

Case Report - Year 2014 - Volume 29 -
Sequelae of inferior lip silicone injection: surgical correction using the modified "bikini" technique
Sequela de injeção de silicone em lábio inferior: correção cirúrgica pela técnica do biquíni modificada
ABSTRACT
Increasing numbers of patients have sequelae due to the injection of non-absorbable substances. Injectable silicone or polydimethylsiloxane fluid is a manufactured polymer containing elemental silicon. The complications associated with the use of this substance can present early or late. Here we present a case report in which a deformity due to a silicone injection in the lips was surgically treated using the modified "bikini" technique that produced a functionally and aesthetically favorable result.
Keywords: Lips; Lip Reduction; Silicone; Siliconoma; Filler Complications.
RESUMO
Pacientes portadores de sequelas devido a injeções de substâncias inabsorvíveis tem se tornado cada vez mais frequentes. O silicone injetável ou polidimetilsiloxano fluido é um polímero manufaturado que contém silicone elementar. As complicações consequentes ao uso desta substância podem ser precoces ou tardias. Apresentamos um relato de caso onde uma deformidade por injeção de silicone em lábios foi tratada cirurgicamente usando a técnica do biquíni modificada obtendo um bom resultado funcional e estético.
Palavras-chave: Lábios; Redução de Lábios; Silicone; Siliconoma; Complicações de Preenchimentos.
Increasing numbers of patients experience sequelae due to the injection of substances aiming at cosmetic improvement of the body. An individual's desire for a body that resembles a model's and professionals who lack the technical training to perform enhancement procedures are responsible for these increased numbers.
The lips are important structures for the aesthetic harmony of the face and common targets for augmentation. Lips that have just the right amount of fullness can be interpreted as synonymous with health and beauty, which makes a person more attractive. Various substances may be injected for this purpose: fat, collagen, and hyaluronic acid, which are absorbable; and silicone1,2, methacrylate, and polyacrylamide, which are non-absorbable.
Injectable silicone or polydimethylsiloxane fluid is a manufactured polymer containing elemental silicon. The complications associated with the use of this substance occur early or late. Early complications include hypersensitivity reactions, dyschromia, skin texture changes, ecchymosis, and edema. Late adverse effects include overcorrection of the treated area, granulomatous inflammatory reactions ("siliconomas"), idiosyncratic reactions, and migration. This last effect occurs when a large volume of liquid silicone is injected at once in a single location3-6.
The management of lip augmentation sequelae can be expectant, pharmaceutical, or surgical.
CASE REPORT
A 43-year-old male public servant and teacher visited the clinic of the 38th Ward of Santa Casa de Misericórdia with a history of having undergone silicone injections in his lower lip, cheeks, chin, and malar region 3 years previously. His chief complaint was the appearance of his lower lip, which he said created difficulty speaking and retained liquids within his mouth. Physical examination revealed that his lower lip was disproportionately augmented compared to the rest of the face.
The patient was treated with surgical reduction of the lower lip. We used a variation of the bikini technique,7 in which we used curved lines rather than straight lines for the resection.
The bikini technique (Figure 1) comprises reducing the lip through resection of the excess tissue in the area of the vermilion. The junction between the mucosa and the vermilion in the upper and lower lip is marked as the midline (points a to a'). Using the fingertip, the surgeon manipulates the patient's lips to create internal rotation and simulate the reduction to obtain a suitable size. This new point (points b and b'), with the point of the junction of the mucosa with the vermilion, will determine the resection limits. The lateral limit of resection is a point a few millimeters from the labial commissure. The bikini layout is then drawn. In the bikini top (upper lip) is 1cm from the initial marking (ab), while the two other points are marked (cd) at a higher opening (also determined by the finger test). The length of cd should not exceed two times that of ab. These lines are joined to make a rounded contour similar to a strapless bra. At the bottom of the bikini (lower lip), the triangle is defined based on the distance between the corners (points f and e) and point b'7.
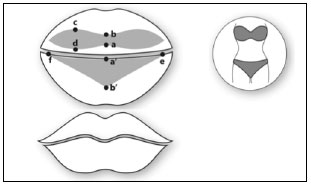
Figure 1. The points marked for use in the bikini technique (middle). The expected result is lip reduction and maintenance of the natural contour thereof (N Fanous, Brousseau VJ, Yoskovitch A. The "Bikini" Lip Reduction: An Approach to Oversized Lips. Plast. Reconstr. Surg. 122: 23e-25e, 2008)7.
The procedure was performed under local anesthesia in a solution of epinephrine at a dilution of 1:200,000 (Figure 2A). The resection was done in a wedge without worrying about identifying the silicone fragments amid the tissue. There was no identification of silicon grouping or major bleeding (Figure 2B). Closure was performed internally in multiple points using vicryl 5-0 sutures and externally using continuous chromic catgut 3-0 sutures (Figure 2C). The patient developed wound dehiscence on postoperative day 7 (Figure 3A) that was treated conservatively with hydrogen peroxide, topical corticosteroids, hydration, and local hygiene until it was resolved on postoperative day 50 (Figure 3B). Both the surgical team and the patient rated the result as very favorable (Figures 4A-4F). In addition to an improved appearance of the lower lip, the patient also reported improved speech and regaining the ability to contain liquid food within his mouth.

Figure 2 A. Bikini markings on the lower lip (curved lines). B. Resection of the excess lip in a wedge. C Postoperative appearance.
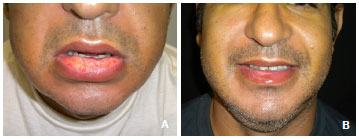
Figure 3 (A e B). Dehiscence seen on postoperative day 7. Appearance of the lip on postoperative day 50.

Figure 4 (A- F). In A, B and C , preoperative representation. In , D , E and F , postoperative results of 65 days.
DISCUSSION
The surgical correction of the sequelae of lips previously filled with non-absorbable substances is often a challenging procedure. The surgeon must ensure that the patient fully understands the limitations of the results in some specific cases, and common sense should be used in the treatment decisions. Drug treatment can range from systemic antibiotics, corticosteroids, and intralesional or systemic antimitotics to alternative drugs such as allopurinol. Surgical treatment includes simple incision and local expression for drainage, aspiration, and excision. Surgical excision is considered the last option for most researchers1-6. In choosing treatment, it should be considered whether an infectious process, inflammatory process (granulomas), or overcorrection is involved.
We believe that aspiration or tentative drainage for removing the injected silicon5 are ineffective. Liposuction is indicated for cases of overcorrection with fat grafting.
In addition to surgical excision, other techniques can have favorable results. The lip can be reduced with mucosal excision in the shape of an ellipse8 or diamond9 that leaves the vermilion intact but indirectly reduces it. Otherwise, as in the present case, excision can be performed directly on the vermilion in the shape of an ellipse (classic vermilionectomy)10,11, w-plasty12,13, bikini7, or, as described here, modified bikini. In a classic vermilionectomy, the resulting scar on the vermilion is linear, representing a greater chance of scar retraction compared to w-plasty13. With the bikini and modified bikini techniques, the resulting scar is also linear, so we can theoretically extend this comparison to these techniques.
Regarding the patient's postoperative progress, dehiscence of the full extension of the suture line was observed. Some factors may have contributed to this complication: intense fibrosis secondary to the presence of silicone, scar tissue with poor vascularization, and topography of the treated area, where food and drinks are constantly in contact, the constant tension that the wound is subjected to speech, chewing, and facial expressions. In this case, we handled the dehiscence of the suture line conservatively with spot cleaning, hydrogen peroxide and mouthwash, hydration, and topical steroids, which produced a favorable result. In the literature, there are reports of adverse developments such as prolonged edema, paresthesia, ecchymosis, and local induration by the formation of exuberant scar tissue underlying the suture line9.
CONCLUSION
This report shows evidence of the important role of plastic surgery as the fundamental practice of aiding in the social integration of individual patients with deformities. Large facial distortions lead to social and occupational segregation because of prejudice and non-acceptance, which isolate patients. The surgical correction performed on this patient's lips created a socially acceptable aesthetic that offered him a life without limitations.
REFERENCES
1. Barnett JG, Barnett CR. Silicone augmentation of the lip. Facial Plast Surg Clin North AM. 2007;15(4):501-12.
2. Fulton JE Jr, Porumbs S, Caruso JC, Shitabata PK. Lip augmentation with liquid silicone. Dermatol Surg. 2005;31(4):1577-86.
3. Vargas FR, Amorim NG, Pitanguy, I. Complicações tardias dos preenchimentos permanentes. Rev Bras Cir Plast. 2009;24:71-81.
4. Rohrich RJ, Monheit G, Nguyen AT, Brown SA, Fagien S. Soft tissue filler complications: the important role of biofilm. Plast Reconstr Surg. 2010;125(4):1250-56.
5. Lemperle G, Gauthier-Hazan N. Foreing body granulomas after all injectable dermal fillers: part 2. Treatment options. Plast Reconstr Surg. 2009;123(6):1864-73.
6. Alam M, Dover JS. Management of complications and sequelae with temporary injectable fillers. Plast Reconstr Surg. 2007;120(65):98-105.
7. Fanous N, Brousseau VJ, Yoskovitch A. The "Bikini" lip reduction: an approach to oversized lips. Plast Reconstr Surg. 2008;122:23e-25e.
8. Pierce HE. Cheiloplasty for redundant lips. J Natl Med Assoc. 1976;68(3):211-12.
9. Botti, G. , Botti, C. H., and Cella, A. A simple surgical remedy for iatrogenic excessively thick lips. Plast Reconstr Surg. 2002;110:1329.
10. Kurth ME. "Lip Shave" or vermilionectomy: Indications and technique. Br J Plast Surg. 1957;10:156-62.
11. Spira M, Hardy B. Vermilionectomy. Review of cases with variations in technique. Plast Reconstr Surg. 1964;33:39-46.
12. Fernandez Vozmediano JM, Romero Cabrera MA, Carrascosa Cerquero A. Vermilionectomy using the Wplasty technique. J Dermatol Oncol. 1989;15:627-29.
13. Rossoe EWT, Tebcherani AJ, Sittart JA, Pires MC. Actinic cheilitis: aesthetic and functional comparative evaluation of vermilionectomy using the classic and W-plasty techniques. An Bras Dermatol. 2011;86(1):65-73.
1 - Member of the Brazilian Society of Plastic Surgery - Plastic Surgeon
2 - Member of the Brazilian Society of Plastic Surgery - Plastic Surgeon
3 - Full Professor of Plastic Surgery at the Federal Fluminense University - Assistant Professor at the Institute Ivo Pitanguy
4 - Member of the Brazilian Society of Plastic Surgery - President of the Instituto Ivo Pitanguy
5 - Patron of the Brazilian Society of Plastic Surgery - Full Professor of the Graduate Course in Plastic Surgery at the Medical School of Graduate Studies at the Pontifical Catholic University of Rio de Janeiro and the Postgraduate Course in Plastic Surgery of the Carlos Chagas Medical Graduate Studies Institute; Head of the 38th Ward of the Santa Casa da Misericordia of Rio de Janeiro (SCM-RJ); Full Member of the Brazilian Society of Plastic Surgery; Full Member of the National Academy of Medicine and the Brazilian Academy of Letters; FACS, FICS, TCBC
Institution: Ivo Pitanguy Institute
Corresponding author:
Pablo Maricevich
Av. Antônio de Góes 275, sala 407 - Pina
Recife - PE - CEP: 51110-000
E-mail: jpmaricevich@hotmail.com
Article received: June 6, 2011
Article accepted: July 29, 2011


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter