

Original Article - Year 2014 - Volume 29 -
Pressure Ulcer Scale for Healing in monitoring of wound healing in elderly patients with leg ulcer
Pressure Ulcer Scale for Healing no acompanhamento da cicatrização em pacientes idosos com úlcera de perna
ABSTRACT
INTRODUCTION: This work describes the evolution of wound healing and outpatient treatment of patients with leg ulcers using the Pressure Ulcer Scale for Healing (PUSH) tool.
METHOD: This research was performed as a case study with four patients. The data were gathered at a State Hospital in the countryside of the State of São Paulo from 2009 to 2010 through digital photographs and the PUSH wound evolution scale. The wound area, amount of exudate and appearance of the wound bed were assessed.
RESULTS: In the first assessment, the first case presented with a total score of 16; the second and third cases, 13; and the fourth case, 15. In the second assessment, the first case presented with a total score of 13; the second, 7; the third, 6; and the fourth, 11. In the last assessment, the first case presented a total score of 4, and the second, third and fourth cases, 0. The application of the PUSH to assess the four patients in this study allowed nurses to perform the optimal wound dressing prescribed for the healing process.
CONCLUSION: It was concluded that the aforementioned tool greatly facilitates nursing performance in assessing and choosing the optimal dressing to promote the epithelialization of the wound, which is based on the assessment of important parameters during the dynamic process of wound care.
Keywords: Venous Ulcer; Wound Healing; Nursing Care.
RESUMO
INTRODUÇÃO: Este trabalho objetiva descrever a evolução da cicatrização e o tratamento realizado em pacientes com úlceras de perna no ambulatório de feridas, utilizando o instrumento Pressure Ulcer Scale for Healing - PUSH.
MÉTODOS: Trata-se de pesquisa na modalidade estudo de caso, realizada com quatro pacientes. Os dados foram colhidos em um Hospital Estadual do interior de São Paulo, nos anos 2009 e 2010, por meio de fotografias digitais e da escala de evolução de feridas Pressure Ulcer Scale for Healing. Os itens avaliados são: área da ferida, quantidade de exsudato e aparência do leito da ferida.
RESULTADOS: Na primeira avaliação, o primeiro caso apresentava escore total 16; o segundo e o terceiro casos, escore total 13; e o quarto caso, escore total 15. Na segunda avaliação, o primeiro caso apresentava escore total 13; o segundo, escore total 7; o terceiro, escore total 6; e o quarto, escore total 11. Na última avaliação, o primeiro caso apresentava escore total 4 e no segundo, terceiro e quarto casos, o escore total foi zero. A aplicação da Escala Pressure Ulcer Scale for Healing na avaliação dos 4 pacientes deste estudo possibilitou aos enfermeiros realizar a prescrição da cobertura ideal para o processo cicatricial da lesão.
CONCLUSÃO: Concluiu-se que o referido instrumento facilita sobremaneira a atuação da enfermagem na avaliação e na escolha da cobertura ideal para a promoção da epitelização da lesão, uma vez que tem por base a avaliação de parâmetros importantes durante o processo dinâmico do cuidar de feridas.
Palavras-chave: Úlcera Venosa; Cicatrização de Feridas; Cuidados de Enfermagem.
Chronic wounds are defined as those that do not spontaneously heal within three months and are often complicated with the presence of an infection. They are also considered complex wounds, especially when associated with systemic diseases that impair the healing process1.
Chronic wounds include leg ulcers, which are very common in medicine and can result in high financial management costs. Leg ulcers are characterized by circumscribed or irregular loss of the dermis or epidermis, which may reach the subcutaneous tissue and underlying tissues2.
It is known that most leg ulcers have vascular causes, mostly venous insufficiency (70% to 90%) and, less frequently, arterial occlusive disease and diabetes (10% to 15%) affecting up to 5% of the adult population in Western countries3,4.
Clinical treatment is based on wound-site dressings and care, which encourage and contribute to healing5,6,7.
In order for the provider to select an optimal dressing for wound healing, the wound must first be assessed so that a therapeutic plan can be developed and the type of dressing appropriate the type of wound and its characteristics can be selected.
A wound assessment involves a description of its characteristics, such as location, size, appearance, the state of the surrounding skin, and its exudate8,9.
Wound assessment may lead to varied diagnoses due to the diversity of the nature, shape and location of the lesions, the personal evaluation of the nurse, and differing degrees of knowledge among health care providers who perform the assessment. The same wound can be assessed and documented differently by different individuals, which may lead to conflicting or disparate diagnoses10,11. The use of scales is necessary in evaluating wound healing evolution parameters and standardize assessment of the tissue type, exudate, wound size and pain12.
Among the wound evolution scales available in the national literature, the Pressure Ulcer Scale for Healing (PUSH) tool is of great importance, as it enables monitoring the wound healing process.
PUSH considers three parameters for the assessment of the wound healing process and the intervention results. The first parameter is the area of the wound (cm2), calculated using the longest length (cephalocaudal) and the longest width (horizontally from right to left). After multiplying the two measures to obtain the area of the wound, values from 0 to > 24 cm2 and scores from 0 to 10 were calculated based on the area obtained.
The second parameter is theamount of exudate present in the wound. This is assessed after removing the dressing and before applying any topical agent. The exudate is classified as absent, small, moderate and large, corresponding to scores ranging from 0 (absent) to 3 (large).
Lastly, the appearance of the wound bed is determined based on the type of tissue prevalent in this region. Necrotic tissue (eschar) is black, brown or maroon in color, adheres firmly to the bed or edges of the wound and may be more hardened or softened compared to the skin. Slough is yellow or white tissue that adheres to the bed of the wound, presents itself as thick strings or crusts, and may be mucinous. Granulation tissue is rosy or red in color, with a shiny, moist and lumpy appearance. Epithelial tissue appears as new rosy or bright tissue that develops from the edges or in the form of "islets" on the lesion surface (superficial wounds). Closed or covered wounds are completely covered with epithelium. These tissues types correspond to scores of 0 (closed wound), 1 (epithelial tissue), 2 (granulation tissue), 3 (slough) and 4 (necrotic tissue).
The sub-scores for these parameters, or sub-scales, render a total score between 0 and 17. Higher scores indicate worse ulcer conditions and decreasing scores indicate improvement in the healing process. Therefore, by measuring only three variables, the PUSH tool generates a score that, through its magnitude and direction of movement, can describe the conditions and development of the ulcers. The tool in question was created to monitor the evolution of pressure ulcers but, in Brazil, has been adapted and validated for the monitoring of leg ulcers13,10.
Thus, the aim of this study were to describe healing evolution using an optimal dressing for 4 leg ulcer cases using the PUSH tool.
METHODS
This is a qualitative case study research conducted with 4 patients with leg ulcers (one patient with a diabetic ulcer, two with venous ulcers and one with a joint ulcer) examined for wounds in an outpatient setting in a hospital in the State of São Paulo.
The inclusion criteria were patients with leg ulcers of vasculogenic origin. Patients with other leg ulcer etiologies were excluded.
Before the beginning of the study, patients received a verbal explanation of the goals and methods of the study and were asked to provide written consent, according to Resolution 196/96 of the National Health Council of Brazil on human research ethics, for the use of photos in the preparation and publication of the article. The project was approved by the Research Ethics Committee of the Universidade Federal de São Paulo (CEP-0793/10). The data were gathered between March 16, 2009 and November 2010.
Data were collected during the following steps: recording with digital photos, wound cleaning, wound assessment and selection of optimal dressing to promote epithelization of the wound.
Photos of the wound were taken using a Sony Cyber-shot DSC P200 digital camera before the study and during the course of wound treatment.
The wound was cleaned with warm 0.9% sodium chloride (NaCl, saline) solution by irrigation with a 20 mL syringe and 40x12 gauge needle. By using saline in a 35 mL syringe and 25x8 gauge needle, a pressure of 13.5 psi is obtained, which reduces bacteria quantitatively and with a greater frequency compared to a 20mL syringe with a 40x 12 gauge needle and mechanical action. When a wound is exposed to the environment, surface temperature decreases. The wound may require up to 40 minutes to return to the initial temperature and up to three hours for mitotic activity to return. For this reason, all dressing must be carried out with warm saline.
After cleaning the wound, an initial assessment of the lesion was performed using the PUSH tool. This assessment was repeated weekly.
The selection of optimal dressing to promote healing and epithelization of the wound was conducted according to the total PUSH score.
RESULTS
Four patients with leg ulcer participated in this study. Two patients (50%) had venous ulcers; 1 (25%), an arterial ulcer; and 1 (25%), a diabetic foot ulcer.
Case 1 (diabetic patient with foot ulcer).
The patient was VPM, a 69-year-old married electrician who had been a diabetic for 10 years. The patient used of 15 units of regular insulin daily. He was referred to the outpatient Wound Prevention and Treatment team by the outpatient clinic in his town. The wound dressing was consisted of fibrinolysin, deoxyribonuclease and chloramphenicol ointment.
On July 15, 2010 (Figure 1), the wound presented with Charcot foot, friable tissue, and slough at the center and edges of the lesion. Additionally, there was a large quantity of exudate. Cleaning was performed using saline and silver Hydrofiber dressing. The wound had a total score of 16 in the PUSH assessment.

Figure 1. Beginning of treatment.
On Aug. 20, 2010 (Figure 2), the wound presented with slough and a moderate amount of exudate. The previous management strategy was maintained. The wound had a total PUSH score of 13.

Figure 2. Treatment, day 35.
On Oct. 14, 2010 (Figure 3), granulation tissue, a small amount of exudate and epithelialization of the edges were noted. Wound management was performed using a dressing made of alginate hydrogel. The wound had a total PUSH score of 8.

Figure 3. Treatment, day 85.
Case 2 (venous ulcer).
The patient was MFTD, a married and retired 66-year-old. The patient had an ankle-brachial index (ABI) of 0.92 and had been living with the ulcer for 5 months.
On Sept. 10, 2010 (Figure 4), the lesion presented with slough and a moderate amount of exudate. Cleaning was performed with saline and Silver Hydrofiber dressing. Compression therapy was used (Unna boot). The wound had a total PUSH score of 13.

Figure 4. Treatment, day 1.
On Sept. 31, 2010 (9/31/2010) (Figure 5), the wound had a small amount of exudate and granulation tissue. The previous management strategy was maintained. The wound had a total PUSH score of 7.

Figure 5. Treatment, day 21.
On Oct. 29, 2010 (Figure 6), the lesion had completely epithelialized. The wound reached a total score of 0 in the PUSH assessment.

Figure 6. Treatment, day 51.
Case 3 (Arterial Ulcer).
The patient was TST, a retired 75-year-old female with hypertension and chronic kidney disease. The patient had an ABI of 0.5. The sudden onset of the ulcer occurred after trauma when alighting from a bus for hemodialysis.
On Dec. 12, 2008 (Figure 7), the ulcer presented with slough throughout the lesion area and a small amount of exudate. Cleaning was performed with saline. The wound was covered with a thin layer of alginate hydrogel and nanocrystalline silver dressing. The wound had a total PUSH score of 12.

Figure 7. Treatment, day 1.
On Jan. 22, 2009 (Figure 8), it was observed that the lesion had granulation tissue in the center, epithelialization around the edges, and an absence of exudate. For the dressing, alginate hydrogel was used. The wound had a total PUSH score of 6.

Figure 8. Treatment, day 41.
On 2/26/09 day (Figure 9), epithelialization was verified in the lesion and a total PUSH score of 0 was achieved.

Figure 9. Treatment, day 67.
Case 4 (venous ulcer).
The patient was NSLM, a 70-year-old female with a personal history of hemolytic anemia, heart disease, osteoporosis, arthritis and arthrosis, and a thyroid cyst. There was a sudden onset of the wound in the lower limb with an ABI of 1. The wound was treated using nanocrystalline silver dressing with an Unna boot and was changed weekly.
On June 29, 2009 (Figure 10), the wound was covered by sloughs with moderate exudate. The ABI was calculated and nanocrystalline silver dressings with an Unna boot were applied. The wound had a total PUSH score of 13.On Aug. 3, 2009 (Figure 11), the lesion had granulation tissue with a small amount of exudate. The wound had a total PUSH score of 1. The same management strategy was maintained.
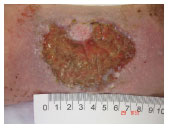
Figure 10. Beginning of treatment.

Figure 11. Treatment, day 34.
On Dec. 7, 2009 (Figure 12), the wound had epithelialized, showing a small portion of granulation tissue around the edges and center, and an absence of exudate. The wound had a total PUSH score of 4. For the dressing, alginate hydrogel was used.
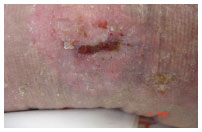
Figure 12. Treatment, day 180.
In Table 1, it was observed that all cases had a high total score during the initial assessment, with the presence of devitalized tissue and exudate verified in the wounds. There was a decrease in the total scores in all cases at the second assessment, along with a verified improvement of the lesions. In the third assessment, there was an improvement of the wounds cases 1 and 4, with the presence of granulation tissue and a decrease in the lesion size. In cases 2 and 3, a total score of zero was reached. By the fourth assessment, cases 1 and 4 also obtained a total score of zero, demonstrating that the ulcers were epithelialized.
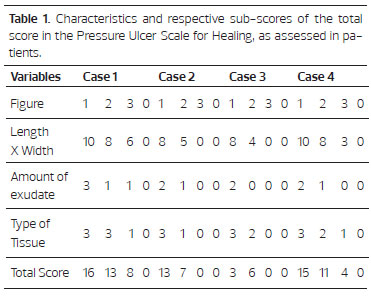
All cases had a high total score in the initial assessment and a low score in the last assessment. The score allowed the researcher to prescribe the optimal dressing at each stage of healing.
In Figure 13, the trends of the wound assessment results through the scores of the Pressure Ulcer Scale for Healing tool are shown. All cases had a high total score in the initial assessment and a low score in the last assessment. The score allowed the researcher to prescribe the optimal dressing at each stage of healing.
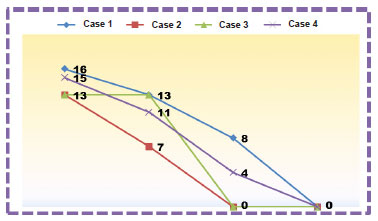
Figure 13. Evolution of the wounds , according of the total score of the Pressure Ulcer Scale for Healing
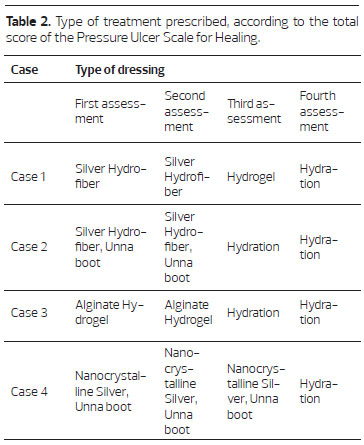
Table 2 describes the dressings used for the treatment of the 4 cases. These choices were made by applying the PUSH tool, enabled prescription of the optimal dressing at each stage and promoting moist conditions and lesion healing.
DISCUSSION
Patient with wounds should be treated by a multidisciplinary team, in which the nurse plays an integral role. During wound assessment, nurses must make decisions based on knowledge of skin anatomy, principles of tissue repair physiology, and influencing factors. These professionals require knowledge of the types of ulcers and various existing forms of treatment to be able to develop an ability to observe tissue loss, the clinical aspect of the lesion, its location and size, the presence of exudate, as well as characteristics of the surrounding skin, pain and signs of infection12,14.
Nursing professionals should objectively assess the wounds to evaluate their evolution on a regular basis, starting with an initial analysis8.
In caring for patients with lesions, the assessment and evolution of the wound should be reported with discretion, based on tools that facilitate documentation of the wounds' characteristics and factors that could slow the epithelialization process.
The use of assessment and wound evolution tools favors the systematic recording of the treatment, facilitates continuity of assistance, and promotes the quality of the therapeutic intervention. The systematic care of patients with lesions minimizes healing time and allows for a cost/benefit analysis of treatment being used8.
In this study, the lesions were assessed using the PUSH tool, which allowed monitoring of the evolution of the wound healing process. The use of this tool contributed to the selection of the optimal dressing for each stage of healing.
Several authors have used the PUSH tool in patients with chronic wounds and concluded that this easily applicable tool contributed to monitoring and documentation of the wound healing progress15-18.
Some authors have used this tool to monitor wound healing process in patients with chronic wounds. They have been able to document the cicatricial evolution of the lesion and select the optimal dressing for this process12,19.
In a study of 27 patients with venous ulcers in which wound healing was monitored using the PUSH Scale, the authors concluded that the PUSH tool is effective in monitoring the wound healing process1.
Another study using a convenience sample of 18 individuals examined the predictive validity of the PUSH Scale in monitoring the healing of diabetic ulcers. The study demonstrated that the lesions healed completely in 13 weeks and that the PUSH tool is an agile assessment tool to monitor and document the progress of wounds20.
The healing process requires the topical treatment of the lesion, dressing, and cleaning. Currently, there is evidence that occlusion of a lesion creates a physical barrier between the wounded bed and the external environment. This maintains some of the factors that are ideal for quick healing, such as moisture and temperature. Prevention of infection must also be considered in the selection of the dressing for wound treatment21-23.
In this study, all lesions were cleaned with saline. The dressing used was chosen in accordance with the total PUSH score. During the initial assessment (7/16/2011) of Case 1, silver Hydrofiber was used. At the second (8/20/2010) assessment, the previous management strategy was maintained. On Oct. 15, 2010, alginate hydrogel was applied. At the initial assessment of Case 2 on Sept. 10, 2010, silver Hydrofiber and compression therapy with an Unna boot were applied. At the second assessment, the same management strategy was maintained. By the third assessment on Oct. 29, 2010, the lesion had healed and the patient was treated with skin hydration and compression therapy with stockings.
Silver Hydrofiber is an antimicrobial dressing composed of sodium carboxymethylcellulose and 1.2% ionic silver. It is absorbent and capable of capturing microorganisms present in the wound bed. Upon contact with the exudate, it becomes a cohesive gel that adapts to the wound bed. Silver Hydrofiber keeps the environment moist and controls bacteria, thus contributing to the healing process and reducing the risk of wound infection24.
Various studies25,26 conducted with chronic and acute wound patients demonstrated that silver Hydrofiber acts by reducing the exudate and as a chemical debrider by liquefying the entire necrotic and devitalized tissue. It also has bactericidal action, stimulates the development of granulation tissue and promotes healing.
Hydrogel is indicated for dry wounds or those with little exudate and necrotic granulation tissue, as it assists in removing crusts. It can also be used to clean superficial wounds, such as lacerations, cuts, abrasions, graft removal and insertion areas, diabetic ulcers and pressure ulcers, lower limb ulcers (arterial, venous and mixed), and in first and second degree burns. It acts by promoting leukocyte chemotaxis, angiogenesis, and autolytic debridement, and keeps moisture at optimal levels for the healing process27,26.
In Case 3, treatment throughout the cicatricial process required the use of alginate hydrogel. In Case 4, starting on 6/29/2009 and continuing throughout the lesion treatment, nanocrystalline silver dressing and compression therapy were used.
Compression therapy (inelastic and elastic systems) is a very useful resource for patients with venous ulcers caused by problems of the lower limb veins27-29.
The inelastic system supports muscular pumping of the calf region while walking and assists in the venous return. It is indicated for patients who are able to walk, thus increasing venous pumping efficiency. For this system, the Unna boot, which can be manipulated or purchased ready for use, was developed28,30.
The Unna boot adapts to the shape of the legs, is flexible and has a relatively low cost. It can also be prepared at hospitals or compounding pharmacies. It can be maintained for a period of up to seven days, provided signs of infection are kept under control31-33.
The bandages of the elastic system provide continuous limb compression. They are classified as a compression bandage system (elastic bandages) and a multi-layer compression bandage system.
The compression bandage system (elastic bandage) consists of elastic fibers and provides a compression that is maintained over a given period of time. This means that compression is exerted during exercise and rest34,35.
Elastic bandages have greater stretch and render high pressure, both during muscular contraction and rest36-38.
Technical-scientific developments require enhancement through professionals to ensure the quality of patient care. Commonly, wounds are usually cared for unsystematically by different professionals. Bandage changing is not often specified and a systematic wound assessment is not performed, thus hindering its evolutionary analysis8,23,39.
Therefore, the nurse assisting the patient with a wound should recognize the importance of using a tool for the assessment of the wound healing stages. This allows such professionals to perform a facilitative intervention of the healing process by selection of the topical therapy or dressing for an optimal environment for wound healing. Finally, a better quality of life for the patient can be achieved by prevention of infection and ensuring patient satisfaction.
CONCLUSION
The PUSH tool enabled the author to monitor the wound healing process by assessing the wound area, the amount of exudate present, and the type of tissue in the lesions, thus enabling the selection of an optimal dressing for each stage of healing.
REFERENCES
1. Ferreira MC, Tuma Júnior P, Carvalho VF, Kamamoto F. Wounds complex. Clinics. 2006;61(6):571-8.
2. Oliveira SH, Soares MJ, Rocha PS. Uso de cobertura com colágeno e aloe vera no tratamento de ferida isquêmica: estudo de caso. Rev. Esc. enferm. USP. 2010;44(2):346-51.
3. Abbade LP Lastória S. Abordagem de pacientes com úlcera da perna de etiologia venosa. Anais Bras Dermatol 2006;81(6):509-22.
4. Salomé GM, Blanes L, Ferreira LM. Capacidade funcional dos pacientes com diabetes mellitus e pé ulcerado. Rev Acta Paul Enferm. 2009;22(4):412-16.
5. Stacey M, Falanga V, Marston W, Moffatt C, Phillips T, Sibbald RG et al. Use of compression therapy in the treatment of venous leg ulcers - via recommended treatment. Euro Wound Manag Assoc J. 2002;2(1):340-5.
6. Trent JT, Falabella A, Eaglstein WH, Kirsner RS. Venous ulcers: pathophysiology and treatment options. Ostomy Wound Manage. 2005;51(5):38-54.
7. Palfreyman S, King B, Walsh B. A review of the treatment for venous leg ulcers. Br J Nurs. 2007;16(15):6-14.
8. Bajay HM, Pedrosa MM Lourenço MT Cortez SL, Paula M. Registro de avaliação e evolução de feridas: subsídios para reflexão e mudanças. Rev Estima. 2003;1(2):20-9.
9. Hon J, Lagden K, McLaren AM, O'Sullivan D, Orr L, Houghton PE, Woodbury MG.prospective, multicenter study to validate use of the PUSH in patients with diabetic, venous, and pressure ulcers. Ostomy Wound Manage.2010;56(2):26-36.
10. Santos VL, Sellmer D, Massulo M M. Confiabilidade interobservadores do Pressure Ulcer Scale for Healing (PUSH), em pacientes com úlceras crônicas de perna. Rev. Latino-Am. Enfermagem. 2007;15(3):391-6.
11. George-Saintilus E, Tommasulo B, Cal CE, Hussain R, Mathew N, Dlugacz Y, Pekmezaris R, Wolf-Klein G. Pressure ulcer PUSH score and traditional nursing assessment in nursing home residents: do they correlate? J Am Med Dir Assoc. 2009;10(2):141-4.
12. Salomé GM, Araujo VS. Uso do Pressure Ulcer Scale for Healing (PUSH) no acompanhamento da cicatrização em paciente diabético com úlcera no pé. Rev Nursing. 2010;14(149):507-11.
13. Santos VLCG et al. Adaptação transcultural do pressure ulcer scale for healing (PUSH) para a língua portuguesa. Rev. Latino-Am. Enfermagem. 2005;13(3):305-13.
14. Castro ME, Silveira JM. Feridas: um desafio para enfermagem. Rev USP. 1999;33(número especial):167-72.
15. Günes UY. A prospective study evaluating the Pressure Ulcer Scale for Healing (PUSH Tool) to assess stage II, stage III, and stage IV pressure ulcers. Ostomy Wound Manage.2009 55(5):48-52.
16. Ratliff CR, Rodeheaver GT. Use of the PUSH tool to measure venous ulcer healing. Ostomy Wound Manage.2005;51(5):58-60.
17. Sung, Young Hee; Park, Kyung Hee. Factors Affecting the Healing of Pressure Ulcers in a Korean Acute Care Hospital. .Journal of Wound, Ostomy & Continence Nursing. 2011;38(1):38-45.
18. Gardner SE, Frantz RA, Bergquist S, Shin CD. A prospective study of the pressure ulcer scale for healing (PUSH). J Gerontol A Biol Sci Med Sci.2005;60(1):93-7.
19. Barros A, Oliveira JD. Uso do pressure ulcer scale for healing no acompanhamento da cicatrização de úlcera por pressão. Rev Estima. 2006;4(4):135.
20. Gardner, Sue, E Hillis, Stephen L, Frantz, Rita A. A Prospective Study of the PUSH Tool in Diabetic Foot Ulcers. J Wound Ostomy Continence Nurs. 2011 Jul-Aug;38(4):385-93.
21. Leaper DJ. Silver dressings: their role in wound management. Int Wound J. 2006;3(3):282-94.
22. Salomé GM. Avaliando lesão: prática e conhecimentos dos enfermeiros que prestam assistência ao indivíduo com ferida. Rev Saúde coletiva. 2009;6(35):280-87.
23. Beam JW, Topical silver for infected wounds. J Athl Train. 2009 Sep-Oct;44(5):531-3.
24. Salomé GM, Araújo E. Uso do Pressure ulcer for Healing (PUSH) no acompanhamento da cicatrização em paciente diabético com úlcera no pé. Rev Enfermagem Prática. 2010;14(149):507-11.
25. Salomé GM. Aplicabilidade da Hidrofibra com prata em lesão provocada pela Síndrome da Founier: relato de experiência. Nursing. 2008:11(127):566-70.
26. Mandelbaum SH, Di Santis, Mandelbaum ÉP, Sant'Ana MH. Cicatrização: conceitos atuais e recursos auxiliares - Parte II. An. Bras. Dermatol. 2003;78(5):521-22.
27. Kirsner R. Tissue engineering shows promise in areas other than skin repair. In: Meeting da AAD; 2003 Mar, Miami, USA.
28. Pina E, Furtado K, Albino AP. Boas práticas no tratamento e prevenção das úlceras de perna de origem venosa. GAIF, 2007.
29. Baptista CM. Bota de Unna Rev Estima. 2004;2(2):39-40.
30. Bolton L.Compression in Venous Ulcer Management. J Wound Ostomy Continence Nurs. 2008 Jan-Feb;35(1):40-9.
31. Lorimer KR, Harrison MB. Graham ID, Friedberg ERN, Davies BRN. Venous Leg Ulcer Care: How Evidence-Based Is Nursing Practice? J Wound Ostomy Continence Nurs. 2003;30(3):132-42.
32. Davis J, Gray M.Is the Unna's Boot Bandage as Effective as a Four-Layer Wrap for Managing Venous Leg Ulcers? J Wound Ostomy Continence Nurs. 2005;32(3):152-6.
33. Moffatt CJ, Franks PJ. Epidemiology and Health Services Research. Implementation of a leg ulcer strategy. Br J Dermatol. 2004;151(4):857-67.
34. Bergan JJ. FA, FR, Sparks, Steven R. Non-elastic Compression: An Alternative in Management of Chronic Venous Insufficiency. J Wound Ostomy Continence Nurs. 2000;27(2):83-9.
35. Carmel JE. Compression therapy options for management of venous insufficiency ulcers. J Wound Ostomy Continence Nurs. 2009 May-Jun;36(3):299-305.
36. Salomé GM. Relato de caso: tratamento de úlcera venosa com hidrocoloide e Terapia compressiva. Rev Estima. 2008;6(2):37-9.
37. Espirito S, Patrícia F, et al. Use of the Pressure Ulcer Scale for Healing tool to evaluate the healing of chronic leg ulcers. Rev. Bras. Cir. Plást.2013;28(1):133-41.
38. Lima EL, Salomé G M, Rocha M J ABo, Ferreira L M.The impacto f compression therapy with unna boot on the functional status of VLU. J Wound Care. 2013;22(10):558-61.
39. Salome GM, Ferreira LM.Quality of life in patients with venous ulcers treated with Unna's boot compressive therapy. Rev. Bras. Cir. Plást. 2012;27(3):466-71.
1- Master's Student in Nursing at the Universidade de Guarulhos, Guarulhos, São Paulo
2- Applied Sciences to Health Master's Student at the Universidade do Vale do Sapucaí-UNIVÁS. Pouso Alegre, MG, Brazil
3- Doctor, Professor of the Professional Applied Sciences to Health Master's Degree Program at the Universidade do Vale do Sapucaí-UNIVÁS. Pouso Alegre, MG, Brazil
Institution: Universidade do Vale do Sapucaí.
Corresponding author:
Geraldo Magela Salome
Universidade do Vale do Sapucaí
Av. Pref. Tuany Toledo, 470
CEP 37550-000, Pouso Alegre, MG
E-mail: estomateropeuta@outlook.com
Article received: October 6,2013
Article accepted: December 8, 2013


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter