

Original Article - Year 2014 - Volume 29 -
Endoscopically assisted rhytidoplasty of the lower third of the face: the videoendoscopic corset
Ritidoplastia videoassistida do terço inferior da face: corset videoendoscópico
ABSTRACT
INTRODUCTION: In contemporary facial surgery, the focus of controversy has shifted from superficial muscular aponeurotic system approaches, to methods by which to improve the neck contour. Larger detachments, such as those resulting from the use of submental access, can provide better outcomes. However, the associated potential for increased complication rates, particularly hematomas, discourages the practice of such detachments. In order to minimize these risks, we propose the use of videoendoscopic assistance during cervicoplasty procedures, such as Feldman's method. The adjustments required to carry out this procedure are described in this study.
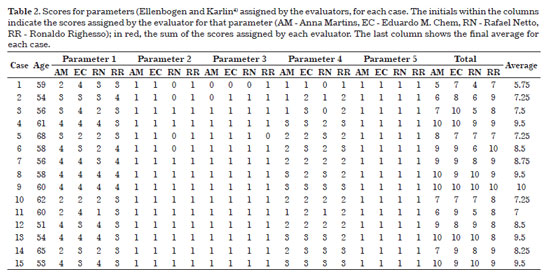
METHOD: This retrospective study included 16 patients, who were sequentially submitted to a surgical procedure in the preceding 12 months, using the technique described above. The results were scored by the main author (RR) and 3 independent plastics surgeons (EC, RN, AM), who were unaware of the details of the technique used. Preoperative and 6-month postoperative photographs were evaluated and scored according to the parameters defined by Ellenbogen and Karlin, with values ranging from 0-10 subsequently applied to the grading system of Labbé.
RESULTS: The group average postoperative score was 8.29, the optimal grade according to the scale of Labbé. An optimal outcome (8-10 points) was reached in 10 cases (62.5%); a good outcome (6-7 points) was reached in 5 cases (31.25%); a score below 6, rated as average, occurred in only one case (6.25%). There was no occurrence of hematomas, skin adhesions or recurrent platysmal bands.
CONCLUSION: The proposed technique appears to provide satisfactory results without increasing the rate of complications. Moreover, use of the technique was associated with less extended submental scar, in addition to improving the direct view of the structures manipulated for all members of the surgical team.
Keywords: Rhytidoplasty/Methods; Face/Surgery; Hematoma/Prevention and Control.
RESUMO
INTRODUÇÃO: Após um período em que a controvérsia em cirurgias faciais teve como foco a abordagem ao SMAS, atualmente se persegue a melhora do contorno cervical. Descolamentos maiores, como os praticados pelo acesso submentoniano, podem aprimorar os resultados, entretanto acarretam aumento das complicações, sobretudo de hematomas, desencorajando seu emprego. No intuito de minimizar estes riscos, propõe-se o uso adjuvante do videoendoscópio durante a realização de cervicoplastias, segundo a Técnica de Feldman. As adaptações necessárias para a realização do procedimento são detalhadas.
MÉTODO: Estudo retrospectivo de 16 pacientes submetidos a procedimento cirúrgico nos últimos 12 meses, sequencialmente, de acordo com a técnica apresentada. Os resultados foram graduados pelo autor principal (RR) e por três cirurgiões plásticos independentes (EC, RN, AM), sem que estes conhecessem detalhes da técnica empregada. Os fotogramas pré e pós-operatórios de seis meses foram avaliados e pontuados conforme os parâmetros definidos por Ellenbogen & Karlin, gerando notas 'de 0 a 10', que foram aplicadas à Grade de Labbé.
RESULTADOS: A média geral do grupo foi 8,29, escore ótimo, segundo a Escala de Labbé. Em dez casos (62,5%), atingiu-se resultado ótimo (8-10 pontos); cinco casos (31,25%), bom (6-7 pontos), e apenas um caso (6,25%), escore abaixo de 6 pontos, classificado como mediano. Não houve ocorrência de hematomas, aderências cutâneas ou recidiva das bandas platismais.
CONCLUSÃO: A técnica apresentada parece propiciar resultados adequados, sem aumento das complicações. Adicionalmente, possibilita uma cicatriz submentoniana de menor extensão, além da visualização magnificada e direta de todas as estruturas abordadas, por todos os membros da equipe.
Palavras-chave: Ritidoplastia/métodos; Face/cirurgia; Hematoma/prevenção & controle.
During cervicoplasty using Feldman's technique1,2, it has been proposed that the use of a videoendoscope may help to control difficult bleeding by aiding the achievement of hemostasis, and providing prompt resolution of the problem. Videoendoscopic assistance has since become a routine procedure in techniques that involve the cervical midline, since larger detachments may result in increased complications, particularly hematomas. Therefore, several adjustments have been made to the classical technique, leading to what we call the "videoendoscope corset", in reference to the original procedure1.
This paper reports the initial experience of the author and describes the surgical approach, which was used in 16 patients operated on in the preceding 12 months, and submitted to a follow-up of at least 6 months. The initial evaluation shows that the outcomes were similar to those obtained with the standard technique. However, the number of complications, in particular the occurrence of skin adhesions and hematoma, appears to be reduced; none of these complications occurred in the group analyzed. In addition, the use of a videoendoscope allows smaller submental incisions to be performed, and improves the view of the surgical field for all members of the team.
OBJECTIVES
To demonstrate the potential of videoendoscope-assisted platysmaplasty, and careful hemostasis in cervicoplasty procedures with a midline cervical approach, conducted after large detachments via a smaller submental incision. To assess the rate of complications with this procedure, compared with the standard technique.
METHOD
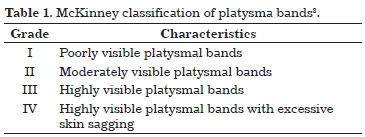
We undertook a retrospective study that included 16 patients with grade IV cervical changes, according to McKinney3 (Table 1), who underwent cervicofacial rhytidoplasty. Surgery was carried out by the first author (RR), with the assistance of a videoendoscope for the treatment of the cervical region, performed according to the procedure described below. Patients were sequentially submitted to the surgical procedure and followed up for a minimum period of 6 months. The data obtained from this group were compiled in specific protocols to be subsequently analyzed and compared with the results published in the literature.
To evaluate the surgical efficiency in promoting facial rejuvenation, the first author (RR), 2 plastic surgeons (EC and RN) and a medical resident in plastic surgery (AM) used the criteria of Ellenbogen & Karlin4 and scored each patient according to 5 parameters:
1) Defined inferior border of the mandible - 0-4 points
2) Subhyoid depression - 0-1 points
3) Visualization of the thyroid cartilage protrusion - 0-1 points
4) Visible anterior border of the sternomastoid - 0-3 points
5) Cervical-mental angle between 105 and 120º - 0-1 point
From the sum of the scores, the results were rated according to Labbé et al.5 (maximum of 10 points):
Optimal 8-10 points Good 6-7 points Average 5 points
Evaluations were performed and scores were independently assigned by assessment of photographic reports; preoperative and 6-month postoperative photographs were compared. The photographs were captured in a standard manner, using frontal, right and left profile images. The evaluators, with the exception of the first author (RR), were unaware of the surgical details, and only knew that the patients had undergone cervicofacial rhytidoplasty, carried out by the first author.
Surgical procedure
All patients underwent preoperative medical tests and a cardiac evaluation. Antihypertensive medications were maintained until the day of surgery and restarted as soon as possible postoperatively. Fifteen days before surgery, all patients were instructed to discontinue their medications in view of possible major bleeding.
Anesthesia was administered by the same anesthesiologist in all 16 cases. The preferred technique was local anesthesia combined with intravenous sedation with dexmedetomidine, administered via an infusion pump, with additional bolus doses of fentanyl and midazolam. During the induction of anesthesia, cefazolin, in a dose corresponding to 1 g and 10 mg dexamethasone, was administered intravenously.
The procedure started with planning the submental incision. With the patient sitting, posterior superior traction was applied bilaterally to the face. The incision should be hidden in the mandibular shadow, parallel to the submental crease, 0.5 cm in the caudal direction, resembling a slightly arcuate posterior line of approximately 2 to 2.5 cm in length1,2,6.
The patient was then placed in the supine position with the back slightly elevated, and preparation of the operative field was started. For anesthetic infiltration, a first solution ("anesthetic solution") was prepared by mixing 320 mL of 0.9% saline solution with 60 mL of 1% lidocaine and 20 mL of 7.5 mg/mL ropivacaine. The vasoconstrictive effect was obtained by adding 1 mg epinephrine to the solution. A second solution ("tumescent solution") was prepared with 400 mL of Ringers lactate and one vial of epinephrine (1 mg). Each hemiface received approximately 160 mL of the anesthetic solution, whereas approximately 80 mL was administered to the central neck region. Each hemiface and cervical region also received about 100 mL of tumescent solution. An 18 G abocath® was used to infiltrate the anesthetic. Once the region was infiltrated, it was necessary to wait for approximately 10 minutes to achieve vasoconstriction. In the meantime, if the surgery was predicted to last over 4 hours, urinary catheterization was performed.
The pre-auricular incision is usually carried out superiorly, in the pretragal and precapillar region, thus contouring the ear inferiorly. In the retroauricular region, the pre-auricular incision follows the retroauricular groove and extends cranially for about three-quarters of the length of the ear. The need for cutaneous resection results in a horizontal scar extension, which descends for 4-5 cm6-8.
After the infiltration, initial detachment was carried out with a blunt cannula, without performing any liposuction. The skin incision was then carried out using a No. 15 scalpel blade, followed by an approximately 5 cm dissection in the supra-superficial musculoaponeurotic system (SMAS) plane, at the auricular perimeter.
After the bilateral flap elevation of the face in the subcutaneous plane, we started to approach the cervical region. An incision of approximately 0.3 cm in length, 0.5 cm cranially to the mentonian fold, allowed detachment in the subdermal plane, using the same blunt cannula previously employed on the face. A submental incision was then carried out according to previous marking. From the incision, a Metzenbaum scissor with its curvature directed toward the depth was used to elevate the flap above the platysma muscle. This resulted in a superior base triangle with the following limits: superiorly, the bottom line of the mandible; laterally, the anterior border of the sternocleidomastoid muscle; and inferiorly, extending about 3 cm from the sternal manubrium. The dissection was also performed cranially to the submental incision. It is important that the flap contains a moderate layer of subcutaneous fat, enough to prevent adhesions or subsequent irregularities1-3,7.
After the initial stage of the dissection, the assistant placed a Senn-Miller retractor, with the claw side fixed to the jaw; applying a pulling force to the retractor maintained the cervical extension. Skin points of traction or Gilles hooks may aid expansion of the optical cavity (Figure 1). The surgeon inserted the videoendoscope assembly and started to observe the image captured and projected, via the monitor (Figure 2). Residual adhesions were released from the skin flap to the platysma using scissors. After the release, the assistant held the videoendoscope; the surgeon, whose hands were now free, used an anatomical clamp of 20 cm and long scissors to remove the excess fat located superficially over the platysma and centrally to it, until obtaining a perfect view of platysmal borders. When subplatysmal fat is removed in a conservative manner, the borders released are of approximately 1-2 cm9 (Figure 3). Through the application of medial traction to these borders (Figure 4), one was border was apposed to the other and the sides were sutured, thus promoting their invagination, as opposed to a simple approximation of the edges1,2. This suture should be performed in a double or triple plane, with 3-0 or 4-0 PDS (polydioxanone) thread (Ethicon, reference PDP496, São José dos Campos-SP, Brazil), and should extend from the submental region to approximately 3 cm from the sternal manubrium. The appearance of the platysma muscle, now merged (Figure 5), resembles a corset, hence the reference to the term "corset"1,2. This is executed using a mounting needle of 12 mm in length, 3/8 of diameter, with a triangular tip, and a Mayo-Hegar long needle holder, 20 cm in length. The cervical region was finalized by means of hemostatic revision and skin sutures. Once completed, an SMAS flap was plicated in the upper portion of the detached face, as required in each individual case6-8. Inferiorly, 2-3 double sutures with 3-0 monofilament nylon thread (Ethicon, mononylon ethilon, São José dos Campos-SP, Brazil) were performed on the lateral edge of the platysma, thus fixing it to the mastoid3,5,10.
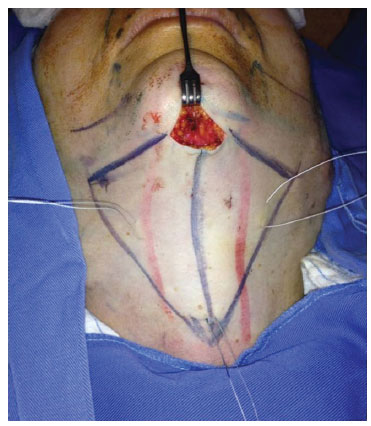
Figure 1. Detail of mandibular traction with Senn-Miller retractor and additional cutaneous sutures. The blue marks show the area to be dissected. The descending lines in red guide the position of the central bands. Note that the extent of the submental scar is approximately 2 cm.
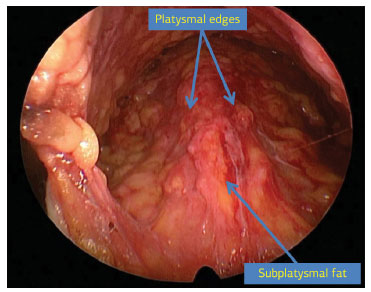
Figure 2. Videoendoscopic image of the cervical region with the arrows indicating platysmal edges and subplatysmal fat.
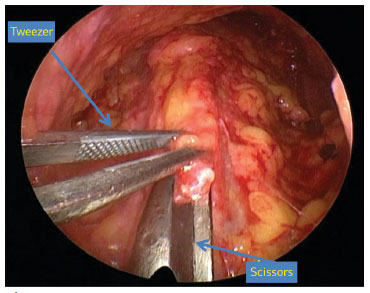
Figure 3. Endoscopic visualization of subplatysmal fat removal, seized by anatomical tweezers.
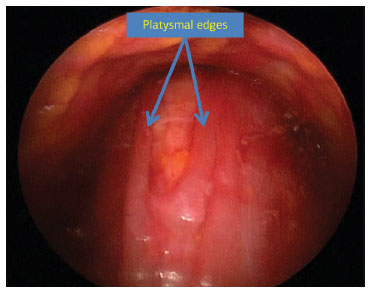
Figure 4. Videoendoscopic aspect of platysmal edges before the closure.
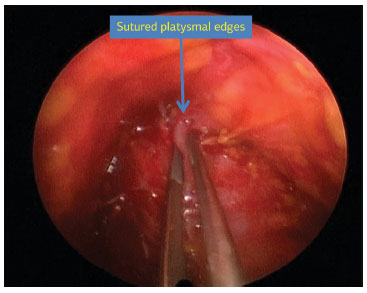
Figure 5. Platysma aspect once the suture is finalized.
After treatment of the deep structures, skin traction and resection were carried out. Once the reference points of the upper auricular and occipital region anchored the skin flap, the excess skin was removed with minimal tension6,8. The deep anchoring of the cutaneous flap to the auriculo-platysma ligament, carried out in the lobe with 4-0 monocryl thread (polyglecaprone) (Ethicon, reference Y426, São José dos Campos-SP, Brazil), prevented its distortion6,10. In the anterior region, the traction was performed obliquely and upward, while, in the posterior region, it followed the direction of the jawline8,11. Neither drains nor bandages were used routinely. The skin was sutured with 5-0 colorless mononylon thread, and 4-0 colorless mononylon thread in the posterior region (Ethicon, mononylon ethilon, São José dos Campos-SP, Brazil).
Meticulous hemostasis is carried out using the so-called second-look, as proposed by Baker & Gordon12. Approximately 30 minutes before the conclusion of the surgical procedure, a vial of 1 mL clonidine (150 µg/mL) was intravenously administered to promote hemodynamic stabilization and to reduce the plasma levels of catecholamines12.
Once the surgical procedure was completed, patients were transferred to the anesthetic recovery room, where they remained under continuous blood pressure monitoring. After approximately 12 hours, once evaluated by the surgeon and anesthesiologist, the patients were discharged. Eventually, they may stay hospitalized for a period of 24 hours.
Special material
For the correct execution of the technique proposed herein, some specific materials are necessary. The following materials will be used in videoassisted surgeries of the superior and middle plane of the face: endoscope of 30º, 18 cm in length and 3 mm in width (Figure 6); Ramirez® retractor (Karl Storz) with grip (Figure 6), presenting the advantage of maintaining the optical cavity, and allowing advancement and retraction of the camera. Gilles hooks or outer sutures may be used for additional traction and skin lifting, thus obtaining a global view of the region. Using a videoendoscope, coagulation of the structures involved was carried out by bipolar cautery (Montserrat Surgery, São Paulo-SP, Brazil), which allowed suction from one of its blades (Figure 7), and prevents the materials suctioned from obscuring the camera. In cases in which the cervical dissection touches the dissected hemifaces, a long surgical aspirator is introduced from the pre-auricular incision, to assist with the removal of suctioned material without occluding the surgical field, as can occur when the suction is carried out from the submental incision. Suturing of the platysma is facilitated by the use of a small incision, and a shorter needle with a lower curvature. It is recommended that a needle with a mounted cutting tip, 3/8 in diameter and 12-15 mm in length.
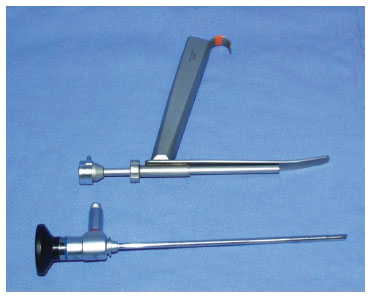
Figure 6. Endoscope and retractor.

Figure 7. Bipolar electrocautery coupled with a suction system.
RESULTS
The patients had an average age of 58.6 years (range, 51-68 years). With regards to sex, 15 patients were female, while only 1 was male. Regarding the ethnicity, 100% of the patients were Caucasians. Among the comorbidities present, hypertension controlled by medication was present in 11 cases (68.75%).
With regard to aesthetic improvement (Figures 8 to 13), Table 2 shows the scores obtained for each parameter according to the analysis of the evaluators. The group average was 8.29, i.e. the optimal score according to the grading system of Labbé et al.5. These results included 10 patients (62.5%) with an optimal score and 5 (31.25%) with a good score. Only 1 patient (6.25%) received a score below 6 points, and 1 patient (6.25%) obtained the maximum score. The patient that received a lower score presented with exacerbated cervical changes due to the occurrence of lipomatosis on the left side; this was subsequently fully removed with the aid of a videoendoscope.

Figure 8. Case 14: (A) preoperative frontal view. (B) frontal view 6 months after surgery.

Figure 9. Case 14: (A) preoperative right profile. (B) right profile 6 months after surgery.

Figure 10. Case 14: (A) preoperative left profile. (B) left profile 6 months after surgery.

Figure 11. Case 16: (A) preoperative frontal view. (B) frontal view 6 months after surgery.

Figure 12. Case 16: (A) preoperative right profile. (B) right profile 6 months after surgery.
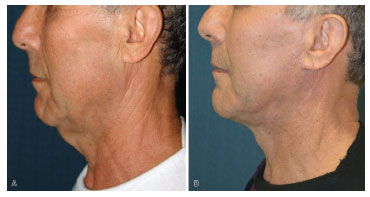
Figure 13. Case 16: (A) preoperative left profile. (B) left profile 6 months after surgery.
No patient presented with recurrent platysmal bands at 6 months after surgery.
Ideally, the scores of the evaluators would have been similar, which would have resulted in a lower range of scores (Figure 14). However, a large variation in scores can be observed in several cases, and is accepted when assessing cosmetic surgery outcomes11,13.
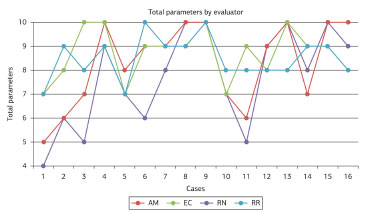
Figure 14. Total scores for each case by evaluator. The red line represents the scores assigned by the evaluator AM (Anna Martins), the green line by the evaluator EC (Eduardo C. Chem), the purple line by the evaluator RN (Rafael Netto), and the blue line by the evaluator RR (Ronaldo Righesso).
Among patients aged 50-65 years, results did not vary significantly. However, when comparing the average scores of younger and elder patients, it is notable that better outcomes were obtained in younger individuals (Figure 15).
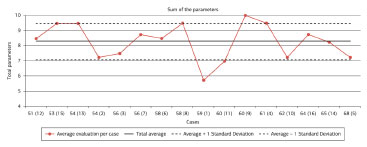
Figure 15. Total scores for each case, with cases distributed in ascending order of age. The X-axis gives the age of each case with the case number in parentheses.
A few mild complications were observed. One patient presented with redness of the scar, which lasted for approximately 3 months. There were no cases of collection in the postoperative period that required surgical drainage or aspiration with a syringe. One patient presented with extended facial edema lasting 20 days. The most frequent complaint was the feeling of cervical stretching, especially when the head was rotated laterally, and neck was hyperextended. In 4 patients (25%), these symptoms were present for approximately 15 days and resolved spontaneously. In 3 patients, palpation revealed hardening in the central region, which persisted for approximately 30 days, and coincided with the platysma suture line. Although palpable, it was not visible and it resolved spontaneously.
DISCUSSION
After a long period in which controversy in facial surgery focused on approaches to SMAS, nowadays, the aim is to achieve a better neck contour5,7-15. Millard was a pioneer of the submental scar, carrying out submental and submandibular lipectomy16. Guerrero-Santos and Connell recommended central plication of the platysma, combined with its lateral traction14,16. Only in the early 1990s, based on the principles of Feldman1,2, did the central platysmaplasty finally demonstrate the effect of previous plication on the cervical contour, and dictate the basis for its broader application.
With the widespread use of the central line, various issues emerged. The studies by Labbé et al.5 and Mustoe et al.17, among others16, highlighted several disadvantages, e.g. visible submental scar, longer surgical time, higher rates of complications (hematoma, seroma and infection), greater recovery time, combined with cervical hardening and potential cervical irregularities, among others.
Among the limiting factors, the most feared is the increased occurrence of hematomas10,14-18. Studies indicate that rates of hematoma development are between 3% and 8%12,18 in conventional rhytidoplasties. This increase, up to approximately 14% from that occurring with submental access, represents the factor mostly associated with hematoma18. It is evident that additional care should be taken while performing this procedure through submental access, as it requires greater tissue detachment15,16,18. We agree with the idea that hematomas should be evaluated in the light of the extension of the tissue to be detached18, as this is an extremely variable parameter. In cases classed as grade IV, according to McKinney3, in which greater tissue sagging can be observed with usual comorbidities of advanced age, including hypertension in particular, small detachments are considered preferable. However, these might result in aesthetic outcomes that are not always satisfactory10-16,18.
The possibility of approaching subplatysmal structures, in addition to the medial traction of platysma edges, are the differences resulting from performing the procedure through cervical midline access. From an anatomical point of view, the facial stratigraphy has a unique feature. Unlike other regions of the body, mesenchymal migration distributed the subcutaneous fat in 2 layers19. Therefore, the SMAS-platysma complex, originating from the mesenchyme, divides these into a superficial and deep portion19. Another difference is that in the upper and middle third of the face, volumetric soft tissue loss may occur due to the aging process. However, in the lower third, the opposite has been found, i.e. progressive fat accumulation8,16. Due to these peculiarities, a differentiated approach is necessary for the treatment of the fat that is deeply located in the platysma1,2,8-14,18.
Another relevant factor is the possibility for correction of the redundant platysma medial edges. The lateral traction of SMAS-platysma will not always result in the resolution of medial sagging, especially in cases with more excess10,16. According to the principle of non-linear elastic deformation20, the more distant from the point in which the force is exerted, the lower will be the traction transmitted. The platysmaplasty proposed by Feldman1,2,10 directly acts on the central region. It should be noted that this procedure not only approximates these redundant edges, but allows the medial advancement with their overlapping to fill the space released from the resection of subplatysmal fat13.
By increasing the indications of videoendoscope-assisted procedures, in cases of minor sagging (McKinney3 II and III), in which the central approach of the platysma is not clear, the use of an endoscope can define whether an additional central treatment is required. Therefore, the videoendoscope is introduced through a submental incision of 1 cm to evaluate the final appearance, resulting from lateral traction on medial bands. In several cases, it is observed that, even after the lateral traction of SMAS-platysma complex, an important sagging persists in the midline and requires further corrections13,16.
According to the technique of Feldman1, the submental scar length is reduced by approximately 50% (Figure 16), although other authors report scars lengths of up to 6 cm6,11,17. Therefore, this is only one of the advantages to the use of videoendoscope-assisted procedures. Feldman1 himself stated: "It is important that the incision would be long enough to allow the visualization of all the detached portions of the anterior cervical region. A very small incision will hinder the generation of the corset". Even with a smaller scar, the use of a videoendoscope allows proper visualization of the structures involved and amplifies this image. The meticulous removal of the excess fat, the careful hemostasis and suturing of the platysmal edges facilitated the implementation of the procedure. Another advantage is the potential for this procedure to be visualized by other members of the team, thus enabling trainees to observe a correct step-by-step demonstration of the surgery.

Figure 16. Submental scar aspect, 6 months after surgery, measuring less than 2 cm in length. The white line emphasizes the scar and its limits.
Among the disadvantages of using a videoendoscope for platysmaplasty procedures, we point out the high cost of the equipment and increased surgical time. In surgeries in which videoendoscope-assisted procedures are carried out in the frontal region, these devices are already available and the increase mentioned above refers only to the surgical time. Once this technique is fully mastered, its gradual employment will allow the procedure to be performed within a surgical time that is similar to conventional techniques; in our cases, this varies between 30 and 65 minutes.
Despite the small cohort, the satisfactory outcomes that were observed suggest that the assistance provided by using a videoendoscope to carry out platysmaplasty procedures can be of great value, in terms of improving the results and reducing the complication rates. However, usual care, e.g. the continuous monitoring of post-operative tension values should be maintained. Further studies are required to determine the validity of this technique, and are about to be implemented. We believe that the technique proposed is another alternative to achieve appropriate surgical outcomes in this highly complex group of patients, that have long been considered to have what has been described as a "difficult neck"3,7.
REFERENCES
1. Feldman JJ. Corset platysmaplasty. Plast Reconstr Surg. 1990;85(3):333-43. http://dx.doi.org/10.1097/00006534-199003000-00001. PMid:2304983
2. Feldman JJ. Neck lift. St. Louis: Quality Medical Publishing; 2006.
3. McKinney P. The management of platysma bands. Plast Reconstr Surg. 1996;98(6):999-1006. http://dx.doi.org/10.1097/00006534-199611000-00011. PMid:8911469
4. Ellenbogen R, Karlin JV. Visual criteria for success in restoring the youthful neck. Plast Reconstr Surg. 1980;66(6):826-37. http://dx.doi.org/10.1097/00006534-198012000-00003. PMid:7443846
5. Labbé D, Franco RG, Nicolas J. Platysma suspension and platysmaplasty during neck lift: anatomical study and analysis of 30 cases. Plast Reconstr Surg. 2006;117(6):2001-7, discussion 2008-10. http://dx.doi.org/10.1097/01.prs.0000218972.75144.9c. PMid:16651976
6. Marten TJ. Facelift. Planning and technique. Clin Plast Surg. 1997;24(2):269-308. PMid:9142469.
7. Benito J, Righesso R. Tratamento cirúrgico da região cervical associado a suturas de suspensão platismal com fios de politetrafluoroetileno. Rev Bras Cir Plást. 2007;22(4):202-8.
8. Warren RJ, Aston SJ, Mendelson BC. Face lift. Plast Reconstr Surg. 2011;128(6):747e-64e. http://dx.doi.org/10.1097/PRS.0b013e318230c939. PMid:22094776
9. Narasimhan K, Stuzin JM, Rohrich RJ. Five-step neck lift: integrating anatomy with clinical practice to optimize results. Plast Reconstr Surg. 2013;132(2):339-50. http://dx.doi.org/10.1097/PRS.0b013e3182958b6f. PMid:23897334
10. Labbé D, Franco RG, Nicolas J. Platysma suspension and platysmaplasty during neck lift: anatomical study and analysis of 30 cases. Plast Reconstr Surg. 2006;117(6):2001-7, discussion 2008-10. http://dx.doi.org/10.1097/01.prs.0000218972.75144.9c. PMid:16651976
11. Nunes D, Ilgenfritz J JR, Viana GP, Viana GAP, Almeida KG, Cury M, et al. Cervicoplastia ampliada para correção de alterações cervicais. Rev Bras Cir Plást. 2011;26(1):58-65. http://dx.doi.org/10.1590/S1983-51752011000100013.
12. Baker DC, Stefani WA, Chiu ES. Reducing the incidence of hematoma requiring surgical evacuation following male rhytidectomy: a 30-year review of 985 cases. Plast Reconstr Surg. 2005;116(7):1973-85, discussion 1986-7. http://dx.doi.org/10.1097/01.prs.0000191182.70617.e9. PMid:16327611
13. Castro CC, Aboudib JH JR, Roxo ACW. Updating the concepts on neck lift and lower third of the face. Plast Reconstr Surg. 2012;130(1):199-205. http://dx.doi.org/10.1097/PRS.0b013e318254b39c. PMid:22743883
14. Cardoso de Castro C. The changing role of platysma in face lifting. Plast Reconstr Surg. 2000;105(2):764-75, discussion 776-7. http://dx.doi.org/10.1097/00006534-200002000-00047. PMid:10697191
15. Citarella ER, Sterodimas A, Condé-Green A. Endoscopically assisted limited-incision rhytidectomy: a 10-year prospective study. J Plast Reconstr Aesthet Surg. 2010;63(11):1842-8. http://dx.doi.org/10.1016/j.bjps.2009.11.021. PMid:19962950
16. Stuzin JM. Discussion. Modified deep plane rhytidectomy with a lateral approach to the neck: an alternative to submental incision and dissection. Plast Reconstr Surg. 2011;127(1):371-3. http://dx.doi.org/10.1097/PRS.0b013e3181f957da. PMid:21200232
17. Mustoe TA, Rawlani V, Zimmerman H. Modified deep plane rhytidectomy with a lateral approach to the neck: an alternative to submental incision and dissection. Plast Reconstr Surg. 2011;127(1):357-70. http://dx.doi.org/10.1097/PRS.0b013e3181f95d66. PMid:21200231
18. Auersvald A, Auersvald LA, Lourdes M, Biondo-Simões P. Rede hemostática: uma alternativa para a prevenção de hematoma em ritidoplastia. Rev Bras Cir Plást. 2012;27(1):22-30. http://dx.doi.org/10.1590/S1983-51752012000100006.
19. Chem RC, Costa LAL, Netto R, Pavelecini M. Anatomia cirúrgica da face. In: Casagrande C, editor. Plástica de face videoendoscópica. Rio de Janeiro: Di Livros; 2010. p. 55-70.
20. Finger ER. A 5-year study of the transmalar subperiosteal midface lift with minimal skin and superficial musculoaponeurotic system dissection: a durable, natural-appearing lift with less surgery and recovery time. Plast Reconstr Surg. 2001;107(5):1273-83, discussion 1284. http://dx.doi.org/10.1097/00006534-200104150-00028. PMid:11373573
1. Titular member of the Brazilian Society of Plastic Surgery (BSPS), Bento Gonçalves, RS, Brazil
2. Master in Medicine, Titular Member of the Brazilian Society of Plastic Surgery (BSPS), Porto Alegre, RS, Brazil
3. Resident physician at the Plastic Surgery Service of the Santa Casa de Misericórdia of Porto Alegre, Training aspirant of the Brazilian Society of Plastic Surgery (BSPS), Porto Alegre, RS, Brazil
4. Resident physician at the Dr. Farid Hakme Surgery Service, Hospital da Plástica-UNIG/RJ, Training aspirant of the Brazilian Society of Plastic Surgery (BSPS), Rio de Janeiro, RJ, Brazil
Institution: Study performed at the Plastic Surgery Center Dr. Ronaldo Righesso - Hospital Tacchini, Bento Gonçalves, RS, Brazil.
Corresponding author:
Ronaldo Righesso
Center of Plastic Surgery Dr. Ronaldo Righesso
Rua General Osório, 329, ground floor, room 1
Bento Gonçalves, RS, Brazil CEP 95700-000
Phone: (54) 3451-8882
E-mail: righesso@yahoo.es
Article received: May 12, 2014.
Article accepted: August 03, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter