

Original Article - Year 2014 - Volume 29 -
Plication and reinsertion of the aponeurosis of the lifting muscle of the upper eyelid with continuous suture in the surgical correction of light and moderate eyelid ptosis - personal experience
Plicatura e reinserção da aponeurose do músculo levantador da pálpebra superior com sutura contínua na correção cirúrgica da ptose palpebral leve e moderada-experiência pessoal
ABSTRACT
INTRODUCTION: Blefaroptose or eyelid ptosis is characterized by the anomalous positioning of the upper eyelid in relation to its normal position, which is 1 to 2 mm below the upper margin of the iris. It can vary from a slight descent to a total occlusion of the eyelid slit. In general, whether caused by a muscular or nerve deficiency, congenital or acquired, it results in the impossibility to use the muscle to raise the eyelid. It can also occur due to the detachment of the aponeurosis. Presented in this study is the tactic of continuous suture of the aponeurosis of the lifting muscle at the tarsus or at its foldings, for the treatment of light or moderate ptosis.
METHODS: In the period from 2006 to 2012, we analyzed 26 eyelids submitted to surgical treatment. 24 were operated upon, addressing the aponeurosis of the raising muscle with a shortening in the relation of 4:1 and, in 2 cases, with the reinsertion of the aponeurosis in the raising muscle of the eyelid, using continuous two-way suture completing the same with a stitch in a figure eight.
RESULTS: In 88.32% of the cases, the results were considered good, and in 11.68% satisfactory.
Keywords: Blepharoplasty; Eyelid ptosis; Congenital ptosis; Type suture continues.
RESUMO
INTRODUÇÃO: A blefaroptose ou ptose palpebral caracteriza-se pelo posicionamento anômalo da pálpebra superior em relação à sua posição normal, que é de 1 a 2 mm abaixo do limbo superior da íris; pode variar, apresentando desde uma queda discreta, até a oclusão total da fenda palpebral. Em geral, trata-se de deficiência muscular ou nervosa, de etiologia congênita ou adquirida, que resulta na impossibilidade de elevação completa da pálpebra superior, podendo também ocorrer por desinserção aponeurótica. Apresenta-se neste trabalho a tática da sutura contínua da aponeurose do músculo levantador ao tarso, ou mesmo na sua plicatura, para o tratamento da ptose leve ou moderada.
MÉTODOS: No período de 2006 a 2012, foram realizadas 26 cirurgias, abordando a aponeurose do músculo levantador com encurtamento na relação 4:1, usando sutura contínua em duplo sentido, finalizando-a com ponto em formato de oito.
RESULTADOS: Em 88,32% dos casos, os resultados foram bons e, em 11,68%, regulares. Apenas um caso evoluiu com retração na pálpebra superior, elevando o sulco palpebral. Observou-se correção incompleta, com ptose residual de 2 a 4 mm em 2 casos, os quais foram submetidos a revisão cirúrgica após 6 meses.
Palavras-chave: Blefaroplastia; Blefaroptose; Ptose congênita; Tipo de sutura contínua.
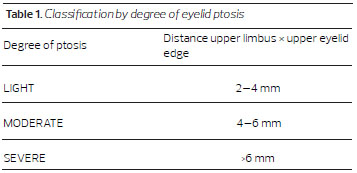
Blepharoptosis or eyelid ptosis, characterized by the anomalous positioning of the eyelid in relation to its normal position of 1-2 mm below the upper limbus of the iris10, can present as slight falling to complete occlusion of the eyelid fold. From the didactic point of view, it is divided into light, moderate, and severe grades according to lifting muscle function. It is generally a muscular or nerve deficiency of congenital or acquired etiology10,11 that can involve detachment of the aponeurosis, resulting in an inability to completely lift the upper eyelid. Ptosis can be uni- or bilateral and can be classified as shown in Tabela 1.
Two types of eyelid ptosis can be distinguished: true and false. True ptosis features irreversible muscular or nerve damage11 or mitochondrial myopathies (external chronic progressive ophthalmolplegia) such as the Kearns-Sayre Syndrome13 (KSS) and Fuchs ocular myophaty20. False ptosis or pseudoptosis occurs due to correctable pathological processes that compromise one or more structures of the eyelid including the skin, muscle, tarsus, or conjunctiva. The leading causes of false ptosis are cutaneous excess, bruising, edema, abscess (of cutaneous origin), myositis (muscular origin), syphilitic or leprous tarsitis (originating in the tarsus), trachoma (originating in the conjunctiva), Syndrome of Duane with fibrosis of the extraocular muscles, enophthalmia, and Graves disease with retraction of the contralateral eyelid16. In cases of microphthalmia, enophthalmia, anophthalmia, enucleation of the ocular globe, and fractures (of the orbital cavity), the eyelid descends irrespective of the integrity of the oculomotor nerve and lifting muscle of the upper eyelid due to lack of support. Finally, we have also encountered "false contrasting ptosis" of the unilateral exophthalmia.
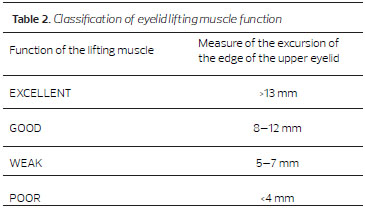
Determination of the function of the lifting muscle of the eyelid is essential in the examination of patients with ptosis because planning of surgical correction of blepharoptosis without this information is not possible. The function of the lifting muscle is classified as excellent, good, weak, or poor (Table 2). The muscle of Müller has only subsidiary action.
Congenital cases may be simple or complex due to other anomalies such as synkinesis, a phenomenon described by Gunn in 1883 that consists of unilateral congenital ptosis that improves with time and certain voluntary movements of the mouth or jaw.
The differentiation between patients with congenital or acquired eyelid ptosis is of great importance because their surgical outcomes can differ13. Thus, determination of the degree of ptosis and the function of the lifting muscle of the eyelid is essential in selecting the optimal correction method1,3,16.
It is of fundamental importance that the ophthalmologist check the eyes for visual acuity, strabismus, visual field, diplopia, amblyopia, ocular motility, Marcus Gunn and Bell phenomenon, and corneal sensitivity, among others. In almost all cases, correction of the ptosis will cause edema and/or lagophthalmos, even if transitory. Research on the Bell phenomenon is very important because, when absent, the corrective surgery must ensure no corneal exposure, which can lead to complications such as keratitis and even corneal ulcers that, in extreme cases, can result in loss of sight in the affected eye16.
In the absence of the lifting muscle, other techniques can be applied, such as use of the upper rectus and corrugator muscles and frontal suspension (use of a silicon strip) of the fascia lata4,6,7. These are the so-called indirect techniques for not acting directly on the lifting muscle.
The objective of this work is to present an alternative to sutures in the correction of light and moderate eyelid ptosis, with continuous suturing for plication and reinsertion of the aponeurosis of the lifting muscle into the tarsus.
METHOD
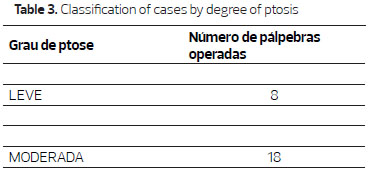
A total of 26 patients (16 male, 10 female) with unilateral light or moderate eyelid ptosis underwent corrective surgery (Table 3) between 2006 and 2012 under general or local anesthesia with sedation. The anesthetic solution consisted of lidocaine with a vasoconstrictor at a concentration of 1:100,000; the patients originated from S.U.S. and from the author's private clinic. The average patient age was 43 years (range, 6-80 years).
After a cutaneous incision was made in the eyelid fold, the orbicular muscle was divulsed and the orbital septum was opened. Immediately below the medium fat mass, the aponeurosis of the lifting muscle was accessed and dissected in the cranial direction up to the Whitnall ligament and caudal to the tarsal plaque.
The aponeurosis portion of the lifting muscle was demarcated in the form of an arch using methylene blue and the lower line had a dimension of 6-8 mm in the central third and 3-4 mm in the lateral and medial thirds. The upper trace corresponded to a line equidistant to the lower trace (Figure 1 ). Shortening of the aponeurosis occurred at the expense of a plication in the proportion of 4 mm of shortening for each millimeter of ptosis moving from the medial to the lateral region (Figure 2). After thread traction was gained, ptosis was corrected and a locking node was made. In the sequence, we used 5-0 monofilament nylon to create a continuous suture in the medial direction that was interlaced with the thread to create suture ends with a figure eight shape. We used 5-0 monofilament nylon for this purpose. We also sutured the edges of the orbicular muscle with 4-5 separate stitches using 6-0 monofilament nylon and closed the skin with an intradermic suture using monofilament nylon 6-0.
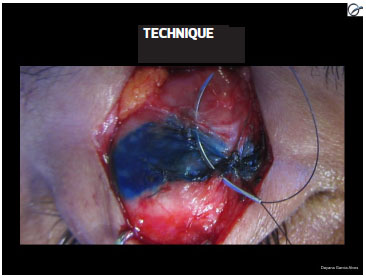
Figura 1. Demarcation of the aponeurosis

Figure 2. Suturing technique
One hour before the start of the surgery, a prophylactic antibiotic consisting of first-generation cephalosporin was administered, and the cornea was protected during all the surgical procedures with methylcellulose ointment and a scleral lens. In the series of treated cases, there was no need to apply the Frost point. Methylcellulose ointment was applied during sleep in addition to swabs with cold physiological saline and an oral analgesic for the first 7 postoperative days. The stitches were removed on the fifth to seventh postoperative day.
RESULTS
Of the 26 patients who underwent surgery, eight had light ptosis, 16 had moderate ptosis, and two had detachment. In cases of aponeurotic shortening, the average shortening was 12mm.
The results were good, regular, or poor according to the achieved esthetic and functional aspects. A good result was identified when the upper eyelid edge was symmetrical with the contralateral side or had a height difference of <0.5mm with the eyes looking forward. A regular result was recorded when the operated side was asymmetrical up to 1 mm in the same position, while a bad result was noted when the operated side had a height difference of >1mm. The average degree of ptosis in the studied cases was 5mm (range, 4-8mm), and the lifting muscle was preserved in all eyes. The patients were followed up for a mean 48 months (range, 1-60 months). We photographed and examined the patients. The results were good in 92.3% of cases and regular in 7.7% of cases. There were no cases with bad results.
Two of the patients had a mean residual ptosis of 1.1 mm. One patient with detachment required surgical review for a residual ptosis of 2mm. Examination of the continuous suture revealed that it was safe and functional. The aponeurosis was shortened further and the previous suture was maintained in the distal portion of the aponeurosis near the tarsal plate. Another patient demonstrated satisfaction with the achieved result and did not undergo surgical review.
All surgeries employed continuous bidirectional sutures for the plication of the aponeurosis of the lifting muscle or its reinsertion into the tarsus.
DISCUSSION
The patients with eyelid ptosis presented with distinct clinical histories and were thoroughly investigated by the surgeon to ensure a precise etiological diagnosis of the deformity. Such details contributed to the correct surgical planning in each case.
It is often interesting to see whether light or moderate ptosis was previously undetected using an old picture of the patient. Dermatochalasis that occurs with age can increase the degree of deformity. This simple observation facilitates the distinction between the acquired and congenital disease forms, and the more the eyelids are touched, the more difficult it will be to identify the anatomical structures due to the formation of fibrous scars.
Patients with acquired ptosis usually report at the start of the disease and present with good lid lifting function. Some cases of acquired ptosis are related to frequent friction of the eyelids, local trauma, or even surgery with associated edema. In these cases, reinsertion of the aponeurosis of the lifting muscle is the surgery of choice and the surgical intervention often has favorable results. In the cases of congenital ptosis, a differential diagnosis is also necessary. Whenever possible, the underlying disease such as hypothyroidism, myasthenia gravis, or Horner syndrome must be treated before surgical correction of the deformity. In the light or moderate forms of ptosis in which the lifting muscle has good or excellent function, the surgical results are usually satisfactory. In contrast, severe ptosis has better results when corrected through indirect methods.
In the congenital form, the function of the lifting muscle and the degree of ptosis will determine the best surgical technique for correction. The accuracy of this procedure has varied in the literature according to surgeon experience. One or more interventions may be necessary to adjust the degree of aponeurotic shortening16,17 or correct an eventual hypercorrection over time.
Aponeurotic plications and lifting muscle reinsertions into the tarsus usually use separate stitches and have reportedly good results in the literature. Because repairing ruptures of tendons and aponeurosis in the human body demands reinforced stitches, we prefer to use continuous stitches that follow the general shape of the eyelid to correct the lifting muscle.
Although the aponeurosis of the lifting muscle is not typically under intense stress, it is frequently pulled during the process of blinking 20 times a minute. Considering that suture threads of higher caliber must be avoided in this thin region to prevent scleral irritation, we prefer to use monofilament nylon 5-0 with a suture that offers reinforcement. As seen with thin caliber sutures, a continuous suture performed in only one direction could cause rupture and loss of function. As such, we used a bidirectional interlaced suture that ended with a figure eight stitch.
CONCLUSION
This correction method achieved good results in cases of light and moderate ptosis with good function of the lifting muscle function, even in cases of detachment. Compared to the use of separate stitches with aponeurotic sutures in conventional techniques, the use of continuous bidirectional sutures is safer and faster due to its easier execution.
In the treatment of light and moderate ptosis, the use of continuous sutures seems to be advantageous over simple stitches because it increases the surface of suture support as well as the number of stitches for anchoring the aponeurosis; additionally, at the end of the plication, only one knot is created.
REFERENCES
1. Beard, C. A. New classification of blepharoptosis. Int Ophthalmol Clin. 1989;29(4):214-6.
2. Beard, C. Advancement in ptosis surgery. Clin Plast Surg. 1978;5(4):537-45.
3. Berke, R.N., Wadsworth, J.A. Histology of levator muscle in congenital and acquired ptosis. AMA Arch Ophthalmol. 1955;53(3):413-28.
4. Blaskovics, L.A new operation for ptosis with shortening of the levator and tarsus. Arch. Ophthalmol. 1923;52:563.
5. Crawford JS. Repair of ptosis using frontalis muscle and fascia lata. Trans Am Acad Ophthalmol Otolaringol. 1956;60(5):672-8.
6. Emsen IM. A new ptosis correction technique: a modification of levator aponeurosis advancement. J Craniofac Surg. 2008;19(3):669-74.
7. Farina, R. Ptose palpebral: contribuição para seu tratamento cirúrgico pelo método de Lexer modificado. (Tese - Livre-Docência). São Paulo, Escola Paulista Medicina; 1962.
8. Friedhofer, H. Correção de blefaroptose severa com implante suspensor palpebral de silicone. (Tese - Livre-Docência). São Paulo, Faculdade de Medicina, Universidade de São Paulo; 2000.
9. Friedhofer H, Nigro MV, Filho AC, Ferreira MC. Correction of blepharophimosis with silicone implant suspensor. Plast Reconstr Surg. 2006;117(5):1428-34.
10. Fox, S.A. Ophthalmic plastic surgery. 5. ed. New York, Grune & Stratton, 1976.
12. Ferreira. L.M. Manual de Cirurgia Plástica. 1°ed. São Paulo: Atheneu, 1995. p.220.
11. Johnson, C.C. Blefaroptosis: a general consideration of surgical methods with the results in 162 operations. Am J Ophthalmol. 1954;38(2):129-62.
12. Jones LT, Quickert MH, Wobig JL. The cure of ptosis by aponeurotic repair. Arch Ophthalmol. 1975;93(8):629-34.
13. Larsson NG, Oldfors A. Mitochondrial myopathies. Acta Physiol Scand. 2001;171(3):385-93.
14. Lessa, S., Carreirão, S. Blefaroptose traumática. Rev. Bras. Cir. 1977;67:31-3.
15. Mccord, C.D., Jr. The evaluation and management of the patiente with ptosis. Clin Plast Surg. 1988 Apr;15(2):169-84.
16. Motais, M. Operation du ptosis par la greffe tarsienne d'une languette du tendon du muscle droit superieur. Ann. Oculist. Ann Oculist. 1897;118:5-12.
17. Mustarde, JC. Repair and Reconstruction in the Orbital Region. 3rd ed. Churchill Livingstone, Edinburgh; 1991.
18. Pitanguy, I.; Lima, J.P. Ptose palpebral. Rev. Bras. Cir.1963;46:265-71.
19. Psillakis, J.M.; Ferreira, M.C.; Spina, V. Ptose palpebral: tratamento cirúrgico pelo encurtamento do músculo elevador da pálpebra. Rev. Col. Bras. Cir. 1971;20:303-7.
Full member, Plastic Surgery by SBCP; Chief of the Plastic Surgery service of Stela Maris Hospital
Institution: Stella Maris Hospital - Guarulhos and DG Clínica (Private Clinic).
Corresponding author:
Dayana Garcia Alves
Rua Vergueiro, 1353 Conj 2001 - Vila Mariana
São Paulo - SP CEP 04101-000
Article received: November 20, 2013
Article accepted: January 6, 2014


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter