

Original Article - Year 2013 - Volume 28 -
Neoadjuvante chemotherapy and immediate breast reconstruction: a good option?
Quimioterapia neoadjuvante e reconstrução mamária imediata: uma boa opção?
ABSTRACT
BACKGROUND: The combination of neoadjuvant chemotherapy and immediate breast reconstruction is a field under discussion. There are doubts whether the association of events could result in an increase of postoperative complications in patients undergoing the surgical procedure.
METHODS: Retrospective study of patients who underwent immediate breast reconstruction from January 2010 to January 2012. Patients submitted to neoadjuvant chemotherapy were compared with those who had not receive any form of chemotherapy and those who received adjuvant chemotherapy.
RESULTS: Fifty-four patients were selected, totalizing 71 immediate breast reconstructions. Thirteen patients received neoadjuvant chemotherapy (15 reconstructions) twenty-three patients did not receive chemotherapy (33 reconstructions) and eighteen received adjuvant chemotherapy (23 reconstructions). Minor complications occurred in 33.3% of breast reconstruction in the group undergoing neoadjuvant therapy. There were 6.7% major complications in the same group. There was no statistical differences in the number of minor and major complications between groups.
CONCLUSION: In the series analyzed, the use of neoadjuvant chemotherapy did not increase the number of postoperative complications in patients undergoing immediate breast reconstruction.
Keywords: Breast cancer. Mastectomy. Mammaplasty. Chemotherapy. Postoperative complications. Reconstructive.
RESUMO
INTRODUÇÃO: A combinação de quimioterapia neoadjuvante e reconstrução mamária imediata é um campo em discussão. Há dúvidas se a associação dos eventos poderia resultar em um aumento de complicações pós-operatórias nas pacientes submetidas ao procedimento cirúrgico.
MÉTODOS: Estudo retrospectivo de pacientes submetidas à reconstrução mamária imediata entre janeiro de 2010 e janeiro de 2012. As pacientes submetidas à quimioterapia neoadjuvante foram comparadas com as que não receberam qualquer forma de quimioterapia e com as que receberam quimioterapia adjuvante.
RESULTADOS: Cinquenta e quatro pacientes foram selecionadas, totalizando 71 reconstruções mamárias imediatas. Treze pacientes receberam quimioterapia neoadjuvante (15 reconstruções), vinte e três pacientes não receberam quimioterapia (33 reconstruções) e dezoito receberam quimioterapia adjuvante (23 reconstruções). Complicações menores ocorreram em 33,3% das reconstruções mamárias no grupo submetido à neoadjuvância. Houve 6,7% de complicações maiores no mesmo grupo. Não houve diferenças estatísticas no número de complicações menores e maiores entre os grupos.
CONCLUSÃO: Na série analisada, o emprego da quimioterapia neoadjuvante não resultou em aumento do número de complicações pós-operatórias nas pacientes submetidas à reconstruções mamárias imediatas.
Palavras-chave: Câncer de mama. Mastectomia. Reconstrução mamária imediata. Quimioterapia neoadjuvante. Complicações pós-operatórias.
Historically, breast cancer therapy consisted of mastectomy followed by adjuvant treatments such as chemotherapy, radiotherapy, and/or hormone therapy. Breast reconstruction procedures were only performed subsequently, frequently after 5 years of follow-up1.
However, in the last decades, this practice has been changing, with regard to the timing of reconstruction as well as the sequence of additional treatments.
Immediate reconstruction, conducted at the same time as mastectomy, is being increasingly performed. It has been shown to be beneficial in reducing morbidity (decreasing the number of surgical interventions and recovery time), reducing psychological and social impacts, improving the aesthetic outcome, and increasing the satisfaction of patients about the treatment, without affecting oncological safety1,8.
Chemotherapy has begun to be increasingly used by oncology and mastology teams, as this therapy has been shown to be efficient in reducing the recurrence and mortality of breast cancer, mainly by eliminating or delaying the development of occult micrometastases8.
Meanwhile, the timing of chemotherapy has also undergone changes. For patients with locally advanced breast cancer, inoperable cancer, or inflammatory breast cancer, chemotherapy conducted before the surgical procedure (neoadjuvant chemotherapy) has been considered as the standard treatment. In addition to the benefits already described, chemotherapy allows testing the efficacy of the drug used, and when the patient is responsive, chemotherapy allows the reduction of tumor size, which enables surgery with higher preservation of the skin envelope and facilitates the reconstruction process3,4.
However, although there are many studies in the literature about this topic, the combination of neoadjuvant chemotherapy and immediate reconstruction remains under discussion.
There are doubts about whether the cytotoxic drugs used in chemotherapy and the timing of their application could produce local or systemic adverse effects, affecting the surgery, increasing the incidence of postoperative complications, and resulting in the failure of reconstruction in patients undergoing immediate reconstruction.
OBJECTIVE
To evaluate the rate of complications in patients undergoing neoadjuvant chemotherapy followed by mastectomy and immediate breast reconstruction, when compared with patients not undergoing chemotherapy or those undergoing adjuvant chemotherapy.
METHODS
A retrospective review of records was conducted for patients who underwent breast reconstruction from January 2010 to January 2012. Fifty-four patients whose reconstructions were conducted at the same time as the mastectomy were selected.
All patients signed the written informed consent form, authorizing the use of their data and treatment information, as well as their photographs, for scientific purposes.
The recommendation of chemotherapy and the timing of chemotherapy (when recommended) were decided by the clinical oncologist, on the basis of the histological characteristics, immunohistochemical characteristics, and tumor stage of each patient.
All reconstructions were performed by the same surgeon. The method of reconstruction performed was selected on the basis of a thorough analysis of the case by the assistant plastic surgeon, along with the personal preference of the patient. All patients were followed-up for at least 5 months postoperatively.
The patients were divided into three groups: those who received neoadjuvant chemotherapy (group 1), those who did not receive chemotherapy (group 2), and those who received adjuvant chemotherapy (group 3).
The characteristics analyzed were age, presence of comorbidities, tumor characteristics, reconstruction methods used, and observed complications.
Minor complications were defined as the presence of seroma, hematoma, small areas of dehiscence, and epidermolysis. Major complications were defined as infection, necrosis, and pulmonary thromboembolism.
Patients who received neoadjuvant chemotherapy (group 1) were compared with patients who did not receive any form of chemotherapy (group 2) and with those who received adjuvant chemotherapy (group 3).
The results were analyzed with statistical tests (e.g., analysis of variance, Levene, chi-square, and Kruskal-Wallis), and the results were considered significant when P < 0.05.
RESULTS
Fifty-four patients were selected, comprising a total of 71 immediate reconstructions, with 13 patients allocated to group 1, 23 to group 2, and 18 to group 3.
The ages of the analyzed patients were from 28 to 73 years (mean, 51.2 years).
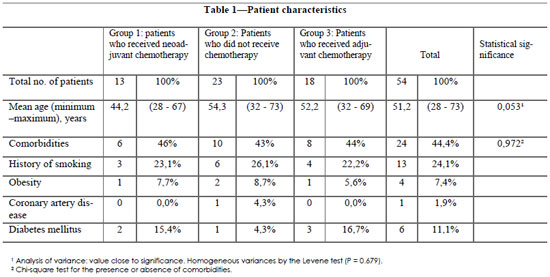
Approximately 44.4% of the patients had some type of comorbidity, such as history of smoking, obesity, coronary artery disease (previous myocardial revascularization), or diabetes mellitus.
The groups were considered homogeneous in both age and the presence of comorbidities, according to the statistical tests performed.
The detailed analysis of the patients' characteristics and their distribution in each of the groups is described in Table 1.
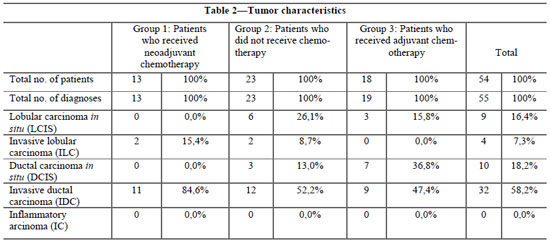
A total of 55 breast neoplasia diagnoses were made, and none of the patients had a diagnosis of bilateral neoplasia. The main histologic types found were invasive ductal carcinoma (58.2%) and ductal carcinoma in situ (18.2%). Cases of inflammatory carcinoma were not observed.
The detailed analysis of tumor characteristics is described in Table 2.
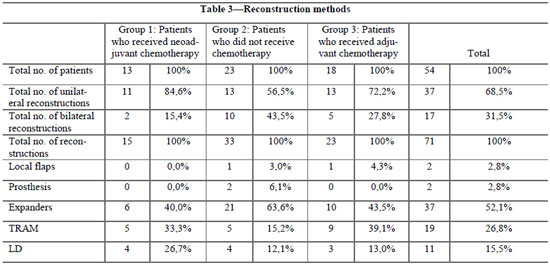
The methods of reconstruction involved the use of local flaps, prosthesis, expanders, myocutaneous flap from the rectus abdominis muscle (TRAM), and myocutaneous flaps from the latissimus dorsi muscle associated with the prosthesis (LD).
Concerning the method of reconstruction, 68.5% of patients underwent unilateral reconstruction and 31.5% underwent bilateral reconstruction. The main method used when all the groups were analyzed was the use of an expander (52.1%), followed by TRAM (26.8%) and LD (15.5%).
The detailed analysis of the reconstruction methods used in each group is described in Table 3.
A mean percentage of 38% reconstructions with complications was observed. In the evaluation of minor complications, the mean incidence was 25.4%, reaching up to 33.3% in group 1. Among the major complications, the mean incidence was 12.7%, being higher in group 3 (21.7%).
The incidence of complications, regardless of severity, was not significant between the groups (P = 0.407). Statistically significant differences were not found between minor and major complications. (P = 0.667 and P = 0.280).
The detailed analysis of the observed complications in each studied group and its respective percentages is described in Table 4, and in Figures 1 and 2.
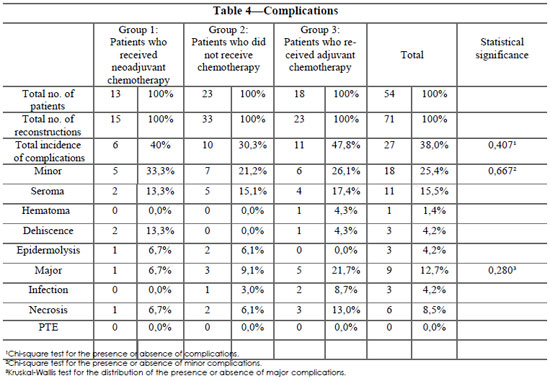

Fig. 1 - Patient with dehiscence and infection in the right immediately reconstructed breast that required the removal of the expander and a subsequent secondary breast reconstruction.

Fig. 2. Patient with necrosis in the reconstructed right breast .
DISCUSSION
The World Health Organization estimates that every year, >1 million of new cases of breast cancer occur worldwide, which makes this cancer the most common among women9. According to data from the Ministry of Health, the situation is similar in Brazil9.
In light of the aging population in Brazil and the higher prevalence of the risk factors for this condition, there is a tendency for an increase in the incidence of the breast cancer in the country. However, the mortality rate of breast cancer in Brazil is stable, despite being high10,11.
This is mainly attributed to improvements in the diagnosis and therapeutics of the disease, which have allowed earlier diagnoses and treatments that are increasingly more effective.
In Brazil, the guidelines for screening the disease are determined by the Ministry of Health, which recommends an annual clinical breast examination for women from the age of 40 years, and a mammography examination every 2 years in women aged 50 to 69 years9,12. For women from population groups considered to be at high risk for breast cancer (family history of breast cancer in first-degree relatives before 50 years of age, family history of bilateral breast or ovarian cancer in first-degree relatives at any age, family history of male breast cancer, histopathological diagnosis of atypical proliferating mammary lesion or in situ lobular neoplasia), clinical breast examination and mammography annually from the age of 35 years are recommended9,10 .
There are two alternatives for the surgical treatment of mammary neoplasia: conservative surgery or total mastectomy. Factors that direct the decision for one or the other approach include the size of the tumor, multicentricity, breast volume, and genetic predisposition to the disease13. The oncologic treatment may still be multidisciplinary, in which there might be a need for complementation with radiotherapy, chemotherapy, and hormone therapy.
Plastic surgery has also changed, accompanying the changes seen in the diagnosis and therapy of breast neoplasia during the last decades. New methods of reconstruction have been proposed, with optimized results being achieved along with a considerable increase in the expectations of patients.
However, diverse factors can interfere in the process of breast reconstruction and affect the results of this treatment.
The increase in postoperative morbidity among patients undergoing immediate mammary reconstruction is closely related to the previous conditions of the patients, such as age, history of smoking, obesity, arterial hypertension, and diabetes mellitus1,5.
In our work, the studied groups were homogenous from the statistical point of view with regard to the variables studied.
Regarding the histologic type, we observed a higher percentage of patients with ductal carcinoma in our cases, which was expected as this is the most prevalent subtype.
When we analyzed the breast reconstruction methods, we verified that the use of an expander was the main method used by our team, with >50% of cases being reconstructed in this manner.
We attributed this fact mainly to the increasing tendency for an early diagnosis of breast cancer, which allows mastectomies that preserve the skin and allows reconstruction with the use of silicone implants/tissue expanders. Furthermore, we believe that the diagnosis of mammary neoplasia performed in ever younger patients (commonly with restricted donor sites because of the desire to become pregnant in the future, engaging in regular physical activity, and having undergone a previous aesthetic abdominal surgery) decrease the possibilities of reconstruction by using autologous flaps in isolation.
Another important factor about this issue is the increasing number of bilateral mastectomies conducted by mastologists in this subgroup of young patients (because of a more potentially aggressive disease, possible genetic causes, and the possibility of new diagnosis of contralateral neoplasia in the future). In our statistical study, there was a need for bilateral reconstruction in approximately 31% of cases.
Although bilateral reconstruction is still controversial in the literature, we noted that this practice is used with some frequency, which hinders even more the possibilities of reconstruction with uniquely autologous flaps.
Most studies concerning complementary therapy indicate that conducting chemotherapy, either neoadjuvant or adjuvant, does not seem to increase the risk of complications and failures in immediate breast reconstruction8.
However, this is controversial. Given the impact of chemotherapy on the patient and its potential local and systemic cytotoxic effects, the combination of surgery and neoadjuvant chemotherapy could result in an increase in the number of complications and failures in patients submitted to immediate breast reconstruction6,7. Some studies suggest that the combination of these processes could cause cicatrization problems in wounds and postoperative infections, causing failures in the reconstruction, mainly when implants are used.
This fact becomes extremely important, because reconstruction with implants is more frequently used in the Brazilian population.
Although several studies have investigated immediate breast reconstruction in the Brazilian literature, we could not find any study that correlates neoadjuvant chemotherapy and the possible complications arising from the process. We believe that we are pioneers in tackling the topic in the country.
In our analysis, there was no statistically significant increase in the number of complications in patients who received neoadjuvant chemotherapy when compared with those who did not receive any form of chemotherapy, or those who received adjuvant chemotherapy. This applies not only to the analysis of the total number of complications but also after subdivision into minor and major complications.
We believe that the reason for this result was that patients who received neoadjuvant chemotherapy underwent surgery only after a period of bone marrow recovery, and when their immunity had reached a minimum safety level, initiating an increasing curve of recovery and decreasing the chances of postoperative infection.
When we compared these groups of patients (potentially of higher risk) with those who underwent surgery and only subsequently underwent chemotherapy, we found that the lower-immunity condition that occurs at each cycle of medication may compromise the safety of the reconstruction, particularly for patients who received reconstruction with implants.
CONCLUSIONS
A surgeon who performs breast reconstruction should be familiar with the recommendations, mechanisms of action, and possible collateral effects of conducting neoadjuvant chemotherapy.
In our sample of cases, neoadjuvant chemotherapy, when associated with immediate breast reconstruction, did not result in increase in complications. Therefore, we conclude that these are not incompatible procedures and that they can be used together.
This result might be due to the number of young patients studied, which makes our results valid; however, a follow-up is needed to make definitive conclusions and validate our results. The present study serves as a basis for further analysis concerning this topic.
REFERENCES
1- Warren Peled A, Itakura K, Foster RD, Hamolsky D, Tanaka J, Ewing C, et al. Impact of chemotherapy on postoperative complications after mastectomy and immediate breast reconstruction. Arch Surg. 2010;145(9):880-5.
2- Mitchem J, Herrmann D, Margenthaler JA, Aft RL. Impact of neoadjuvant chemotherapy on rate of tissue expander/implant loss and progression to successful breast reconstruction following mastectomy. Am J Surg. 2008;196(4):519-22.
3- Zweifel-Schlatter M, Darhouse N, Roblin P, Ross D, Zweifel M, Farhadi J. Immediate microvascular breast reconstruction after neoadjuvant chemotherapy: complication rates and effect on start of adjuvant treatment. Ann Surg Oncol. 2010;17(11):2945-50.
4- Hu YY, Weeks CM, In H, Dodgion CM, Golshan M, Chun YS, et al. Impact of neoadjuvant chemotherapy on breast reconstruction. Cancer. 2011;117(13):2833-41.
5- Pinsolle V, Grinfeder C, Mathoulin-Pelissier S, Faucher A. Complications analysis of 266 immediate breast reconstructions. J Plast Reconstr Aesthet Surg. 2006;59(10):1017-24.
6- Azzawi K, Ismail A, Earl H, Forouhi P, Malata CM. Influence of neoadjuvant chemotherapy on outcomes of immediate breast reconstruction. Plast Reconstr Surg. 2010;126(1):1-11.
7- Gouy S, Rouzier R, Missana MC, Atallah D, Youssef O, Barreau-Pouhaer L. Immediate reconstruction after neoadjuvant chemotherapy: effect on adjuvant treatment starting and survival. Ann Surg Oncol. 2005;12(2):161-6.
8- Oh E, Chim H, Soltanian HT. The effects of neoadjuvant and adjuvant chemotherapy on the surgical outcomes of breast reconstruction. J Plast Reconstr Aesthet Surg. 2012;65(10):e267-80.
9- Brasil. Ministério da Saúde. Instituto Nacional de Câncer. Controle do câncer de mama: documento de consenso. Rio de Janeiro: INCA; 2004.
10- Fonseca LAM, Eluf-Neto J, Wunsch Filho V. Tendências da mortalidade por câncer nas capitais dos estados do Brasil entre 1980-2004. Rev Assoc Med Bras. 2010;56(3):309-12.
11- Freitas R Jr, Siqueira LB, Carrijo EN, Lacerda RP, Paulinelli RR, Rahal RM, et al. Temporal variation of breast cancer surgical treatment in a university hospital in Brazil's Central West region. Rev Col Bras Cir. 2013;40(3):180-5.
12- Brasil. Ministério da Saúde. Estimativa 2012: incidência de câncer no Brasil. Rio de Janeiro: INCA; 2011. 118p.
13- Piñero Madrona A. Surgical treatment of breast cancer in young women. Breast Cancer Res Treat. 2010;123 Suppl 1:21-4.
1. Full member of the Brazilian Society of Plastic Surgery (SBCP); plastic surgery physician and lecturer at the Plastic Surgery Service, Daher Lago Sul Hospital (HDLS), Brasília, DF, Brazil
2. Aspiring member of the SBCP; resident physician at the Plastic Surgery Service, HDLS, Brasília, DF, Brazil
3. Full member of the SBCP; principal physician at the Plastic Surgery Service, HDLS, Brasília, DF, Brazil
4. Full member of the SBCP; plastic surgery physician and lecturer at the Plastic Surgery Service, HDLS, Brasília, DF, Brazil
5. Associate member of the SBCP; plastic surgery physician and lecturer at the Plastic Surgery Service, HDLS, Brasília, DF, Brazil
Bruno Peixoto Esteves
Hospital Daher Lago Sul
SHIS QI 7, Conjunto F - Lago Sul
CEP: 71615-570. Brasília, DF, Brasil
E-mail: brunopeixotoesteves@outlook.com
Article received: 30/09/2013
Article accepted: 30/10/2013
Work was performed at the Plastic Surgery Service of the Daher Lago Sul Hospital, Brasília, DF, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter