

Original Article - Year 2013 - Volume 28 -
Un unprecedent auricular reconstruction
Uma reconstrução auricular sem precedentes
ABSTRACT
INTRODUCTION: As auricular reconstruction is a very difficult procedure, patients are unfortunately sometimes found in doctor's surgeries who have previously been operated on with disastrous results that are impossible to correct or improve upon with known methods. Some of these patients accept the result achieved, while others do not and thus seek a better solution. What is to be presented now cannot be found in other publications and may be added to the specialty's arsenal as a new method. This work focuses on a twenty-one-year-old patient born with microtia on the right side who, between the age of six and the day of their consultation, had undergone twenty-five unsuccessful operations.
CASUISTRY AND METHOD: Only one case was operated on and the method consisted of the transfer of all the retroauricular skin from the left ear in order to cover the right auricular region and thus create an ear. The fingertips of the 2nd and 3rd fingers of the right hand were used as vectors.
RESULT: The author had a satisfactory result within the desired expectations.
CONCLUSION: It is possible to use fingertips as a vector for the transfer of auricular flaps for complicated cases of auricular or facial reconstruction.
Keywords: Otoplasty, Microtia, Flaps, Vectors.
RESUMO
INTRODUÇÃO: Por ser a reconstrução auricular um procedimento muito difícil, infelizmente encontram-se nos consultórios alguns pacientes já operados e com resultados desastrosos, impossíveis de serem corrigidos ou melhorados com os métodos já conhecidos. Alguns pacientes se conformam com o resultado conseguido, mas outros não e procuram uma melhor solução. O que vai se apresentar agora não consta em outras publicações e pode ser incluído no arsenal da especialidade como método novo. Este trabalho trata de um paciente, 21 anos, que nasceu com microtia do lado direito, que desde os 6 anos, até o dia da consulta, já tinha sido submetido a vinte e cinco operações, sem sucesso.
CASUÍSTICA E MÉTODO: Um caso, que foi operado, cujo método consistiu em transferir toda a pele retroauricular da orelha esquerda, para cobrir a região auricular direita, fazendo assim uma orelha. Usaram-se como vetores as polpas dos dedos 2º e 3º da mão direita.
RESULTADO: O autor ficou satisfeito com o resultado alcançado.
CONCLUSÃO: É possível usar as polpas digitais como vetor para transferir retalhos auriculares para casos complicados de reconstrução auricular ou facial.
Palavras-chave: Otoplastia, Microtia, Retalhos, Vetores.
During his surgical practice, the author encountered a 21-year-old patient who was born with microtia of the right ear. The entire right auricular, peri-auricular, and cervical areas; scalp; thorax (both sides); and right scapular region had scars resulting from previous attempts at reconstruction (Fig. 1A, 1B, 1C).

Fig.1.A 21-year-old male patient who had undergone 25 procedures to correct microtia.

Fig.1.B Multiple scars in the auricular and periauricular areas, face, scalp, and scapular area.

Fig. 1.C Scars in the right scapular area and the scalp.
When the patient was 6 years old, an otolaryngologist created an external auditory canal in the patient. Later, a plastic surgeon, experienced in the field, performed reconstruction of the ear with a costal cartilage. Some months later, cartilage exposure, infection, and total loss occurred. Back in his hometown, the patient visited another surgeon who also decided to perform reconstruction by using the costal cartilage from the other hemithorax. This second attempt was also not successful as extrusion occurred.
With time, the patient received expanders and was subjected to two new consecutive interventions, performed by the same surgeon: in the first procedure, a silicone implant was used, designed almost half a century ago by Cronin (1); in the second procedure, an implant idealized by Arrunátegui was used. Both interventions were unsuccessful. Subsequently, the patient was advised to consult an odontology faculty. Here, a silicone ear was glued to his skin, which after few days, became detached, resulted in a torn epithelium, and a bleeding wound. The same faculty proposed placing an osteo-integrated Brånemark prosthesis, but the patient refused. Because he already has many scars, he felt discouraged, and with all possibilities of auricular reconstruction exhausted, he decided to wear a type of skin-colored paper prosthesis that he himself had manufactured several years before (Fig. 2).
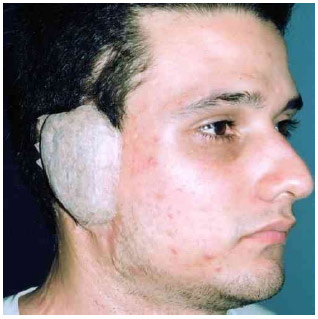
Fig.2 Paper prosthesis manufactured by the patient.
The years passed until someone referred the patient to consult the author of this work. The author told the patient that, unfortunately, he had no solution to offer because all the possibilities had already been tried. The patient was very insistent that the author attempts some solution, as he did not wish to remain without an ear at the age of 21 years. The author asked for a week to study the case. Luckily, all the retroauricular skin and temporal-parietal fascia of the left ear had been completely spared. Because the author had many years of surgical experience with vascularization of the finger pulps and transfer of small flaps, he proposed to the patient and his mother that, the retroauricular skin of the left side could be transferred to the right side by using the finger pulps as vectors, in order to cover the entire affected area on the right side. Thus, there would be material to reconstruct the ear (2-4).
METHODS
All the skin in left ear that could be used and a small area of the scalp for the transfer were defined, with care to avoid deforming them.
First surgical stage. With the patient sedated and under local anesthesia, the area on the right side was improved by removing the remaining costal cartilage tissue from the previous operations.
Two right-hand finger pulps were selected (second and third fingers), with the hand, arm, and head in a comfortable position for the patient at the time of transfer (Fig. 3).
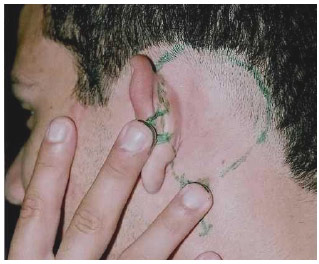
Fig.3.Defining the skin of the left retroauricular area that could be used to reconstruct the right side. The pedicles for the flap were drawn at the height of the third and fourth finger pulps.
With the patient in this position, large pedicles were drawn, and the flap to be transferred was delimited; it was ensured that the flap was not small relative to the receiving area. The incision was drawn in the vector fingers, in the shape of an alligator's mouth, 3 or 4 mm from the nails. Local anesthesia was extended to the fingers and retro-auricular area, and the surgery was initiated.
The pedicles were confectioned to be inserted into the finger pulps; they were 1-cm wide and 0.5-cm long, with maximum thickness. The epithelial side of the tiny flaps was scraped with a scalpel until light bleeding was observed.
Vascular delay of the flap was performed by making incisions with a scalpel, leaving three untouched sites to ensure effective blood supply to the flap. Before suturing the incisions of the vascular delay, in-depth detachment of the flap (with the maximum thickness possible) was performed (exceeding all its edges by 1 cm).
A thin silicone sheet (score 50-0.50) was placed over the entire detached area of the flap as well as one drain of the same material, to avoid flap revascularization (Fig. 4).

Fig 4. Thin silicone sheet being placed under the flap.
The incisions made for the vascular delay of the flap were sutured with nylon 5-0. Incisions were made in the pulps 4 mm from the nails, where the pedicles would be sutured.
The right hand was placed near the left auricular area while the patient was awake and collaborating, and the pedicles were sutured inside the finger pulps with nylon 5-0. Small grafts of thin skin from the scalp were placed in the exposed bloody areas of the pedicles. Nylon 4-0 stitches were loosely placed between some fingers and the scalp to immobilize the compromised parts.
Intermediate treatment was performed by dripping antibiotic on the pedicles.
Second surgical stage: vascular delay. At day 5, under local anesthesia, another vascular delay of the flap was performed on the sides that had not been sectioned previously. The flap's vascular response was good. Further treatment was made by dripping gentamicin.
Third surgical stage: flap transfer. The initial plan was to perform the transfer of the flap at 10 days; however, because this was the first time that this technique was used, it was deemed safer to perform the transfer at 15 days, although the flap showed good blood flow. As flap vascularization was apparently good, the flap's margins were sectioned, and the flap was left attached only to the fingers' pedicles while the patient was under local anesthesia and sedation (Fig. 5A).

Fig. 5A . Transfer of the flap attached only to the fingers. Difficult venous return was observed.
At this point, one-third of the silicone sheet had folded, possibly because it was too thin and poorly placed, which allowed involuntary revascularization of the flap within its bloody bed, giving the surgeon the false impression of good blood flow in the flap. The occurrence of this imperfection in the vascular delay led to difficult venous return in the flap. The right hand with the flap attached to the fingers was moved to the right side (Fig. 5B).

Fig 5B . Placement and suture of the flap in the right auricular area where the flap would be sutured.
The patient agreed to undergo more procedures; the flap was placed in the receiving area, and the area of the suture was marked with a marker. The skin of the auricular area and the scars were removed as much as possible, ensuring that the flap's margins were sutured to the edges that were in good condition (i.e., without scars); a small area of the scalp was invaded. The suture was performed using nylon 5-0 (Fig. 6).

Fig.6. A flap sutured in the receiving area of the cyanosed segment.
A graft of intermediate thickness from the abdomen was placed in the large, bloody, left retroauricular area.
On the following day, the nylon stitches were removed 2 cm from the margin, in the most cyanosed area, to correct venous stasis. The flap was massaged gently to eliminate the accumulated venous blood. For the drainage to be more effective, the edge of the flap was gently scraped and light pressure was applied using the fingers. This maneuver was performed thrice a day for 3 days until the flap's dark color disappeared.
The initial plan was to section the pedicles of the fingers after 10 days; however, because of venous stasis, it was deemed safer to resect the fingers 15 days after the transfer. The flap exhibited good blood flow after the pedicles were sectioned; however, there was loss of epithelium in the distal part (Fig. 7).

Fig 7. Seven days after pedicle sectioning. Light degeneration in the flap margins was observed.
Betamethasone dipropionate with gentamicin sulfate was applied on the flap for 1 month.
Fourth surgical stage. At 8 months, once the new skin in the auricular area was soft, a silicone auricular implant (model Arrunátegui) was placed underneath (Fig. 8).

Fig 8. Soft skin marked for implant placement.
Because the skin exhibited some fibrosis in the deepest plane, the ear's convolutions were not ideal. Therefore, after 3 months, new incisions had to be made at the site of the depressions to implant skin grafts and thus, improve the ear's appearance.
Fifth surgical stage. Ten months later, a fairly limited ear lift was performed by placing a supra-inguinal skin graft (Fig. 9A, 9B).

Fig.9A Before the start of the reconstruction .

Fig.9B. Definitive postoperative appearance 3 years after the start of the reconstruction.
Sixth surgical stage. Because the left ear was protruding relative to the reconstructed right ear, the left ear was corrected (Fig. 10A, 10B).
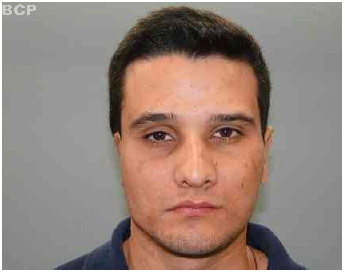
Fig.10A. Protruding left ear.

Fig.10B. After the correction.
DISCUSSION
Auricular reconstruction is a very difficult procedure. Currently, the most frequently used technique is reconstruction with a costal cartilage; however, this is the most invasive method in plastic surgery. According to many surgeons, approximately 70% of procedures of this type are performed with material from the thorax, which increases the number of complications because the surgeon removes three or four costal cartilages to sculpt and bind the fragments to form the skeleton of the new ear. Despite these great challenges, this case was resolved by using only an industrially manufactured a silicone implant that was sterilized.
The patient was very insistent that the surgeon finds a solution. The author proposed a possibility but suggested to the patient and his family to take 1 week to reflect on the possible complications. After this period, the patient and his family accepted the proposed surgery.
Because the left retroauricular area was the only adequate source of skin that had been left completely untouched, the surgeon proposed to transfer this entire area to the right side so that he could use this excellent-quality and highly vascularized skin to perform the auricular reconstruction so that patient could stop wearing the micropore "prosthesis" that he had confectioned and worn for many years.
This skin transfer was inspired by the author's knowledge of the surprising vascular richness of finger pulps, which has been extensively studied by Reinisch (2) and Daniels (3). These authors highlighted the abundance of arteriovenous anastomoses at the capillary level. When a finger pulp is placed above the forearm, it is possible to observe a strong red color in the pulp when compared with the pale skin of the forearm, which confirms appropriate vascularization. In addition, the mean flow in the fingers is 20-30 times the minimum blood flow that occurs during intense vasoconstriction and can increase up to 100 times during vasodilatation.
The above-mentioned two studies inspired the author to use finger pulps as vectors for quickly transferring the small flaps. The hypothenar flap of the opposite hand was used to reconstruct the amputated pulps. In these cases, the two hands were joined and immobilized, and the successful sectioning of the pedicle could be done in only 3 or 4 days owing to the vascularization of the compromised parts (4).
After receiving an extensive explanation of the proposed surgery, the patient and his family considered the surgery because they thought that the result would be better than result from wearing the paper "prosthesis", even after they were aware that this is the first such operation.
Initially, the plan was for the pedicles of the retroauricular skin to remain grafted to the fingers for only 10 days, to allow the rich vascular supply of the finger pulps to nourish the flap; however, because this was the first case and the patient had agreed to retain the flap for 5 more days, the hand with the flap was only separated 15 days after the transfer was initiated. The patient agreed to this because it was easier to maintain the position of the hand attached to the head for 15 days than enduring the cross-legged position with attached tubes, as had been done during previous procedures. As this was the first case of its kind, there could be unforeseen developments that would compromise the flap's vitality, some of which were, in fact, observed during the transfer. Therefore, waiting for a few more days proved to be a good decision, as the flap was not lost. In this operation, the following flaws were observed:
1 - The silicone sheet placed between the flap and its bed, was very thin and folded spontaneously, leading to unwanted revascularization of the flap in some areas. Moreover, the silicone sheet should have been placed under the pedicles.
2 - The flap should have been further detached, by at least 7 mm, for better entry of the silicone sheet and to safely avoid revascularization of the flap from its bed.
3 - The pedicles that are inserted into the finger pulps should be thick, and the epithelium should be scraped with a scalpel with great care to achieve a larger bloody area to facilitate revascularization from the finger pulp.
4 - The bloody parts of the pedicles that remain exposed should be covered with thin scalp grafts. After the pedicles were sutured to the finger pulps, the physiological position of the fingers (slight flexion relative to the hand) caused the pulps to apply light pressure to the deep tissues, which probably hindered the revascularization of the flap. Therefore, the author believes that the most comfortable and ideal position for the hand and fingers is that shown in Fig. 11.
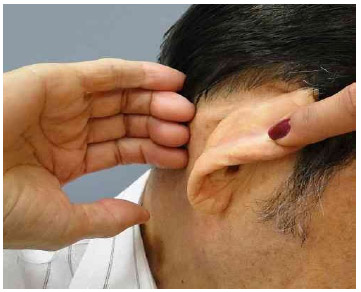
Fig.11. Proposed position of the hand and fingers for future similar cases.
The aforementioned limitation led to venous stasis in the flap, which was reversed by removing five stiches from the most compromised part and by scraping the wound and draining the area of stasis by gently massaging the tissue every 8 h for 3 days.
Once the flap was integrated, and because the skin exhibited fibrosis at the base, the auricular silicone implant was only placed after 8 months.
The right ear showed protrusion after the reconstruction. The left ear, however, showed protrusion, and the patient requested the surgeon to correct the false flappy ear.
CONCLUSION
In cases in which complications occur after unsuccessful operations, it is still possible to reconstruct the ear by transferring ear flaps by using the fingers as vectors. In addition, it is possible to extend the indication of this technique to the reconstruction of other parts of the face.
REFERENCES
1. Shaw GM, Carmichael SL, Kaidarova Z, et al. Epidemiologic characteristics of anotia and microtia in Califórnia, 1989-1997. Birth Defects Res 70(7):472, 2004.
2. Wildervanck LS. Hereditary malformations of the ear in three generations: marginal pits, preauricular appendages, malformations of the auricle and conductive deafness. Acta Otolaryngol 54:553, 1962.
3. Tanzer RC. Total reconstruction of the auricle: the evolution of a plano f treatment. Plast Reconstr Surg 47:523, 1971.
4. Brent B. Technical advances in ear reconstruction with autologous rib cartilage grafts: personal experience with 1200 cases. Plast Reconstr Surg 104:319, 1999.
5. Nagata S. Modification of the stages in total reconstruction of the auricle: Part I. Grafting the three-dimensional costal cartilage framework for lobule-type microtia. Plast Reconstr Surg 93:221, 1994.
6. Nagata S. Modification of the stages in total reconstruction of the auricle: Part II. Grafting the three-dimensional costal cartilage framework for concha-type microtia. Plast Reconstr Surg 93:231, 1994.
7. Nagata S. Modification of the stages in total reconstruction of the auricle: Part III. Grafting the three-dimensional costal cartilage framework for small concha-type microtia. Plast Reconstr Surg 93:243, 1994.
8. Bauer BS. Reconstruction of microtia. Plast Reconstr Surg 124:14e, 2009.
9. Firmin F, Sanger C, O'Toolr G. Ear reconstruction following severe complications of otoplasty. J Plast Reconstr Aesthet Surg 61:s13, 2008.
Post-graduate-plastic surgeon at the Hospital Belvedere
Article received: 26/02/2013
Article accepted: 27/03/2013
work performed at the Hospital Belverede


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter