

Original Article - Year 2014 - Volume 29 -
Brachioplasty after bariatric surgery: evaluation of patient satisfaction
Braquioplastia pós-gastroplastia: avaliação da satisfação dos pacientes
ABSTRACT
INTRODUCTION: Upper limb deformity caused by massive weight loss can be corrected by brachioplasty. This plastic surgery improves limb contour, facilitates hygiene, and enables use of certain clothing.
strong>OBJECTIVE: To present the cases, describe interventions and complications, and evaluate the satisfaction of patients who underwent brachioplasty after bariatric surgery.
METHOD: Herein, 34 patients (including 33 females) aged 46.6 ± 12 years, who underwent brachioplasty after bariatric surgery, were recruited for the study. Interventions and complications associated with the surgical procedure were described, and the satisfaction of 33 patients was evaluated by a qualitative interview and specific questionnaire.
RESULTS: As a minor complication, slight dehiscence was observed in five patients (14.7%), but no major surgical complications were seen. Some degree of satisfaction was reported by 81.8% of the patients, and the outcome achieved in 69.7% was close to that expected.
CONCLUSIONS: The brachioplasty techniques that were used restored proper arm contour with a low rate of minor complications, and a high degree of satisfaction among the patients evaluated.
Keywords: Brachioplasty; Plastic Surgery; Bariatric Surgery; Surgical Complications; Patient Satisfaction; Quality of life.
RESUMO
INTRODUÇÃO: A deformidade dos membros superiores, causada pela perda ponderal maciça, pode ser corrigida por meio da braquioplastia. Essa cirurgia plástica visa melhorar o contorno dos membros, facilitar a higiene e possibilitar o uso de determinadas vestimentas.
OBJETIVO: Demonstrar casuística, relatar intercorrências e complicações e avaliar a satisfação de pacientes submetidos à braquioplastia após gastroplastia.
MÉTODO: Trinta e quatro pacientes (97% mulheres, idade 46,6 ± 12 anos) submetidos à braquioplastia após cirurgia bariátrica foram recrutados para o estudo. Descrevemos a ocorrência de intercorrências e complicações associadas ao procedimento cirúrgico e avaliamos a satisfação de 33 pacientes por meio de entrevista qualitativa e questionário específico.
RESULTADOS: Como complicações menores, observou-se pequena deiscência em cinco pacientes (14,7%); não foram observadas complicações cirúrgicas maiores. O grau de satisfação foi obtido em 81,8% dos pacientes e o resultado alcançado ficou próximo das expectativas de 69,7% deles.
CONCLUSÕES: As técnicas utilizadas de braquioplastia pós-bariátrica restabeleceram o adequado contorno braquial, com baixo índice de complicações menores e alto grau de satisfação dos pacientes avaliados.
Palavras-chave: Braquioplastia; Cirurgia plástica; Cirurgia bariátrica; Complicações cirúrgicas; Satisfação do paciente; Qualidade de vida.
Bariatric surgery facilitates significant and sustained weight loss1. After bariatric surgery, body contours change; excess skin forms large folds on different parts of the body, such as the upper and lower extremities, abdomen, breasts, and face. This body dysmorphia impairs the quality of life of the patients who undergo this surgical procedure2.
In the arms, this dysmorphia is characterized by the loss of cylindrical contour; this is caused by the development of a skin fold of variable size, which can extend from the elbow to the axilla or beyond, and even to the lateral wall of the chest (Figure 1). This deformity is due to the loss of fat content, the limited capacity of the skin to retract, and by sagging induced by distesion of the superficial fascia3,4.
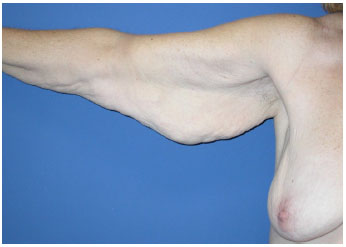
Figure 1 (A). Excess skin in the right arm after a weight loss of 49 kg - Frontal view.
Brachioplasty after bariatric surgery removes hanging excess skin-fat, and improves arm contour, making it more cylindrical and balanced; this results in greater amplitude of movement and encourages use of lighter clothing, such as T-shirts or sleeveless shirts4,6. Improvement of this surgical technique has resulted in increasingly satisfactory outcomes; the higher number of bariatric surgeries explains the growing demand for brachioplasty7.
For many years, the evaluation of plastic surgery outcomes was conducted by photography. Pre- and post-operative photographic analysis can be performed by surgeons, laymen, or a combination of the two. However, the importance of the surgical technique employed for the assessment of patient satisfaction was recently reported8.
OBJECTIVE
This study aims to present the cases of brachioplasty after bariatric surgery, describes the surgical complications observed, and evaluates patient satisfaction using a questionnaire, which was developed for this purpose.
METHOD
The cohort in this retrospective study was composed of 34 patients, including 33 females, who had significant weight loss after bariatric surgery using the restrictive-malabsorptive Fobi-Capella technique9. Between 2007 and 2012, all patients underwent brachioplasty within 5 years (6.8 + 3.2 years) after bariatric surgery.
All patients who underwent brachioplasty maintained a stable weight for at least the prior 12 months.
Patients who lost weight with clinical treatments, such as diet and food reeducation, and those who did not complete the questionnaire, were excluded from the study.
We collected data on gender, age, time interval between bariatric surgery and brachioplasty (TBB), operative time (OT), hospitalization time (HT), and prebariatric surgery and prebrachioplasty body weight and body mass index (BMI) (Table 1).
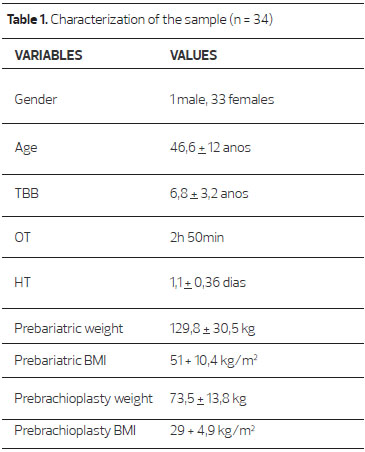
In this group of 34 patients, brachioplasty was performed at age 46.6 + 12 years, 6.8 + 3.2 years after bariatric surgery. Prebariatric BMI was 51 + 10.4 kg/m2 and 29 + 4.9 kg/m2 after bariatric surgery. The average operative time was 170 minutes.
Patients who only underwent brachioplasty (n=26, 76.5%) were hospitalized for a day and discharged with guidelines of postoperative care to be followed. Patients who underwent combined surgery (n=8, 23.5%) were hospitalized for 2 days.
Surgical procedure
First, a straight line is drawn on the medial arm, which remains hidden as much as possible when the arms are placed next to the body. With a bidigital clamping technique, and with the arm abducted to 90º and elbow flexed at 80º, elliptical lines were drawn in a spindle pattern, corresponding to excess skin to be resected without excess tension. This spindle pattern usually extended from the anterior axillary line to 2cm proximal to the medial epicondyle. Along the axillary pre-hairline and parallel to it, a second spindle of skin is demarcated perpendicular to the first, for resection of skin flaps. After rigorous hemostasis, superficial fascial suspension is carried out by plication of the fascia and synthesis by planes10. This demarcation will result in a "T"-shaped scar, with or without extension to the chest (Figures 2 and 3)4,11-13.
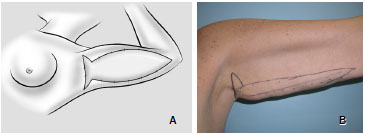
Figure 2 (A). "T" Technique - Method of "fish tail" demarcation. (B). Preoperative patient demarcation.

Figure 2 (B). Back view.
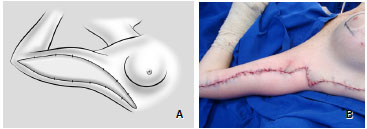
Figure 3 (A) - "T" Technique extending to the chest - Method of excess skin demarcation. (B) - Immediate post-operative period showing a detail of the plastic surgery and axillary "Z".
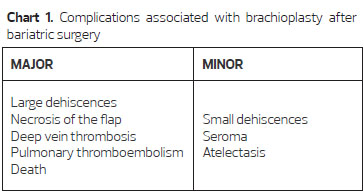
In all cases, general anesthesia and prophylactic antibiotic therapy was administered, and all patients were operated on by the same surgical team. Complications associated with brachioplasty were tabulated and classified as major or minor (Chart 1).
Satisfaction Questionnaire
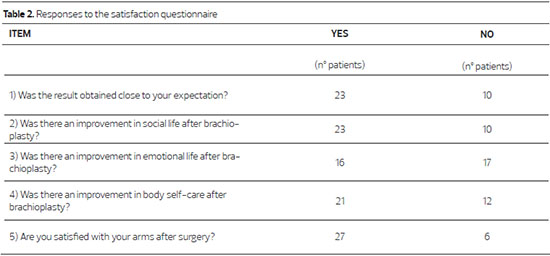
Satisfaction with plastic surgery outcomes was estimated using a questionnaire that was specifically developed for this study. Five items were evaluated: surgical outcome vs. expectation, improvement in social and emotional life, improvement in body self-care, and satisfaction with arms after brachioplasty. Each item was answered "yes" or "no."
Statistics
All scores obtained were tabulated and statistically analyzed. Numerical results are presented as average ± standard deviation.
RESULTS
No major complications associated with brachioplasty were observed. However, five cases of small dehiscences were a minor complication (14.7%), with no cases of seroma or atelectasis.
The satisfaction questionnaire was administered to 33 patients. Of these, 23 patients (69.7%) stated that the outcome obtained was close to their expectations, 23 (69.7%) reported an improvement in social life, 16 (48.5%) reported an improvement in emotional life, 21 reported improved body self-care (63.6%), and 27 (81.8%) were satisfied with their arms after plastic surgery (Table 2).
DISCUSSION
Brachioplasty is a technically well-established surgery and is specifically indicated in patients with massive weight loss. However, issues such as positioning of the scar14, among others, remain subjects of discussion.
The most used classifications, such as those of Teimourian15 and El Khatib16, correlate the type of deformity to the indicated surgical treatment. El Khatib16 clinically classified brachial ptosis into five groups, which aids planning of the surgical approach.
This study evaluated postoperative satisfaction with the arms in patients with brachial ptosis stages 3 and 4; these patients underwent extensive brachioplasty, with or without extension to the chest.
In this study, there were no major surgical complications; minor complications included five cases of small dehiscence, which resolved spontaneously.
The questionnaire evaluated patient satisfaction after brachioplasty, and indirectly assessed improvement in the quality of life.
Most patients were satisfied with the results (81.81%) and the outcome that was most appreciated was the ability to wear lighter clothing. Of six dissatisfied patients (18.2%), one complained about a hypertrophic scar and the other about the asymmetry between limbs, complications inherent to the surgical procedure. Four patients reported excess skin as the cause of dissatisfaction.
Ten patients (30.3%) reported that the outcome was far from expectations, claiming persistent brachial sagging. These patients had a prebariatric surgery BMI greater than 42 kg/m2, and four were morbidly obese, with a BMI above 50 kg/m2; this may explain the difficulty in removing excess skin.
Patients who denied an improvement in social (30.3%) or emotional life (51.5%) after brachioplasty claimed that any improvement was due to the bariatric surgery, with no positive or negative benefit from subsequent plastic surgery.
Of the 33 patients interviewed, 21 (63.6%) reported improvement in body self-care after brachioplasty, attributing this to the removal of excess skin and an increase in self-esteem. The remaining patients (36.4%) reported no change in body self-care, with no influence by plastic surgery.
CONCLUSION
The results obtained in this series of patients permits an inference that postbariatric brachioplasty can be considered a safe procedure, which may be indicated in patients with stable weight and upper extremity dysmorphia due to excess skin.
This procedure restores proper arm contour, resulting in functional and esthetic benefits, a high degree of satisfaction, and improvement in self-esteem, with positive effects on the quality of life.
REFERENCES
1. Geloneze B, Pareja JC. Cirurgia bariátrica cura a síndrome metabólica? Arq Bras Endocrinol Metab. 2006;50(2):400-7.
2. Cintra Junior W, Modolin ML, Faintuch J, Gemperli R, Ferreira MC. Quality of life after abdominoplasty in women after bariatric surgery. Obes Surg. 2008;18:728-32.
3. Orpheu SC, Coltro PS, Scopel GP, Gomez DS, Rodrigues CJ, Modolin ML et al. Collagen and elastic content of abdominal skin after surgical weight loss. Obes Surg. 2010;20(4):480-6.
4. Modolin M, Cintra Jr W, Faintuch J, Silva MM, Moraes LB, Gemperli R, Ferreira MC. Improved double-fuse technique for post-bariatric brachioplasty. Rev Col Bras Cir 2011;38(4):217-22.
5. Baroudi R. Dermolipectomy of the upper arm. Clin Plast Surg. 1975;2:485-91.
6. Regnault P. Brachioplasty, axilloplasty and pre-axilloplasty. Aesthet Plast Surg. 1983;7:31-6.
7. Symbas JD, Losken A. An outcome analysis of brachioplasty techniques following massive weight loss. Ann Plast Surg. 2010;64(5):588-91.
8. Cintra Junior W. Mastopexia com inclusão de implantes mamários após tratamento cirúrgico da obesidade mórbida: avaliação da satisfação das pacientes e resultados cirúrgicos. [Tese de Doutoramento]. São Paulo: Universidade de São Paulo; 2010.
9. Capella RF, Capella JF. Reducing early technical complications in gastric bypass surgery. Obes Surg. 1997;7(2):149-56.
10. Lockwood T. Brachioplasty with superficial fascial system suspension. Plast Reconstr Surg. 1995;96(4):912-20.
11. Pitanguy I. Correction of lipodystrophy of the lateral thoracic aspect and inner side of the arm and elbow dermosenescence. Clin Plast Surg. 1975;2(3):477-83.
12. Aly A, Pace D, Cram A. Brachioplasty in the patient with massive weight loss. Aesthet Surg J. 2006;26(1):76-84.
13. Hurwitz DJ, Holland SW. The L brachioplasty: an innovative approach to correct excess tissue of the upper arm, axilla and lateral chest. Plast Reconstr Surg. 2006;117(2):403-11; discussion 412-3.
14. Samra S, Sawh-Martinez R, Liu YJ, Samra F, Persing JA. Optimal placement of brachioplasty scar: a survey evaluation. Plast Reconstr Surg 2010;126(suppl 4S): 77 (abstract).
15. Teimourian B, Malekzadeh S. Rejuvenation of the upper arm. Plast Reconstr Surg. 1998;102(2):545-51.
16. El Khatib HA. Classification of brachial ptosis: strategy for treatment. Plast Reconstr Surg. 2007;199(4):1337-42.
1 - Doctor of Plastic Surgery, Faculty of Medicine of the University of São Paulo (FMUSP) - Medical Assistant at HCFMUSP and the State Institute of Medical
2 - Assistance and Public Service (IAMSPE)
3 - Medical Assistant in the Division of Plastic Surgery of HCFMUSP - Member of the Brazilian Society of Plastic Surgery (BSPS)
4 - Academic at the Faculty of Medicine of the University of São Paulo - Undergraduate Student at the FMUSP
5 - Medical Assistant in the Division of Plastic Surgery of HCFMUSP - Member of the BSPS
6 - Medical Resident in the Division of Plastic Surgery of HCFMUSP - Medical Resident in the Plastic Surgery Program of the FMUSP
Institution: Plastic Surgery and Burn Service of the Clinical Hospital of the Faculty of Medicine (HCFM) - USP.
Corresponding author:
Wilson Cintra Juúnior
Avenida São Gabriel, 201 - conj. 704/5, Itaim Bibi
São Paulo, SP. CEP: 01435-001
E-mail: wcintra@terra.com.br
Article received: January 6, 2014
Article accepted: March 4, 2014


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter