed that the women are more affected by lesions; nonetheless, most men develop emotional or psychological changes following the appearance of a wound, which can affect the quality of life, self-esteem, self-image, or sleep, from 50 to 60 years of age21,25,26.
In studies to evaluate depression in patients with wounds who had any kind of depressive condition from moderate to severe, symptoms were self-depreciation, sadness, distortion of the body image, and diminished libido. Authors concluded that when an individual develops a wound, he/she shows emotional changes that can indicate several levels of depressive symptoms19,21. In other studies, authors concluded that for a person with a wound, the exterior signs that characterize the skin lesion, such as the exudate, the malodor, and the edema, are sufficient to impact the quality of life of these patients, their functional capacities, and their sleep. These characteristics are also directly affected by sociodemographic aspects, such as gender, civil status, and occupation20,26,27.
Mental health can be affected by functional capacity, such as difficulty or incapacity in performing daily activities; moreover, the odor and the exudate can have a negative impact over the psychological health, hope, and faith of the individuals. Therefore, these patients undergo changes of humor, suffer from reduced motivation, loss of self-control, helplessness, and feel pessimistic about the future. These emotions correlate with mental health, such as the worsening of the overall status of the patient, and can lead to mental perturbations like depression19,21,28,29. However, when the patient realizes that the lesion is improving, he/she feels useful, productive, and misses daily activities.
In some cultures, people consider wound cicatrization and the healing of other diseases to be due to beliefs and not to resources and scientific discoveries. Hope makes the patient stronger to deal with the challenges associated with the disease and makes him/her feel alive, human and active in the search for survival30-32.Remarkably, patients with wounds, in general, are constantly melancholic, a form of psychic suffering that is a consequence of the deterioration of their quality of life. These individuals are victims of imposed values that are not in agreement with human solidarity33.
Research has shown that venous ulcers can lead to severe psychological problems in affected individuals that can be translated into several degrees of depression. It is known that, in pathological conditions, there is no clear separation between the physical and emotional contexts, which discourages a prosperous and positive attitude towards the future. In addition, such issues impose functional limitations related to the bad condition of the wounds34,35. In the nomenclature associated with diagnosis, the related factors are in agreement with the factors imposed by the society, which leads to conditioning of certain alterations: "helpless life style, disease, incapacity, fear of disapproval, constant feedback, abandon, prolonged restriction of activities with consequent isolation"9,22.
In this study, the average result concerning powerlessness was significant for men (36.00%). On the contrary, men were more hopeful in the possibility of wound cicatrization. In studies testing powerlessness and hope in patients with leg ulcers, the average score in the Powerlessness Assessment Scale was higher for diabetic individuals with ulcerated feet (53.3), whereas for venous ulcer patients, the average was 34.3. Concerning hope on the Herth Index, the average was lower in diabetic patients with ulcerated feet, 16.50, than in patients with venous ulcers, 27.50. Authors concluded that diabetic patients with ulcerated feet feel powerless and hopeless toward wound healing. In contrast, patients with venous ulcers feel powerless but with hope for wound cicatrization30.
In this context, a study has established that patients with lesions oscillate between hope and despair due to the delayed cicatrization process, which showed that having an ulcer places the patient among esthetic and visual alterations, socializes and faces pain episodes, is confronted with the body's functional limitations, and the hope of freedom from a "diseased body." The same study has concluded that image is of high importance in the elderly, and it is the role of professional therapists to show perceptual sensibility towards the individuals by inferring the extent to which interference in their lives would be appropriate36.
The realization that incapacity feelings predominate in patients with venous ulcers, following the thorough analysis of the results presented here and taking into consideration empirical and scientific data, as well as information from the professional experience concerning the difficulties in maintaining adherence to therapy, leads to the question: how much does the behavior of the health professional, decisive, participant, immutable, inflexible, isolated and selfish, contribute to the diagnosis here identified? Studies showed that when the health professional involves the patient in the treatment, allowing bodily autonomy, responsibility, and true knowledge of the problem, it leads to adaptation to the problem, thus producing better responses to the proposed therapy and avoiding negative feelings18,33. Social isolation denotes a strong risk factor contributing to diagnoses that diminish the capacities of the individuals37,38.
Feelings associated with the doubt of a definitive cure and that force the individual to consider the possibility of either yes or no, lead to instability towards life, and to decision making in the context of uncertainty about the future. Because a final prognosis may take considerable time, studies have highlighted the benefits of increasing physical activity and mobility exercises for the lower limbs as a preventive action to deal with recurrent ulcers. Previous work has also shown the efficacy of the use of elastic socks in preventing relapse39.
This work emphasizes the need to redirect the attention given to patients with venous ulcers toward the alterations of the functional capacity of those who live with these wounds, the establishment of main health care needs, and the capacitation of the caregiver to deal with the described incapacities; this new approach should be practiced both in hospitals and ambulatory health services, Family Health Programs, amongst others.
Another study has suggested that patients with venous ulcers are directly responsible for the decrease in their quality of life, as the psychosocial adaptation is low due to the difficulties associated with adherence to therapy, which can only increase the chronic nature of this condition39-41.Considering the increase in chronic diseases and in patients with wounds registered during the last decades, it is unavoidable to redirect the academic training and qualifications of the health professionals to achieve the valorization not only of contents learned, but also of practice focused on patient assistance.
Future studies should be performed aiming at increasing sample size and at improving the understanding of the extent of such problems. A limitation of this study was the limited number of participants, and more research is required to identify the emotional alterations affecting these patients and to propose preventive and therapeutic approaches.
CONCLUSION
The results obtained led to the conclusion that the individuals with venous ulcers studied here feel powerless and hopeless about the possibility of wound cicatrization.
REFERENCES
1. Margolis DJ. Epidemiology of Wounds. In: Mani R, Romanelli M, Shukla V. Measurements in Wound Healing. London: Springer; 2012. p.145-153. Doi: 10.1007/978-1-4471-2987-5_8.
2. Salavastru CM, Nedelcu LE, Tiplica GS. Management of leg ulcers in patients with chronic venous insufficiency: the experience of a Dermatology Clinic in Bucharest, Romania. Dermatol Ther. 2012;25(4):304-13.
3. Silva MH, Jesus MCP, Merighi MAB, Oliveira DM, Santos SM, Vicente EJD. Manejo clínico de úlceras venosas na atenção primária à saúde. Acta Paul Enferm. 2012;25(3):329-33.
4. Silva FAA, Moreira, TMM. Características sociodemográficas e clínicas de clientes com úlcera venosa de perna. Rev Enferm UERJ. 2011;19(3):468-72.
5. Maffei FH, Magaldi C, Pinho SZ, Lastoria S, Pinho W, Yoshida WB, et al. Varicose veins and chronic venous insufficiency in Brazil: prevalence among 1755 inhabitants of a country town. Int J Epidemiol. 1986;15(2):210-7.
6. Braga CG, Cruz DALM. A resposta psicossocial de impotência em pacientes no pós-operatório de cirurgia cardíaca. Rev Esc Enferm USP. 2003;37(1):26-35.
7. Del Porto JA. Conceito e diagnóstico. Rev Bras Psiquiatr. 1999;21(1):6-11.
8. Kaspar K, König P. Emotions and personality traits as high-level factors in visual attention: a review. Front Hum Neurosci. 2012;6:321.
9. Nanda Internacional. Diagnósticos de Enfermagem Nanda, Definições e Classificações 2009-2010. Porto Alegre: Artmed; 2010.
10. Braga CG, da Cruz Dde A. Powerlessness: differentiation from other diagnoses and concepts. Rev Esc Enferm USP. 2005;39(3):350-7.
11. Watson J. Enfermagem: Ciência Humana e Cuidar. Uma Teoria de Enfermagem. Loures: Lusociência; 2002.
12. Duggleby WD, Degner L, Williams A, Wright K, Cooper D, Popkin D, et al. Living with hope: initial evaluation of a psychosocial hope intervention for older palliative home care patients. J Pain Symptom Manage. 2007;33(3):247-57.
13. Lucas LS, Martins JT, Robazzi MLCC. Qualidade de vida dos portadores de feridas em membros inferiores - úlcera de perna. Cienc Enferm. 2008;14(1):43-52.
14. Braga CG, Cruz DALM. Powerlessness assessment tool for adult patients. Rev Esc Enferm USP. 2009;43(Spe):1062-9.
15. Sartore AC, Grossi SA. Herth Hope Index--instrument adapted and validated to Portuguese. Rev Esc Enferm USP. 2008;42(2):227-32.
16. Balsanelli ACS, Grossi SAA, Herth K. Assessment of hope in patients with chronic illness and their family or caregivers. Acta Paul Enferm 2011;24(3):354-8.
17. Jones J, Barr W, Robinson J, Carlisle C. Depression in patients with chronic venous ulceration. Br J Nurs. 2006;15(11):S17-23.
18. Finlayson K, Edwards H, Courtney M. The impact of psychosocial factors on adherence to compression therapy to prevent recurrence of venous leg ulcers. J Clin Nurs. 2010;19(9-10):1289-97.
19. Salomé GM, Blanes L, Ferreira LM. Evaluation of depressive symptoms in patients with venous ulcers. Rev Bras Cir Plást. 2012;27(1):124-9.
20. Salomé GM, Blanes L, Ferreira LM. Functional capability of patients with diabetes with foot ulceration. Acta Paul Enferm. 2009;22(4):412-6.
21. Salomé GM, Blanes L, Ferreira LM. Assessment of depressive symptoms in people with diabetes mellitus and foot ulcers. Rev Col Bras Cir. 2011;38(5):327-33.
22. Carpenito-Moyet LJ. Planos de cuidados de enfermagem e documentação. 4ª ed. Porto Alegre: Artmed; 2006.
23. Braga CG, da Cruz Dde A. The powerlessness psycho-social response in the postoperative period in cardiac surgery patients. Rev Esc Enferm USP. 2003;37(1):26-35.
24. Castro SLS, Ferreira NMLA, Roque M, Souza MBB. Vivendo uma situação difícil: a compreensão da experiência da pessoa com úlcera venosa em membros inferiores. Rev Estima. 2012;10(1):12-19.
25. Salomé GM, Pellegrino DMS, Vieira TF, Blanes L, Ferreira LM. Sleep quality among patients with venous ulcers: a cross-sectional study in a health care setting in São Paulo, Brazil. Wounds. 2012;24(5):124-31.
26. Nogueira GS, Zanin CR, Miyazaki MCOS, Godoy JMP. Quality of life of patients with chronic venous ulcers and sociodemographic factors. Wounds. 2012;24(10):289-92.
27. Salomé, GM, Donata MSP, Blanes L, Ferreira LM. Sleep quality in patients with diabetic foot ulcers. Wounds. 2013;25(1):20-7.
28. Souza Nogueira G, Rodrigues Zanin C, Miyazaki MC, Pereira de Godoy JM. Venous leg ulcers and emotional consequences. Int J Low Extrem Wounds. 2009;8(4):194-6.
29. Waidman MAP, Rocha SC, Correa AB, Marcon SS. Daily routines for individuals with a chronic wound and their mental health. Texto Conexto Enferm. 2011;20(4):691-9.
30. Salomé GM, Alves SG, Costa VF, Pereira VR, Ferreira LM. Feelings of powerlessness and hope for cure in patients with chronic lower-limb ulcers. J Wound Care. 2013;22(6):300, 302-4.
31. Silva DM, Mocelin KR. O cuidado de enfermagem ao cliente portador de feridas sob a óptica do cuidado transcultural. Nursing. 2007;105(9):81-8.
32. Salome GM, Ferreira LM. Quality of life in patients with venous ulcers treated with Unna's boot compressive therapy. Rev Bras Cir Plást. 2012;27(3):466-71.
33. Mapplebeck L. Case study: psychosocial aspects of chronic bilateral venous leg ulcers. Br J Community Nurs. 2008;13(3):S33-4.
34. Salomé GM, Blanes L, Ferreira LM. Avaliação de sintomas depressivos em pessoas com úlcera venosa. Rev Bras Cir Plást. 2012;27(1):124-9.
35. Malaquias SG, Bachio MM, Sant'Ana SMSC, Dallmarmi CCB, Junior RSL, Ferreira PS. Pessoas com úlceras vasculogênicas em atendimento ambulatorial de enfermagem: estudo das variáveis clínicas e sociodemográficas. Rev Esc Enferm USP. 2012;46(2):302-10.
36. Ebbeskog B, Ekman SL. Elderly persons' experiences of living with venous leg ulcer: living in a dialectal relationship between freedom and imprisonment. Scand J Caring Sci. 2001;15(3):235-43.
37. Broer T, Nieboer AP, Bal R. Mutual powerlessness in client participation practices in mental health care. Health Expect. 2012 Mar 6. [Epub ahead of print]
38. An GJ, Kim MJ. Powerlessness, social support, and glycemic control in Korean adults with type 2 diabetes. Contemp Nurse. 2012;42(2):272-9.
39. Nelson EA, Bell-Syer SE. Compression for preventing recurrence of venous ulcers. Cochrane Database Syst Rev. 2012;8:CD002303.
40. Costa IKF, Nóbrega WG, Costa IK, Torres GV, Lira ALB, Tourinho FSV, et al. Pessoas com úlceras venosas: estudo do modo psicossocial do modelo adaptativo de Roy. Rev Gaúcha Enferm Porto Alegre. 2011;32(3):561-8.
41. Salomé GM, Espósito VHC. Vivências de acadêmicos de enfermagem durante o cuidado prestado às pessoas com feridas. Rev Bras Enferm. 2008;61(6):822-7.
1. Nursing Student at Sapucaí Valley University (UNIVÁS), Pouso Alegre, MG, Brazil
2. Nursing Student at Sapucaí Valley University (UNIVÁS), Pouso Alegre, MG, Brazil
3. Medical Doctor, Sapucaí Valley University (UNIVÁS), Pouso Alegre, MG, Brazil
4. MSc in Nursing, Full Professor, Sapucaí Valley University (UNIVÁS), Pouso Alegre, MG, Brazil
5. Stoma therapist "TiSOBEST", MSc, PhD, Postdoc and Professor of the Master's Degree in Applied Health Sciences at Sapucaí Valley University (UNIVÁS), Pouso Alegre, MG, Brazil
Suellen Garcia Alves
Av. Francisco de Paula Quintaninha Ribeiro, 280/134
Jabaquara CEP: 04330-020. São Paulo, SP, Brasil
Manuscript received: 03/05/2013
Manuscript accepted: 03/06/2013
Work performed at the Sapucaí Valley University (UNIVÁS), Pouso Alegre, MG, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter