

Original Article - Year 2013 - Volume 28 -
Neck contour alterations:
Alterações do contorno cervical: Classificação lamelar e protocolo de tratamento
ABSTRACT
OBJECTIVE: The aim of the current study is to propose a classification based on neck lamellas for the aesthetic variations of the cervical region, considering its unique anatomy and analysing each structure involved (skin, muscle, fat and submandibular gland), in order to make it easier to choose the most appropriate surgical treatment.
METHOD: The senior author, elaborated an observational study of 480 patients operated for neck and face lift between 1998 and 2010, established a classification comparing the skin flaccidity, the amount of fat accumulation, muscle flaccidity and cervical contour alterations, with the best surgical treatment for each group, being grade I (11.7%), grade II (7%), grade III (23%), grade IV (40%) and grade V (18.3%).
RESULTS: The development of the current classification made it possible to group the cervical alterations that results from the aging process. Each group has common, easily recognizable alterations and for each one we have proposed a different treatment algorithm, in relation to the technique and the scar positioning (classic neck and facelift, short scar facelift, cervical lift, atypical lift and neck and facelift with anterior temporal scar).
CONCLUSION: With the present study it was possible to come to the conclusion that the cervical region is the main determinant for the selection of the best surgical technique and scars placement in the surgery for the rejuvenation of the neck and face.
Keywords: Face. Neck, Rhytidoplasty. Surgery, Plastic. Reconstructive Surgical Procedures.
RESUMO
OBJETIVO: O objetivo do presente trabalho foi propor uma nova classificação das alterações estéticas da região cervical, com base na sua anatomia, a fim de direcionar o tratamento cirúrgico adequado. O intuito foi classificar e sistematizar a abordagem cirúrgica de cada estrutura envolvida (pele, músculo, gordura e glândula submandibular), correlacionando o procedimento cirúrgico mais indicado para o seu tratamento.
MÉTODO: O autor sênior, baseado em observação de 480 casos operados, entre os anos de 1998-2010, estabeleceu uma classificação correlacionando a flacidez de pele encontrada, grau de lipodistrofia, alteração muscular e alteração do contorno cervical, com o tratamento empregado, sendo grau I (11,7%), grau II (7%); grau III (23%), grau IV (40 %), grau V (18,3%.).
RESULTADOS: O desenvolvimento da presente classificação demonstrou ser possível agrupar as alterações cervicais, decorrentes do processo de envelhecimento humano, em subgrupos (Grau I-V), com alterações comuns, facilmente reconhecíveis, facilitando a proposição do melhor tratamento para a região cervical e propiciando a criação de um algoritmo terapêutico. Esta classificação em subgrupos auxilia o cirurgião na escolha do tipo de abordagem cirúrgica e cicatrizes (Lifting cervico facial clássico, Lifting cérvico facial com cicatriz reduzida, Lifting cervical, Lifting atípico com cicatriz temporal anterior).
CONCLUSÃO: Concluímos que a região cervical é a principal determinante na escolha do tipo de abordagem cirúrgica e cicatrizes, no rejuvenescimento cérvico facial.
Palavras-chave: Face. Pescoço. Ritidoplastia. Cirurgia plástica. Procedimentos cirúrgicos Reconstrutivos.
The aesthetic surgical procedure for the rejuvenation of the face and neck, remains one of the most frequently performed surgical procedures in the entire world. With the aging process affecting lives of more and more people around the world every year, it is clear that more men and women will search for plastic surgeons to perform some rejuvenating procedure of the face and neck.
Historically, facelift was first reported by Lexer in 1906, however, the first published article reporting the procedure was by Passot, in 19191. Since the first published works, the importance of the correct management of the cervical region for a better facelift result was evident. In the beginning, it was accomplished by undermining the skin and pulling it2. From Aufrich, in 1906, to Cardoso de Castro, in 1980, much was described about the neck's superficial anatomy and its changes as a consequence of the aging process, as well as the many surgical and non-surgical possible approaches to treat these changes3-6.
When evaluating an aged face and neck, one must bear in mind that one of the first visible changes is the loss of neck contour. This is caused by a myriad of anatomical changes that are well known. The affected tissues are the skin, with wrinkles and flaccidity, muscle hypotonia, with formation of visible platysmal bands, loss of adequate jawline contour, herniation or bulging of subplatysmal structures, such as submandibular gland, and anterior accumulation of fat, above the platysma muscle.
The aesthetic neck, according to Elleenbogen & Karlin7, is the one that preserves a cervicomental angle between 105 e 120 degrees, a well defined jawline, visible anterior border of the sternocleidomastoid muscle, a subhyoid depression, visible thyroid cartilage bulge and a submental-sternocleidomastoid angle of 90 degrees. Subsequently, others added to these parameters, the importance of the anterior projection of the chin, to the neck's aesthetic8,9. The submental region is defined as a triangle, with the hyoid bone being its base, the chin being its apex and the anterior part of the digastric muscles as its lateral walls. The submental's floor is formed by the mylohyoid muscle5.
Although the anatomy of the face and neck is well defined, some doubts remain regarding the best treatment for each one of the variables presented by the aging process. Many authors have tried to clarify this issue, proposing an enormity of surgical techniques to each variants of the aging process of the face and neck. Nevertheless, some techniques may apply to different variants of the aging process, what may cause some confusion to surgeons. Some other authors tried to classify these variants encountered with the aging process of the face and neck, proposing different approaches to each variant7,10-13, being all these classifications complex and of limited practical use. However, this shows how much concern actually exists regarding the need to establish the scientific bases for the choice of the most appropriate surgical procedure for each person's encountered variants.
The aim of the present study is to propose a classification based on anatomical lamellar layers of the aesthetic variants of the neck, in order to help choosing the best surgical procedure. So, we divided the neck in three layers: anterior layer being the skin and subcutaneous fat; middle layer being the platysma muscle and its fascia; and deep layer being the subplatysmal structures, such as submandibular gland, digastric muscle, subplatysmal fat and hyoid bone.
METHOD
It was conducted an analytical and observational study of all patients that underwent neck and face lift, between the years 1998 and 2010, at the senior author's private Clinic, at Natal and Rio de Janeiro, Brazil. In all patients, the authors analyzed the changes in their face and neck anatomy and appearance that took place because of aging. Afterwards, the authors grouped the patients according to the severity of the changes encountered, relating them to the performed surgical procedure.
The neck structures were subdivided according to its relation to the superficial musculoaponeurotic system (SMAS), as it follows: anterior lamella being the skin and subcutaneous fat; middle lamella being the SMAS (platysma muscle and its fascia); deep lamella being the subplatysmal structures (submandibular gland, digastric muscle, subplatysmal fat and hyoid bone).
According to the severity of the lamellar alterations found in each case, the surgical procedure was chosen (Table 1). In almost all cases we used the liposuction, with or without open submental lipectomy, associated with one of the following surgical procedures: only liposuction with 3 mm cannula (grade I, Figure 1) , neck lift (N.L. - grade II, Figure 2); short scar face and neck lift (S.S.F.N.L. - grade III, Figure 3); Pitanguy's face lift and neck lift1,3 (P.F.N.L. - grade IV, Figure 4); atypical face and neck lift with anterior to the hairline scar (A.F.N.L. - grade V, Figure 5). In the last surgical procedure, it is possible to divide the vector of traction of the skin in two, being one vertical and the other posterior oblique in patients with severe neck alterations (grade V), enhancing the efficacy of the skin repositioning that allows a better redraping of the skin of the neck. The undermining of the neck's skin is accomplished in the most anterior part of the neck and in the lateral aspect of it, being occasionally possible, and advisable, to unite the undermined flaps in the middle. The submental incision is placed 3 mm caudal to the submental crease, making it possible to adequately address the middle area of the neck. Whenever necessary, it is possible to place a chin implant through this incision. We do not advice to excise skin from this incision, because this surface will change from a convex to a concave one, and it will be necessary to have enough skin to cover it7.
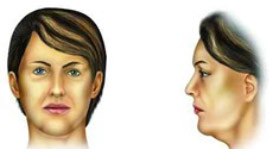
Figure 1 - Typical encountered alterations in grade I patients
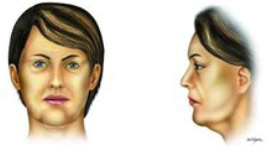
Figure 2 - Typical encountered alterations in grade II ptients
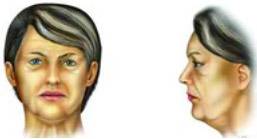
Figura 3 - Typical encountered alterations in grade III patients
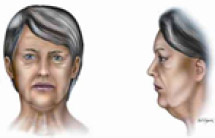
Figura 4 - Typical encountered alterations in grade IV patients
Figura 5 - Typical encountered alterations in grade V patients
In the presence of medial platysmal borders, we performed the middle sutured of these borders , from the thyroid cartilage to the submental level, using absorbable 4-0 sutures, through the submental incision of 3 to 4 cm5,10 (patients grade II, III, IV and V). In some cases, we excised a strip of muscle, tangential to the hypertrophic border of the platysma. In those patients in the groups II to V, the lateral borders of the platysma muscle are pulled and sutured with four to five absorbable 4-0 sutures, to the mastoid preeminence.
In those cases where it is observed a bulge in the submandibular region (submandibular gland ptosis), we used an intraplastysmal vicryl® 4-0 vertical suture along with the platysmal fibers from the most medial area of the neck to the second premolar tooth.
Furthermore, the authors submitted the photographs taken before and after 12 months of the surgical procedures to the analysis by two independent and experienced plastic surgeons, that graded the success or not of the procedures according to the improvement of the cervical region. These surgeons graded it from 1 to 10, according to those paramethers previously described by Elleenbogen and Karlin7. Then, the authors stratified the grades as excellent (9-10), good (7-8), satisfactory (5-6) and unsatisfactory (1-4).
RESULTS
Between 1998 and 2010, 480 patients underwent neck and face lift, at the senior author's private Clinic. Of those, 86 where male (18%) and 394, female (82%), while 82% where primary facelifts, 15%, secondary, and 3%, tertiary. All patients were grouped in one out of five groups, according to the anatomical changes observed and surgical treatment employed (Tables 1 and 2, and Figure 1 to 5). Of the 480 cases, 11,7% were classified as grade I (Figure 6); 7%, grade II (Figures 7 and 8); 23%, grade III (Figures 9 and 10); 40%; grade IV (Figures 11 and 12) and 18.3%, grade V (Figures 13 and 14). The follow-up time was of 18 to 48 months, with an average of 32.1 months.
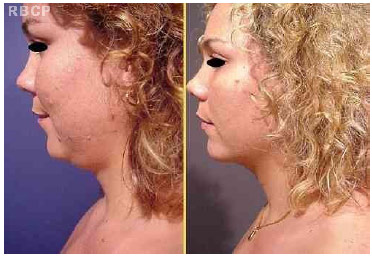
Figure 6 - 28 years old patient, classified as grade I, before (left) and 8 months after (right) neck liposuction (lateral view).

Figure 7 - 45 years old patient, classified as grade II, before (left) and 12 months after (right) neck lifting (lateral view)

Figure 8 - Figure patient, before (left) and 12 months after (right) surgery (anterior view)

Figure 9 - 49 years old patient, classified as grade III, before (left) and 14 months after (right) short scar face and neck lift (lateral view).

Figure 10 - Patient, before (left) and 14 months after (right) surgery (anterior view).

Figure 11- 53 years old patient classified as grade IV, before (left) and 9 months after (right) Pitanguy's face and neck lifting (lateral view)

Figure 12 - Patient before (left) and 9 months after (right) surgery (anterior view).
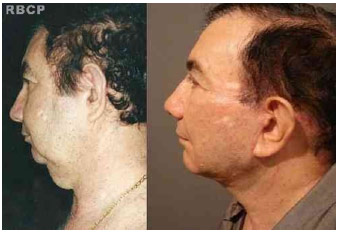
Figure 13 - 63 years old patient classified as grade V, before (left) and 18 months after (right) atypical face and neck lifting with anterior to the hairline scars (lateral view
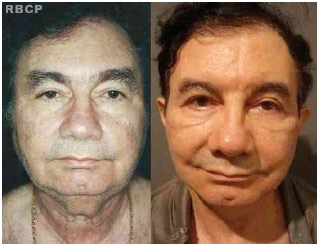
Figure 13 - 63 years old patient classified as grade V, before (left) and 18 months after (right) atypical face and neck lifting with anterior to the hairline scars (front view).
The results based on the photograph's analysis by the two independent plastic surgeons are listed below (Figures 15 and 16):
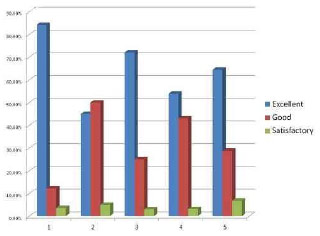
Figure 15 - Analysis results by plastic surgeon number 1
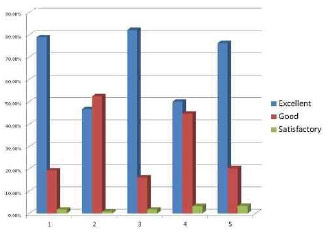
Figure 16 - Analysis results by plastic surgeon number 2
Group 1 patients: 78.9% of excellent results, 19.3% of good results and 1.8% of satisfactory results according to examiner 1 whereas examiner 2 found 84.2% of excellent results, 12.2% of good results and 3.6% of satisfactory results.
Group 2 patients: 46.7% of excellent results, 52.5% of good results and 0.8% of satisfactory results according to examiner 1, whereas examiner 2 found 45% of excellent results, 50% of good results and 5% of satisfactory results.
Group 3 patients: 82.14% excellent results, 16.06% good results and 1.8% of satisfactory results according to examiner 1, whereas examiner 2 found 72% of excellent results, 25% of good results and 3% of satisfactory results.
Group 4 patients: 50% of excellent results, 44.7% of good results and 3.3% of satisfactory results according to examiner 1, whereas examiner 2 found 53.9% of excellent results, 43% of good results and 3.1% of satisfactory results.
Group 5 patients: 76.3% of excellent results, 20.3% of good results and 3.4% of satisfactory results according to examiner 1, whereas examiner 2 found 64.4% of excellent results, 28.8% of good results and 6.8% of satisfactory results.
There were no unsatisfactory results in any group of patients according to both examiners.
The complications related to the procedures were surgical revisions in 15 cases, scar alterations in 10, mandibular paresis in 4 and hematoma in 3 patients (Table 3).
DISCUSSION
In the last few years several authors have proposed different classifications for the variants of neck contour7,10,11,13,16-20. All of them based their classifications in muscle and fat alterations, correlating the surgical procedures to the treatment of these aspects of the neck aging process. In the present study, however, the authors determinate the need to correctly diagnose the alterations of the neck contour, as well as identify the degree of change in the anatomical structures involved, therefore individualizing the treatment. In order to do so, the authors defined the existence of three aesthetically important layers or lamellas at the neck. Those layers are divided in superficial, intermediate and deep. It is important to bear in mind that a correct lipectomy, either open or closed9,13,21, with the adequate repositioning of the skin flaps, alongside with the treatment of the deeper neck structures is of utter importance to achieving a better neck contour. This might as well be individualized according to the degree of the neck alterations identified.
In the present study, we developed, based on clinical and surgical observations, a diagnostic classification of the alterations identified in the aged face and neck. The most commonly involved structures are the skin, the subcutaneous fat, the platysma muscle and the neck contour. Other involved structures, such as, those of the deep layer of the neck are depicted in the classification as well, although less frequently identified and treated. The classification divides the alterations according to their severity, in five groups, as shown in Table 1 and in Figures 1 to 5.
As shown in the present study, the main abnormality found in the superficial layer of the neck was the skin flaccidity, which can be associated to abnormal fat accumulation in the subcutaneous space. Neck liposuction, therefore, is necessary in all cases of surgical procedures to the neck, and we use it routinely. Although some authors have shown good results with extensive neck lipectomy21, the senior author advises, in special cases, making a complementary excision of the subcutaneous fat under direct vision, following a conservative approach to avoid producing a concave aspect in the submental region. This step helps to better redrape the skin, being a very important aspect of the surgical procedure.
The effectiveness of the surgical procedures was evaluated by the comparison of the photographs taken before and after the procedures by two independent and experienced plastic surgeons. Most of patients were evaluated as excellent or good results. Those patients who underwent reoperation, were classified as being grade IV or V before the first procedure. The procedure used was Pitanguy's "round" face and neck lift. In the reoperation, we used atypical face and neck lift with anterior to the hairline scar (Tables 2 and 3). Patients classified as good results in group 2 probably lacked jawline definition after the procedure, because of the surgical technique utilized. One could say that not treating the SMAS and using only neck lift, was responsible for that.
In the intermediate layer of the neck there might be some degree of flaccidity of the musculoaponeurotic superficial system of the neck (plastysma muscle), with the presence of platysmal bands (because of the platysmal flaccidity) and hypertrophy of the platysmal margins. The correct preoperative diagnosis is very important to the choice of the best treatment and is crucial to achieve the best aesthetic result5,6,10,15,17-19. The medial platysmal border is sutured in the middle, from the thyroid cartilage to the submental level, using absorbable 4-0 sutures, through the submental incision of 3 to 4 cm5,10 (patients grade II, III, IV and V). In some cases, we excised a strip of muscle, tangential to the hypertrophic border of the platysma. In those patients in the groups II to V, the lateral borders of the platysma muscle are pulled and sutured with four to five absorbable 4-0 sutures, to the mastoid proeminence. We do not make transverse incisions in the platysma muscle to the level of the thyroid cartilage bulge in order to create a mobile flap7,21, because of the higher risk of skin irregularities, submandibular gland ptosis, marginal mandibular branch lesion and, after some years, the risk of hypotonia and atrophy of the muscle, with the loss of its supporting function to the subplatysmal structures. The maintenance of the muscular tone is the most important factor of stability to the neck7,10,11,18,19,22,23. We believe that the intermediate layer (platysma muscle and its fascia) is the most important structure in providing support to the neck contour. The lateral pliacture of the platysma muscle enhances the definition of the jawline and the submandibular contour24. We routinely adopt the procedure to the middle third of the face as described by Amorim14, which enhances the neck contour and the definition of the jawline24-26. It is important to make sutures to the SMAS at the face's middle third in order to better define the jawline and one must use the appropriate vectors to achieve it27.
In the present study one can observe the routine use of lateral suture of the platysma muscle, with an oblique vector, whenever there was the necessity of performing a neck and face lift (patients graded II to V). However, the suture of the medial margins of the platysma muscle was necessary only in those cases where we have observed the existence of medial platysmal bands during preoperative examination or significant loss of neck contour (patients graded II to V). The use of "corsette" sutures, transverse to the platysma muscle, previously described by Nahai, Guerreirosantos and others, were not used in the present study19,28. In the present study we have used the paramedial platysma muscle plication in order to enhance the tension over the submandibular gland, as described above.
However, aside from these alterations, one must observe other anatomical neck variants related to the aging process, such as: height of the hyoid bone; chin projection; congenital modifications of the cervicomental angle; and submandibular gland ptosis. Each one of these alterations must be addressed individually. It is not advisable to group these alterations in any classification as they appear less frequently. As Rohrich and Nahai, we do not advise the treatment of the submandibular gland ptosis or the correction of the hyoid bone height variants through surgical procedures directly over these structures, given the high complications rates and less than ideal results observed13,16,20,23,25. We prefer to use the intraplatysmal vertical suture at the level of the second premolar tooth, avoiding the risky region of the marginal mandibular branch of the facial nerve15. Sometimes we have observed that the diagnosis of submandibular gland ptosis could only be made intraoperatively.
The development of the present classification showed the possibility of grouping the aging process alterations to the neck in subgroups (I to V), being very easy to identify and differentiate common alterations, while allowing the proposition of different surgical treatments to each group of patients. In order to do that, the grouping of the neck anatomic structures in layers or lamellas, allows the surgeon to easily diagnose and visualize the affected structures, become easier to select the surgical procedure. The better the preoperative diagnosis, the better the treatment selection, and this must be individualized in order to achieve the most exquisite aesthetic results. Furthermore, this classification helps with the choice of the best treatment option in relation to the placement of the scars and the skin vectors of traction.
CONCLUSION
The classification based on neck lamellas for the aesthetic variations of the cervical region became easier to choose the most appropriate surgical treatment. Comparing the skin flaccidity, the amount of fat accumulation, muscle flaccidity and cervical contour alterations, the patients were classified into 5 groups and for each group was determined the best surgical treatment.
The final aspect obtained through the surgical procedures, that best addressed the anatomical alterations identified, were analysed by two independent and experienced plastic surgeons with excellent and good results in the majority of the cases.
REFERENCES
1. Pitanguy I. Face Lifting. In: Pitanguy I, ed. Aesthetic Plastic Surgery of Head and Body. 1st ed. Berlin Heidelberg New York: Springer-Verlag; 1981. p.165-200.
2. Thorne CH. Facelift. In: Thorne CH, ed. Grabb & Smith's Plastic Surgery. 6th ed. Philadelphia: Lippincott Williams & Wilkins; 2007. p.498-508.
3. Pitanguy I. La ritidoplastica: soluzione eclettica del problema. Minerva Chir. 1967;22(17):942-7.
4. Mitz V, Peyronie M. The superficial musculo-aponeurotic system (SMAS) in the parotid and cheek area. Plast Reconstr Surg. 1976;58(1):80-8.
5. de Castro CC. The anatomy of the platysma muscle. Plast Reconstr Surg. 1980;66(5):680-3.
6. Gardetto A, Dabernig J, Rainer C, Piegger J, Piza-Katzer H, Fritsch H. Does a superficial musculoaponeurotic system exist in the face and neck? An anatomical study by the tissue plastination technique. Plast Reconstr Surg. 2003;111(2):664-72.
7. Ellenbogen R, Karlin JV. Visual criteria for success in restoring the youthful neck. Plast Reconstr Surg. 1980;66(6):826-37.
8. Byrd HS, Burt JD. Dimensional approach to rhinoplasty: Perfecting the esthetic balance between the nose and chin. In: Gunter J, Rohrich RJ, Adams WP, eds. Dallas Rhinoplasty: Nasal Surgery by the Masters. 1st ed. St Louis: Quality Medical Publishing; 2002. p.117-31.
9. Millard DR, Pigott RW, Hedo A. Submandibular lipectomy. Plast Reconstr Surg. 1968;41(6):513-22.
10. De Castro CC. Anatomy of the neck and procedure selection. Clin Plast Surg. 2008;35(4):625-42.
11. Mottura AA. Cervical rhytidectomy. Aesthetic Plast Surg. 1999;23(3);179-88.
12. Michalany Filho S. Neck rhytidectomy: aesthetic treatment variations. Aesthetic Plast Surg. 1997;21(1):32-7.
13. Marino H, Galeano EJ, Gandolfo EA. Plastic correction of double chin. Importance of the position of the hyoid bone. Plast Reconstr Surg. 1963;31:45-50.
14. Pitanguy I, Amorim NFG. Treatment of the nasolabial fold. Rev Bras Cir. 1997;87(5):231-42.
15. Gonzalez R. Composite platysmaplasty and closed percutaneous platysma myotomy: a simple way to treat deformities of the neck caused by aging. Aesthet Surg J. 2009;29(5):344-54.
16. Rohrich RJ, Rios JL, Smith PD, Gutowski KA. Neck rejuvenation revisited. Plast Reconstr Surg. 2006;118(5):1251-63.
17. Guerrero-Santos J, Espaillat L, Morales F. Muscular lift in cervical rhytidoplasty. Plast Reconstr Surg. 1974;54(2):127-30.
18. McKinney P. The management of platysma bands. Plast Reconstr Surg. 1996;98(6):999-1006.
19. Guerrerosantos J. Managing platysma bands in the aging neck. Aesthet Surg J. 2008;28(2):211-6.
20. Connell BF, Shamoun JM. The significance of digastric muscle contouring for rejuvenation of the submental area of the face. Plast Reconstr Surg. 1997;99(6);1586-90.
21. Pita PCC, Azevedo SFD, Cabral PO, Pessoa de Melo SRP. Lifting cervical gravitacional. Rev Bras Cir Plást. 2010;25(2):291-6.
22. Connell BF. Contouring the neck in rhytidectomy by lipectomy and a muscle sling. Plast Reconstr Surg. 1978;61(3):376-83.
23. Graf R, Neto LG, Araújo LR, Bernardes A, Rippel R, Auersvald A. Vertical vectors in SMASectomy to reshape the aging face. Aesthet Surg J. 2003;23(3):198-201.
24. Baker DC. Minimal incision rhytidectomy (short scar face lift) with lateral SMASectomy: evolution and application. Aesthet Surg J. 2001;21(1):14-26.
25. McKinney P, Tresley GE. The "maxi-SMAS": management of the platysma bands in rhytidectomy. Ann Plast Surg. 1984;12(3):260-7.
26. Riascos A, Baroudi R. Ritidoplastia sem cicatriz periauricular. Rev Bras Cir Plást. 2012;27(2):260-5.
27. Letizio NA, Anger J, Baroudi R. Ritidoplastias: smasplastia cervicofacial mediante sutura de vetores. Rev Bras Cir Plást. 2012;27(2):266-71.
28. Nahai F. Reconsidering neck suspension sutures. Aesthet Surg J. 2004;24(4):365-7.
1. Member holder SBCP - Preceptor of the Ivo Pitanguy Institute Member SBCP holder
2. Preceptor of the Ivo Pitanguy Institute and Coordinator of the Research Department of the Ivo Pitanguy Institute
3. Plastic Surgeon, member of the BSPS, and AExPI ISPRES - Plastic Surgeon in Private Practice
4. General Surgeon - Surgeon in private practice
Charles de Sá, M.D.
Clínica Performa
R. Joana Angélica, number 124, 602
Rio de Janeiro, RJ, Brazil ZIP code 22420-030
Article received :10/05/2013
Article accepted :05/10/2013
work performed at the Clínica Performa , Rio de Janeiro, RJ, Brazil


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter