

Ideas and Innovation - Year 2014 - Volume 29 -
Breast reconstruction with excess reverse abdominoplasty flap
Reconstrução de mama com retalho excedente de abdominoplastia reversa
ABSTRACT
INTRODUCTION: Mastectomy is a highly traumatic procedure for many women, and mammary reconstruction is a fundamental part of the treatment. Reconstruction has been shown to improve the psychosocial wellbeing and quality of life of these patients, and several techniques and advancements thereof have been described in order to reach the current diversity of modern procedures, whether associated with breast implants or not. This diversity in techniques enables an appropriate selection for each individual case, thus attaining better results. The objective of this report was to present an alternative breast reconstruction method using an upper abdominal flap along with breast implants.
METHOD: A 59-year-old woman had undergone right radical mastectomy and three previous breast reconstruction operations with silicone prostheses, without success. We first performed reverse abdominoplasty with exploitation of an excess right flap used as prosthesis coverage. Two years later, we performed contralateral breast symmetrization using mastopexy with a change of prosthesis.
RESULT: The planned breast volume reconstruction was achieved. Discrete inflammatory signals were observed in the immediate postoperative period, mainly in the upper pole, and treated with corticosteroid therapy for two weeks; this resulted in complete regression of all signs and symptoms. Seroma was aspirated (20 ml) with a syringe on the 15th postoperative day, with no recurrence. No complications, such as epitheliolysis or flap necrosis, occurred.
CONCLUSION: Breast reconstruction with an abdominal flap from reverse abdominoplasty may be an option in a subset of cases, and offers satisfactory results.
Keywords: Breast cancer; Reconstruction; Implant; Reverse abdominoplasty; Skin/abdominal flap.
RESUMO
INTRODUÇÃO: A mastectomia é um procedimento muito traumático para a mulher. A reconstrução mamaria é parte fundamental do tratamento para melhorar o bem estar psicossocial e a qualidade de vida destas pacientes. Muitas técnicas foram descritas e evoluíram até chegar à atual diversidade de procedimentos modernos associados ou não as próteses mamárias. Esta diversidade de técnicas possibilita a seleção adequada para cada caso, oferecendo melhores resultados. O objetivo deste trabalho é apresentar uma alternativa cirúrgica de reconstrução mamária com retalho de abdome superior associado à prótese mamária.
MÉTODO: paciente de 59 anos com mastectomia radical direita e três cirurgias prévias de reconstrução mamária com prótese de silicone, sem sucesso. Foi utilizada abdominoplastia reversa com aproveitamento do retalho excedente direito para cobertura de prótese no mesmo tempo cirúrgico. Simetrização da mama contralateral foi obtida dois anos depois, através de mastopexia com troca de prótese.
RESULTADO: Foi obtido o resultado planejado para reconstrtução do volume mamário. Discretos sinais inflamatórios no pós-operatório imediato, principalmente no polo superior, tratado com corticoterapia por duas semanas, com regressão completa dos sinais e sintomas. Aspirado seroma (20ml) com seringa no dia 15º pós cirúrgico, sem recidiva. Não ocorreram complicações como epiteliólise ou necrose do retalho.
CONCLUSÃO: A reconstrução mamária com retalho abdominal resultante de abdominoplastia reversa pode ser uma opção em casos especiais, oferecendo resultado satisfatório.
Palavras-chave: Câncer mamário; Reconstrução; Implante; Abdominoplastia reversa; Retalho cutâneo/abdominal.
Breast reconstruction is a fundamental aspect of mastectomy, and has been demonstrated to improve the psychosocial well-being and quality of life of these patients 1.
The first attempts at breast reconstruction date back to the late 19th century2-5, with William Halsted, based on Rudolph Virchow's theory, performing the first radical mastectomy in 18892 and considered that plastic surgery interfered with the local control of cancer, and thus recommended avoiding reconstructive surgery in the mastectomized region.
Harold Gilles (1942) used distant skin flaps (tubed flaps of the abdomen and lower chest) to perform the first breast reconstruction 6. Despite the relatively good results at the time, this technique was abandoned due to the need for multiple surgical events and the high rate of complications and scarring sequelae3.
Currently, the trend of less aggressive mastectomy has facilitated breast reconstruction as a result of increased preservation of the dermal cutaneous tissue2.
Depending on the experience and preference of the surgeon, some of the most commonly used breast reconstruction techniques include:
Breast implants in breast reconstruction
Developed in 1961 by Cronin, Gerow, and Dow Corning Corp., and first presented in 1963, the silicone gel breast implant changed the field of breast reconstruction, creating the basis of delayed treatment7. In 1978, Jarret et al. recommended submuscular placement of the implants8.
In France, Arion presented the first tissue expander in 1965, but it was not until in 1982 that Radovan described its use in breast reconstruction9, and later, in 1984, Becker first developed a permanent tissue expander10.
Latissimus dorsi flap
The use of the latissimus dorsi muscle to restore defects caused by the absence of the pectoralis major muscle was first described in 1939 by Hutchins, but it was not until 1974 that this technique was used by Brantigan for radical post-mastectomy reconstruction; subsequently, in 1976, Olivari popularized and perfected the technique11,12.
However, due to insufficient volume, this technique usually requires placement of an implant, as described by Schneider in 197713.
Transverse rectus abdominis myocutaneous (TRAM) and free TRAM flaps
The first description of this flap was in 1979 by Robbins, who used a vertically oriented skin-muscle flap of the rectus abdominis muscle14. In 1982, Hartrampf described its use with a horizontally oriented cutaneous paddle, providing a more aesthetic donor site closure. Its advantages include the fact that is provides sufficient tissue to cover large defects, while its disadvantages include weakness generated in the abdominal wall and a risk of hernias15.
Holmström (1979) was the first to describe the free flap of the rectus abdominis16, and in 1989, Grotting published a study demonstrating the advantages of this technique such as improved blood supply, reduced risk of necrosis, and improvements in the functional loss of the abdominal wall17.
Other, no less important, techniques include the deep and superficial inferior epigastric perforator and artery flaps (DIEP and SIEA)18-23, superior and inferior gluteal artery perforator free flaps (SGAP and IGAP)24,25, local dermal-fat and fasciocutaneous flaps 26-31, and upper abdominal flap32-35.
In 2009, Deós36 revisited and applied new concepts to the reverse abdominoplasty37,38, correcting the drawbacks of the original technique, with strategic planning in terms of the markup, flap positioning, and maintenance of a stable scar, referring to this new technique as "tensioned reverse abdominoplasty ".
Although used in many surgical situations, there are no previous reports of reverse abdominoplasty for providing an additional subcutaneous tissue for breast reconstruction to protect the silicone prosthesis. In 1992, Berrino compared different reconstructive techniques for type II breast deformities39, one being a flap obtained by reverse abdominoplasty, but did not present any major conclusions or detailed the technique. Nonetheless, reverse abdominoplasty may represent a practical option for breast reconstruction in carefully selected patients.
OBJECTIVE
The aim of the present report was to describe an alternative breast reconstruction method performed using an upper abdominal flap during reverse abdominoplasty.
METHOD
A 59-year-old female patient with a history of radical mastectomy for cancer in the right breast had undergone three previous procedures (in 1997, 2007, and 2009) for breast reconstruction with implants, without success. In the last surgery, a contralateral breast prosthesis was placed with the purpose of symmetrization.
Local physical examination findings:
a) Absence of right breast volume, scar retraction, and thin skin adhering to the deep planes, without subcutaneous tissue and with traces of the nipple areola complex.
b) Contralateral breast with volume provided by silicone prosthesis, without changes.
c) Upper abdominal flaccidity with sufficient fat volume to use as a dermal-fat flap for covering the breast implant.
Surgical Technique
The incision of the reverse abdominoplasty was clearly marked, following the mammary fold and midline up to the xiphoid process. The breast area D, which should be detached from the deep layers, is based on the fold and upper pole of the contralateral breast (Figure 1). After incision and reverse detachment of the supraumbilical abdomen, the abdominal flap was fixed with adhesion sutures, followed by five traction sutures to fix it to the muscle fascia in order to prevent it from sliding down (Figure 2 A-B). The excess right dermal-fat flap was decorticated in its distal half, pulled in the cephalic direction and invaginated under the previously detached skin of breast region D, serving as a protective cushion for the breast implant. The skin of the lower portion was maintained for reconstruction of the lower breast pole (Figure 3 A-D).

Figure 1. Markup.
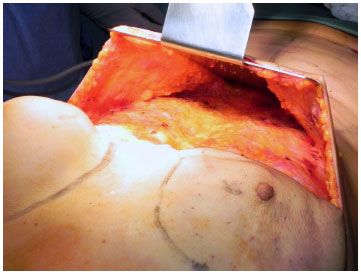
Figure 2. (A) - Flap detachment.
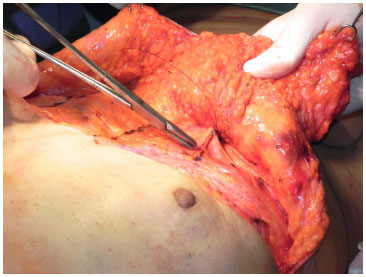
Figure 2. (B) - Adhesion sutures.

Figure 3. (A) - Evaluation of the excess upper abdominal flap.

Figure 3. (B) - Assessment of the area to be decorticated and invaginated.

Figure 3. (C) - Upper portion of the decorticated flap.

Figure 3. (D) - Invagination of the decorticated flap.
The excess left flap was discarded and accommodated to the edge of the breast fold on that side.
The de-epithelialized dermal-fat flap was set in the upper pole by five mattress sutures through the skin, impeding the sliding of the flap (Figure 4. A-B). Thereafter, a 255-ml polyurethane breast implant was placed.
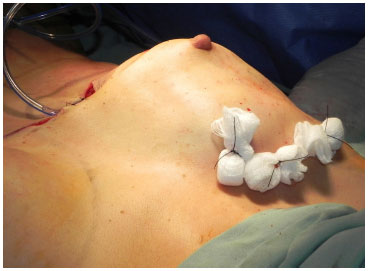
Figure 4. (A) - Upper portion of the decorticated flap fixed superiorly with mattress sutures.

Figure 4. (B) - End suture and placement of a vacuum drain.
The formation of the new infra-mammary fold was created using attachment points from the periosteum of the 6th rib.
A vacuum drain was placed in the detached abdominal area as well as in the breast implant pocket D, with outlets in the medial and lateral scar, respectively, and removed on the 4th day after surgery, with a net volume of less than 30ml.
The sutures were performed at three levels: subcutaneous (Monocryl 3-0), subdermal (Monocryl 4-0), and skin (nylon 5/0). The mattress and skin sutures were removed on the 7th and 12th postoperative days, respectively.
Two years later, symmetrization was obtained through mastopexy with a change of the polyurethane prosthesis in the left breast (255ml to 145ml).
RESULTS
In the immediate postoperative period, the patient presented signs of inflammation in the right breast area, especially in the upper pole, which were treated with corticosteroid therapy for two weeks, resulting in complete regression of all signs and symptoms.
Seroma (20 ml) was aspirated with a syringe on the 15th day after surgery, with no recurrence.
The sternal region (at the height of the drain) presented a small suture dehiscence, resulting in a hypertrophic and unsightly scar; this scar was revised 13 months after surgery.
Figure 5 shows the preoperative findings, and Figure 6 shows the results of the reconstruction and symmetrization after the second surgical procedure (two years later).

Figure 5. (A) - Preoperative frontal view.

Figure 5. (B) - Preoperative oblique view.

Figure 5. (C) - Preoperative profile.

Figure 6. (A) - Postoperative frontal view.

Figure 6. (B) - Postoperative profile.

Figure 6. (C) - Postoperative profile.
DISCUSSION
Mastectomy is highly traumatic for many women, and breast reconstruction is an essential procedure to improve the psychosocial well-being and quality of life of these patients 1.
Conservative techniques7,8 involving breast prostheses9,10 have changed the trends in breast reconstruction, and influenced the advances of several modern techniques. The resulting diversity of breast reconstruction techniques enables an adequate selection for each individual case, thus offering better results.
Most breast reconstruction procedures provide sufficient coverage and volume2,4,9,14; however, breast prostheses are essential to enhance the volume and shape of the breasts and for improving the results8-10.
In some cases, despite having preserved anatomy, the subcutaneous tissue may be scarce or absent, hence preventing the placement of the prostheses.
In such cases, when placed, they may externalize and require removal.
In addition, many procedures use local flaps of the upper abdominal region for breast reconstruction27-31. Reverse abdominoplasty, initially described by Rebello-Franco37 and recently reviewed and improved by Deós, can provide sufficient tissue from the upper abdomen to cover the breast implant36.
Alternatively, the excess flap resulting from reverse abdominoplasty may be another option for breast reconstruction in well-selected patients who have supra-umbilical abdominal flaccidity.
CONCLUSION
Breast reconstruction with an abdominal flap resulting from reverse abdominoplasty displayed satisfactory results in the case described herein, and may represent an alternative option for breast reconstruction in a select patient population.
REFERENCES
1. Wilkins EG, Cederna PS, Lowery J, et al. Prospective analysis of psychosocial outcomes in breast reconstruction: one year postoperative results from the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg. 2000;106:1014-1025.
2. Wickman M. Breast reconstruction--past achievements, current status and future goals. Scand J Plast Reconstr Hand Surg. 1995;29:81-100.
3. Goldwyn RM. Vincenz Czerny and the beginnings of breast reconstruction. Plast Reconstr Surg. 1978;61:673-681.
4. Maxwell GP. Iginio Tansini and the origin of the latissimus dorsi musculocutaneos flap. Plast Reconstr Surg. 1980;65:686-692.
5. Teimourian B, Adham MN. Louis Ombredanne and the origin of muscle flap use for immediate breast mound reconstruction. Plast Reconstr Surg. 1983;72:905-910.
6. Gillies HD, Millard DR Jr. The principles and art of plastic surgery. Boston: Little, Brown & Co. 1957:175-179.
7. Cronin TD, Gerow F. Augmentation mammaplasty: a new "natural feel" prosthesis. In: Broadbent TR, editor. Transactions of the Third International Congress of Plastic Surgery. Amsterdam: Excerpta Medica.1964:4-49.
8. Jarrett JR, Cutler RG, Teal DF. Subcutaneous mastectomy in small, large, or ptotic breasts with immediate submuscular placement of implants. Plast Reconstr Surg. 1978;62:702-705.
9. Radovan C. Breast reconstruction after mastectomy using the temporary expander. Plast Reconstr Surg. 1982;69:195-208.
10. Becker H. Breast reconstruction using an inflatable breast implant with detachable reservoir. Plast Reconstr Surg. 1984;73:678-683.
11. Brantigan OC. Evaluation of Hutchins' modification of radical mastectomy for cancer of the breast. Am Surg. 1974;40:86-88.
12. Olivari N. The latissimus flap. Br J Plast Surg. 1976;29:126-28.
13. Schneider WJ, Hill HL Jr, Brown RG. Latissimus dorsi myocutaneous flap for breast reconstruction. Br J Plast Surg. 1977;30:277-281.
14. Robbins TH. Rectus abdominis myocutaneous flap for breast reconstruction. Aust N Z J Surg. 1979;49:527-530.
15. Hartrampf CR, Scheflan M, Black PW. Breast reconstruction with a transverse abdominal island flap. Plast Reconstr Surg. 1982;69:216-225.
16. Holmström H. The free abdominoplasty flap and its use in breast reconstruction. An experimental study and clinical case report. Scand J Plast Reconstr Surg. 1979;13:423-427.
17. Grotting JC, Urist MM, Maddos WA, Vasconez LO. Conventional TRAM flap versus free microsurgical TRAM flap for immediate breast reconstruction. Plast Reconstr Surg. 1989;83:828-844.
18. Futter CM, Webster MH, Hagen S, Mitchell SL. A retrospective comparison of abdominal muscle strength following breast reconstruction with a free TRAM or DIEP flap. Br J Plast Surg. 2000;53:578-583.
19. Taylor GI, Palmer JH. The vascular territories (angiosomes) of the body: experimental study and clinical applications. Br J Plast Surg. 1987;40:113-141.
20. Allen RJ, Treece P. Deep inferior epigastric perforator flap for breast reconstruction. Ann Plast Surg. 1994;32:32-38.
21. Allen R. The superficial inferior epigastric artery free flap: an anatomic and clinical study for the use in reconstruction of the breast. Presented at the 33rd Annual Meeting of the Southeastern. Society of Plastic and Reconstructive Surgeons. Kiawah (SC), June 3-7, 1990.
22. Arnez ZM, Khan U, Pogorelec D, Planinsek F. Breast reconstruction using the free superficial inferior epigastric artery (SIEA) flap. Br J Plast Surg. 1999;52:276-279.
23. Chevray PM. Breast reconstruction with superficial inferior epigastric artery flaps: a prospective comparison with TRAM and DIEP flaps. Plast Reconstr Surg. 2004;114:1077-1083.
24. Allen RJ, Levine JL, Granzow JW. The in-the-crease inferior gluteal artery perforator flap for breast reconstruction. Plast Reconstr Surg. 2006;118:333-339.
25. Granzow JW, Levine JL, Chiu ES, Allen RJ. Breast reconstruction with gluteal artery perforator flaps. J Plast Reconstr Aesthet Surg. 2006;59:614-621.
26. Mendes F, Figueiredo JC, Pereira WB, Mélega JM. Reconstrução mamária: uma revisão e classificação de técnicas. In: Tournieux AA, CURI MM. Atualização em cirurgia plástica - SBCP, São Paulo: Robe editorial, 1996. p.341-351.
27. Longracre JT. The use of local pedicle flaps for reconstruction of the breast after subtotal or total extirpation of the mammary gland and for the correction of distortion and atrophy of the breast due to excessive scar. Plast Reconstr Surg (1946). 1953;11:380-403.
28. Baroudi R, Pinotti JA, Keppke EM. A transverse thoraco-abdominal skin flap for closure after radical mastectomy. Plast Reconstr Surg. 1978;6:547-554.
29. de Souza PE, da Costa MA, Erazo P, Cação EG, de Souza PA. Reconstrução Mamária: Princípios Geométricos dos Retalhos Cutâneos em Duplo V. Rev Soc Bras Cir Plist. 1998;13:19-42.
30. Holmström H, Lossing C. The lateral thoracodorsal flap in breast reconstruction. Plast Reconstr Surg. 1986;77:933-943.
31. Pitanguy I, Caldeira AM, Alexandrino A, Trevino MN, Calixio CA. Retalho braquial fasciocutâneo - técnica de Pitanguy para deformidade infraclavicular pós-mastectomia. Rev Bras Cir. 1984;74:349.
32. Lewis JR Jr. Use of a sliding flap from the abdomen to provide cover in breast reconstruction. Plast Reconstr Surg. 1979;64:491-497.
33. Leal PR, de Souza AF. Breast reconstruction by expansion and advancement of the upper abdominal flap. Aesthetic Plast Surg. 1997;21:175-179.
34. Zienowicz RJ, Karacaoglu E. Augmentation mammaplasty by reverse abdominoplasty (AMBRA). Plast Reconstr Surg. 2009;124:1662-1672.
35. Pantelides NM, Mondal D, Wishart GC, Malata CM. Reverse abdominoplasty: a practical option for oncological trunk reconstruction. Eplasty. 2013;13:e2.
36. Deos MF, Arnt RA, Gus EI. Tensioned reverse abdominoplasty. Plast Reconstr Surg. 2009;124:2134-2141.
37. Rebello C, Franco T. Abdominoplastia pela incisão sub-mamária. Rev Bras Cir. 1972;7:249-252.
38. Baroudi R, Keppke EM, Carvalho CG. Mammary reduction combined with reverse abdominoplasty. Ann Plast Surg. 1979;2:368-373.
39. Berrino P, Campora E, Leone S, Santi P. Correction of type II breast deformities following conservative cancer surgery. Plast Reconstr Surg.1992;90:846-853.
1 - Regent of accredited service by the BSPS; Director, Desc; Former-President of the BSPS, International Editor of the PRS
2 - MD - Postgraduate in Plastic Surgery, UNISANTA
3 - MD - Postgraduate in Plastic Surgery, UNISANTA
4 - MD - Specialist in Plastic Surgery, UNISANTA
5 - MD - Specialist in General Surgery, Santa Casa de Misericórdia de Santos
Institution: Clinica Osvaldo Saldanha, Regent of Accredited Service.
Corresponding author:
Osvaldo Ribeiro Saldanha
Avenida Washington Luiz, 142 - Vila Mathias
Santos - SP. CEP: 11050-200
E-mail: clinica@clinicasaldanha.com.br
Article received: December 3, 2013
Article accepted: March 4, 2014


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter