

Ideas and Innovation - Year 2014 - Volume 29 -
Elastic suture: An alternative for extensive skin loss
Sutura elástica - uma alternativa para grandes perdas cutâneas
ABSTRACT
The treatment of complex wounds in soft tissues remains a major challenge for plastic surgeons. Several reconstruction methods have been used for this purpose, including the use of grafts, flaps, and spreaders. This study aimed to improve the technique of elastic suture by using the biomechanical properties of the skin and in which the open wound areas are closed without the need for detachment and often under local anesthesia, in two surgical stages, and without causing further sequelae. The contribution to the improvement of the technique is based on the use of a polypropylene mesh (Marlex) fixed to wound edges, allowing the elastic traction to be homogeneously distributed throughout the tissue, thus avoiding ischemic necrosis of the wound edges.
Keywords: Suture; Elastic; Scar; Synthesis; Correction; Cutaneous.
RESUMO
O tratamento das feridas complexas das partes moles é um desafio para a cirurgia plástica. Para isso diversos métodos de reconstrução têm sido utilizados como: enxertos, retalhos e expansores. Este trabalho vem aprimorar a técnica de sutura elástica ao utilizar as propriedades biomecânicas da pele, onde as áreas cruentas são fechadas sem a necessidade de descolamentos, muitas vezes, sob anestesia local, em dois tempos cirúrgicos, e sem novas sequelas. A contribuição para o aprimoramento da técnica baseia-se no uso da tela de polipropileno (Marlex), fixada nas bordas da ferida para que a tração elástica seja redistribuída de maneira homogenia, por todo o tecido, evitando a necrose isquêmica das bordas do ferimento.
Palavras-chave: Sutura; Elastica; Cicatriz; Sintese; Correção; Cutânea.
The treatment of complex wounds in soft tissues remains a major challenge for plastic surgeons. In this context, skin detachments, slow expansion, and presuture and elastic suture methods use the basic principles of skin biomechanics to correct various skin defects that are the result of various causes such as car accidents, tissue necrosis, resection of skin lesions, and scar formation, which would otherwise require grafts, flaps, or spreaders.
The elastic suture technique, as an alternative treatment of acute skin loss is a low-cost and easy procedure that provides satisfactory results in the most complicated cases of tissue loss.
Selecting the best technique is essential for the success of the reconstruction, and the fundamentals of reconstructive surgery were created under the assumption that the simplest repair is always the best1. Therefore, primary wound closure is the first choice of treatment whenever possible. Elastic suture was introduced as an alternative therapeutic tool to grafts, flaps, and spreaders.
The anatomical and histological structures of the skin have viscoelastic properties that allow for gradual extension when subjected to continuous traction. This phenomenon is called the "creep phenomenon"2.
In the technique proposed by Raskin3 in 1993 that aimed to perform fasciotomy without tissue loss, an interwoven elastic band is directly fixed to the skin of the wound edges to produce tension, which applies the concept of skin elasticity.
In 1996, Leite3 observed the incidence of skin necrosis in wound edges when the Raskin technique was used and proposed the fixation of the elastic band subcutaneously and to the superficial fascia to avoid tensile force-induced skin ischemia.
Therefore, the technique established in this study uses the total coverage of wound edges with a polypropylene mesh fixed to the skin and to the superficial fascia with several mononylon 2.0 anchoring stitches. This new technique maintains the basic principles of elastic suture associated with the distribution of the traction forces of the skin on the polypropylene mesh to avoid tissue ischemia in wound edges and to further improve the final result.
METHODS
Over 16 years of practice (from September 1996 to November 2012), 78 procedures of complex wound closure were performed by using the described technique of elastic suture. The 78 patients had skin wounds that exhibited tissue loss and did not allow primary closure. The following body areas were treated: scalp, upper limbs, lower limbs, and trunk. The patients' ages ranged from 6 to 52 years, and most (87%) of the patients were male.
Prior to conduction of this study, the patients were informed about the proposed treatment and the need for photographic documentation, and informed consent was obtained.
The technique was performed in two basic surgical stages, interspaced by ambulatory procedures. The first surgical stage was performed under local anesthesia and antibiotic prophylaxis (2g of cefazolin IV) after antiseptic preparation. The wound edges were undermined, and a piece of polypropylene mesh (Marlex), adapted to the thickness of the edges, was fixed to the skin with mononylon 2.0 thread by using the continuous suture technique, and then subcutaneously and to the superficial fascia by using simple interrupted mononylon 3.0 stitches. The procedure was then repeated on the other edge of the wound (Figure 1).
Figure 1. Coverage of the wound edges with the polypropylene mesh, appropriately fixed by using mononylon 2.0 thread.
The next step was to fix a sterile elastic band to the mesh at the apex of the wound by using the sterile elastic of the surgical gloves and interweaving it along the wound with lateral fixation to the mesh. The elastic thread was not tied to the mononylon 2.0 thread, as it should slide through the stitch. The elastic band was pulled and attached to the other edge after each lateral fixation, and the procedure was repeated with the other side of the elastic band, which resulted in the interweaving (Figure 2).
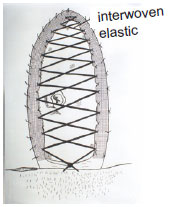
Figure 2. Interwoven elastic band under tension, with lateral fixation to the polypropylene mesh. The elastic band should run through the lateral fixation stitches, like a pulley.
At the end of the procedure was an approximation of the edges, which increased with time and made the elastic band lose its traction. Therefore, a device was coupled to the end of the interwoven elastic band that worked as a tourniquet by rotating around its own axis (by using the cap of a 40- 12-mm needle) to recreate the original traction of the elastic band.
This procedure should be performed until the approximation of the edges is complete so that in a second surgical stage, the mesh can be removed, and the primary suture of the wound is performed with a satisfactory aesthetic result.
RESULTS
Over 16 years of experience with using the described technique, all the 78 cases with indication for elastic suture resulted in the expected approximation of the wound edges, thus allowing primary closure.
The duration of the treatment varies according to the distance between the edges and the technical rigor of both the main suture procedure and the tensile strength of the elastic band, every 3 days. On average, 14 days are required for wound closure.
The most common complication was scar widening; however, it did not cause pain to the patients. No wound infections were observed during the treatments, and an antibiotic prophylaxis was performed by using first-generation cephalosporins only in the primary surgical procedure. Moreover, the various body areas exhibited distinct speeds of wound edge approximation.
CLINICAL CASES
Case 1
Obs: First case of elastic suture in which the Raskin technique was used; the main complication of this technique (ischemic necrosis of the wound edges) can be observed.
A 26-year-old patient had an infected hematoma in the left forearm that progressed to compartment syndrome. Drainage and local fasciotomy were performed; and at a later stage, a large open wound area was formed in the inside of the forearm that did not allow primary closure. The therapeutic option was to perform elastic suture followed by primary closure, and functional and aesthetic recovery of the limb (Figures 3-5).

Figure 3. Tissue loss in the forearm

Figure 4. Elastic suture in the forearm

Figure 5. Final result of the primary closure of elastic suture
Case 2
A 46-year-old patient had undergone a left mastectomy (Halsted technique) and breast reconstruction with a rectus abdominis myocutaneous flap. The patient developed necrosis in the anterior wall of the abdomen (Figure 6), which resulted in a large open wound area of 10 20cm after local undermining (Figure 7). The wound was subjected to elastic suture by using the proposed technique (Figure 1). Because of the thickness of the abdominal wall, two elastics were fixed to the mesh, one posteriorly (Figure 2) and the other anteriorly (Figure 8). Figure 6 shows the results obtained 12 days after the elastic suture, when the elastic bands and mesh are removed, and the primary and definitive suture is performed. Figure 7 shows the final result after primary closure.

Figure 6. Appearance of the abdominal necrotic wound.

Figure 7. Undermined necrotic tissue with lateral fixation of the polypropylene mesh.
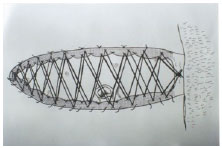
Figure 8. A new layer of intertwined elastic bands over the first layer because of the thickness of the wound edges.
Case 3
A 32-year-old patient who was in a car accident and lost part of the scalp in the frontoparietal region was treated with elastic suture by using the described technique (Figures 9-11).

Figure 9. Scalp wound with tissue loss.

Figure 10. Seven days after the elastic suture.

Figure 11. Final result. alopecia improved in the late postoperative period.
Case 4
A 58-year-old patient who had been run over 40 days previously presented a compound fracture in the distal third of the tibia, which resulted in an area of bone exposure of 9 3cm (Figure 12). Elastic suture using the described technique (Figures 13 and 14) was indicated. The size of the wound was initially 3.0cm in its most wide portion and was reduced to 0.3cm 7 days after elastic suture (Figure 15). On this occasion, the elastic suture and the mesh were removed, and the wound was closed with mononylon 2.0 interrupted stitches (Figure 16).

Figure 12. Wound in the distal third of the leg at 40 days after the procedure.

Figure 13. After undermining and placement of the mesh on the edges of the wound.

Figure 14. After elastic suture.

Figure 15. Elastic suture appearance 7 days after the procedure.

Figure 16. Final appearance of the scar.
Therefore, in this series of 78 patients and 16 years of experience, the results obtained by using the elastic suture technique were satisfactory and effective in the treatment of extensive skin wounds that would otherwise require reconstruction with grafts or flaps, which sometimes result in aesthetic and functional problems. The scars were usually wide; however, this aesthetic problem was expected. Furthermore, the functional and aesthetic results on the scalp were good, and the elongation did not cause permanent alopecia.
DISCUSSION
The use of the biomechanical principle of tissue tension, that is, the increase in metabolic activity that induces vessel growth and collagen fiber proliferation, allows the skin to extend beyond the normal limits of expansibility.
The good results obtained in this study show that extensive skin defects can be corrected without major detachments. The comparison of the initial cases in which the Raskin technique was used and those in which the proposed technique was used showed that the inclusion of the polypropylene mesh allowed a better distribution of the forces on the wound edges, thus avoiding tissue necrosis and providing satisfactory aesthetic and functional results.
CONCLUSION
The elastic suture technique proved to be highly effective, better than grafts and flaps, in the treatment of extensive skin defects because it is easy to execute, does not result in new scars, and only requires local anesthesia in the first and last surgical stages. It can be used on ulcer sites that are difficult to treat, such as the distal third of the leg (as in case 4).
REFERENCES
1. Mathes SJ, Nahai F. Reconstructive Surgery. Principles, Anatomy Techinique. Churchil Livingstone and Qualit Medical Publishing Inc., 1997.
2. Briggs SE, Banis JR, Kaebnick H. Distal Revascularization and Microvascular Free Tissue Tranfer. J. Vasc Surg. 1985; 2:806-11.
3. Raskin. KB. Acute vascular injuries of de upper extremity, in Shaw Wilgis, EF. (ed): Vascular disordes. Hand clin. 1993;9:115-130;
4. Reis, FB. Tratamento de ferimentos deixados abertos com o método da sutura elástica. Rev Bras Ortop. 1996;31(8))687-9.
5. Vidal, MA, Sutura elástica. Atualização em cirurgia plástica SBCP. 2006;124:965- 970.
1 - Full Member of the SBCP, Head of the Plastic Surgery Department of the Faculty of Medicine of Catanduva
2 - Full Member of the SBCP, Professor at the Plastic Surgery Department of the Faculty of Medicine of Catanduva
3 - Member of the SBCP, Professor at the Plastic Surgery Department of the Faculty of Medicine of Catanduva
Institution: Plastic Surgery Department of the Faculty of Medicine of Catanduva - SP.
Corresponding author:
Manoel Alves Vidal
Avenida Orlando Zancaner, 497 - Vila Amendola
Catanduva/SP
E-mail: manoel.a.vidal@gmail.com
Article received: January 14,2013
Article accepted: March 3, 2013


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter