

Original Article - Year 2014 - Volume 29 -
Lower trapezius myocutaneous pedicle flap in head, neck, and chest reconstructions after cancer surgeries
Retalho miocutâneo inferior pediculado do músculo trapézio nas reconstruções após cirurgias oncológicas de cabeça e pescoço, e tórax
ABSTRACT
INTRODUCTION: In this article, we present a literature review on the lower myocutaneous trapezius flap, and report its advantages, surgical technique, and complications.
METHODS: We studied 19 patients treated at INCA with a specific technique, and compared the outcomes with those reported in the international literature.
RESULTS: All reconstructions achieved the procedural objectives, and the defects of soft tissues and skin were repaired. The aesthetic outcome was considered satisfactory by the patients and medical staff. The rate of complications was 21%. No necrosis or signs of infection were detected in the flaps. Concerning the functions, 89.5% of patients preserved their motor function, whereas reduced functional movements were observed in 10.5% of the patients due to tumor invasion to the accessory nerve.
CONCLUSIONS: Despite the continuous advancements in microsurgical techniques, pedicle myocutaneous flaps are still indicated for reconstruction procedures after extended cancer resections. The use of the lower trapezius myocutaneous flap is safe and represents a suitable option for the reconstruction of soft tissues of the lateral and posterior cervical regions, side of the head, shoulder, and upper paravertebral and parascapular regions.
Keywords: Lower trapezius flap; myocutaneous flap; head and neck reconstruction; chest reconstruction.
RESUMO
INTRODUÇÃO: Revisão da literatura sobre o retalho miocutâneo inferior do músculo trapézio, apresentando suas vantagens, técnica cirúrgica e complicações.
MÉTODOS: Estudo de 19 casos tratados no INCA, através de técnica específica, e comparação dos dados com a literatura internacional.
RESULTADOS: Todas as reconstruções atingiram seus objetivos, com correção dos defeitos em partes moles e pele. O efeito estético foi considerado bom pelos pacientes e pela equipe médica. Foi observada uma taxa de 21% de complicações. Não houve necrose ou infecção nos retalhos. Em relação às funções, 89,5% apresentaram função motora preservada e 10,5%, déficit funcional por acometimento tumoral do nervo acessório.
CONCLUSÃO: A despeito do aprimoramento contínuo das técnicas microcirúrgicas, os retalhos miocutâneos pediculados ainda encontram indicações nas reconstruções após ressecções oncológicas alargadas. O retalho miocutâneo inferior do músculo trapézio é uma alternativa segura e aplicável para as reconstruções de partes moles das regiões cervicais lateral e posterior, da região lateral da cabeça, da região do ombro e para as regiões paraespinhal superior e paraescapulares.
Palavras-chave: Retalho inferior trapézio; Retalho miocutâneo; Reconstrução cabeça e pescoço; Reconstrução tórax.
For the reconstruction of large defects after the resection of head and neck cancers, microsurgery techniques are the preferred option, in particular because of their versatility in three-dimensional reconstructions. In the thoracic region, the availability of different pedicle flaps means that microvascularized flaps should only be used for the reconstruction of large and combined defects. Although microsurgical flaps have advantages, their indication is not appropriate in particular situations. Prohibitive medical condition, reserved prognosis, hygienic resections, and difficulty of obtaining recipient vessels are some of the reasons justifying the use of pedicled flaps. The use of pedicled flaps reduces the surgical time, simplifies the reconstructive procedures, and could be carried out at centers for reconstructive plastic surgery that do not have microsurgical expertise. The use of pectoralis major muscle flaps for head and neck surgery and of latissimus dorsi flaps for thoracic surgery are of great importance and still used with high frequency. In these specific situations, the use of the lower trapezius myocutaneous flap is still limited. However, this is a simple alternative that presents a low morbidity and provides satisfactory results, with minimal functional loss, thus constituting a suitable option for the reconstructions of the upper chest and distal third of head and neck. In this article, we describe our experience with 19 consecutive patients that were operated on at the Reconstructive Plastic Surgery and Microsurgery Service of INCA (Rio de Janeiro, Brazil), between 2004 and 2009, by using the lower trapezius myocutaneous pedicle flap. In addition, we highlight the features, advantages, and complications of this treatment method.
PATIENTS AND METHODS
We conducted a retrospective study of medical records of patients who underwent surgical treatment, between 2004 and 2009, for the resection of advanced chest, head, and neck tumors. The subsequent reconstruction was performed by the plastic surgery team of INCA, by using the lower trapezius myocutaneous pedicle flap. We recorded the patients' demographic data, stage, location and histopathological diagnosis of the tumor, size of the surgical specimen (obtained from the pathological records), and complications related to the procedure. The patients were followed from the date of the scheduled surgery and monitored from 15 days to 31 months, during the outpatient treatment, for an average period of approximately 15 months. All patients were evaluated postoperatively in relation to the abduction capacity and elevation of the ipsilateral upper limb above the shoulder line.
Surgical technique
The trapezius muscle is divided into three parts: upper, middle, and lower. Its vascularization derives from the transverse cervical, occipital, dorsal scapular, and perforating vessels from the posterior intercostal vessels. Owing to this pattern, several authors classify this vascularization as presenting the V pattern of Mathes and Nahai. Its motor innervation derives from the spinal nerve. Besides having other secondary functions, the trapezius muscle participates in the elevation, retraction, and rotation of the scapula, in addition to allowing the elevation of the shoulder during the abduction and flexion of the arm. Its denervation results in a drop of the shoulder1-6.
Demarcation of the skin island is carried out by taking as references the middle line and tip of the scapula. This should be planned in such a way that at least one-third of this area is located above the tip of the scapula, thus providing sufficient contact between the skin island and the muscle, while ensuring the preservation of the minimum number of perforating myocutaneous vessels and sufficient vascular supply to the skin. Once the skin island is planned and the medial edge is incised, muscle dissection can begin. The positioning of the skin island could be changed according to the overlap between this structure and the muscle. Therefore, if juxtaposed, the marking should be maintained and in the presence of discrepancies, the skin island would then need to be re-marked, more caudal or cranial, depending on the position of the muscle. A craniocaudal dissection is performed with the transection of spine inserts and their lateral border, having as cranial limit the spine of the scapula. Thus, the dorsal scapular artery is identified, being located between the rhomboid major and minor muscles, which elevate the flap up to its pivot point, juxtaposing to the rhomboid minor muscle, which could be sectioned to improve flap rotation. The maintenance of a double vascularization provided by both the superficial cervical and dorsal scapular arteries ensures the safety of the procedure, which presents a lower rate of partial losses and flap necrosis. The communication between donor and recipient areas can be achieved by tunneling the cranial skin to the flap, or with incision and detachment. Muscle dissection should not exceed >10 cm from the spine of the scapula, which represents the emergency point of the scapula, an option corroborated by other authors7-9. This limit for the muscle section is also essential to preserve the function of muscle horizontal fibers, which are responsible for the abduction of the upper limb and its elevation above the shoulder line. The implementation of the lower flap through this technique and the plan described above allows producing a flap with a skin island, the length of which varies according to the capacity of the flaccid skin of the patient to allow the primary suture of the donor area, since usually the arc of rotation enables to reach the lower temporal, occipital, parotid, and auricular regions, in addition to the lateral and posterior cervical regions. In the thoracic region, the arc of rotation involves the shoulder, scapular and parascapular, and ipsilateral and contralateral regions. Therefore, we were able to obtain a flap that was safe from a circulatory point of view and presented minimal functional morbidity1,9,10-18.
RESULTS
Nineteen reconstructions were performed by using a lower trapezius myocutaneous pedicle flap. These were carried out at the Reconstructive Plastic Surgery and Microsurgery Service of INCA, in 12 female and 7 male patients. At the time of surgery, all patients presented an advanced tumor stage and were classified as T4 (TNM)19. The average age of the patients was 66.1 years and varied between 44 and 82 years.
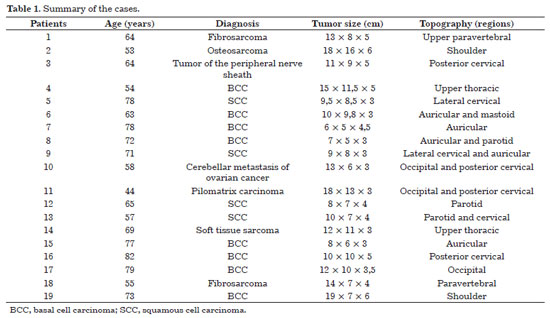
After the resection of malignant neoplasms, all patients were treated with immediate reconstruction. The resected tumors were as follows: basal cell carcinoma in 8 cases, squamous cell carcinoma in 4 cases, and fibrosarcoma in 2 cases. One case each of the following histological types was also found: osteosarcoma, peripheral nerve sheath tumor, cerebellar ovarian carcinoma metastasis, pilomatrix carcinoma, and soft tissue sarcoma. The dimensions of the tumors varied between 7 × 5 × 3 cm3 and 18 × 16 × 6 cm3. These measures probably underestimated the actual size of the defect, owing to the primary contraction of the tumor after its resection. All flaps that were used have smaller dimensions. The 19 cases are summarized in Table 1.
All reconstructions achieved the proposed objectives in the surgical plan, and the defects due to soft tissue reduction and skin coverage were repaired. The aesthetic outcome in the recipient area was considered satisfactory by the patients and medical staff.
Complications were observed in 21% of the patients. No necrosis of the flaps or infections were observed in the receiving area. One patient presented a delay in the integration of the flap, and a new surgical procedure for the revitalization of the contact surface between the recipient bed and the flap was required. Two patients presented small dehiscences; however, these did not need a second surgical intervention. In all cases, a primary synthesis of the donor area was performed. Scar enlargement was observed on the back of four patients. One case of seroma was detected on the back of one patient, whereas no hematomas occurred after the removal of vacuum drains that were used in all patients in donor and receiving areas. The motor function of the ipsilateral upper limbs was preserved in 17 patients (89.5%). Two patients (10.5%) presented a reduced functionality of the ipsilateral upper limb, which was caused by the resection of the accessory nerve along with the tumor. Figures 1 to 5 show cases in which reconstruction with a lower trapezius flap was indicated, in addition to the surgical plan and outcomes during the immediate and late postoperative period.

Figure 1. Defect, reconstruction, immediate postoperative period, and 7 days after the resection of retroauricular basal cell carcinoma.

Figure 2. Defect, reconstruction, immediate postoperative period, and 3 months after the surgery with a lower trapezius flap for the reconstruction of the occipital region. Notice the relation between the skin island and the projection of the trapezius muscle fibers.

Figure 3. Repair of the largest defect in the occipital region carried out after resecting a pilomatrix carcinoma.

Figure 4. Photograph of the left shoulder resection, dissection and positioning of the flap to avoid disarticulation of the ipsilateral limb, and immediate aspect of the donor area. Late postoperative period of 6 months, showing the occurrence of an unsightly scar, with a satisfactory defect coverage and no functional loss.

Figure 5. Appearance after the resection of a large squamous cell carcinoma on the right shoulder. Images of the immediate postoperative period, and at 7 days and 12 months after the reconstruction. Scar enlargement in the donor area can be observed, with no motor dysfunction.
DISCUSSION
The first description of a trapezius muscle flap was published by Conley in 1972, based on perforating veins of the paraspinal muscle derived from posterior intercostal vessels20. McCraw et al., in 1977, were pioneers in studying skin regions in flaps21. Lateral and lower flaps were originally described by Demergasso and Piazza in 1979 and by Baek et al. in 1980, respectively10,11. As composite flaps, these were commonly used in jaw reconstructions. However, the high rate of complications, need for intraoperative decubitus change, and development of better techniques prevent their use nowadays. The trapezius muscle flap, being either muscular, musculocutaneous, or osteomyocutaneous, was classified as type II by Mathes and Nahai1. As the main pedicle, it presents transverse cervical vessels; on the other hand, occipital, dorsal scapular, and posterior intercostal perforating vessels serve as secondary pedicles. When the reconstruction is planned only with the use of a muscle component, the middle and lower portions of the muscle, based on the descending branch of the transverse cervical artery, are used. This allows an arc of rotation based on the inferior-posterior region of the neck, and is able to reach the occipital, cervical, and superior-posterior thoracic regions as well as the middle third of the face. Three variants of myocutaneous flaps can be used: the lateral flap, upper flap, and lower trapezius myocutaneous flap. With this flap, is it possible to use vascularized bone tissues that include the spine and part of the body of the scapula for the reconstruction of complex defects, such as in cases of mandibular resection22.
The lower trapezius myocutaneous flap presents the following advantages: reconstruction with tissue that is distant from the resection area and a long vascular pedicle that provides an excellent arc of rotation. Moreover, it contains little subcutaneous tissue on its skin island, which presents few hairs and allows the primary synthesis of the donor area2-4,10,20,23-26. On the other hand, it has the disadvantage of causing the appearance of an unsightly scar in the donor area.
Mastering the angiosome concepts of the body allows modifying the skin islands plan, in order to increase the arc of rotation and ensure its viability, with a small contact area between the muscle and skin island27. Recent studies showed that the use of the lower trapezius flap extending beyond the scapular spine is a feasible procedure, based on the vascularization obtained from the scapular dorsal artery and choke vessels located among its branches and intercostal vessels. Therefore, it is possible to obtain musculocutaneous flaps with sizes up to 7 × 38 cm, without the involvement of the dermal plexus and overlying skin, which in most cases remain functional and preserve the abduction capacity23-26. However, larger series of patients would be required to obtain statistically significant results to support the feasibility of this procedure.
The results from new anatomical studies and clinical series9 have started to allow a safer indication of this procedure with less morbidity. A better knowledge on vascularization and the limitations of its recommendation in specific situations has allowed ensuring flap survival and significantly diminished failures7-9,12,17,18.
In our experience, the dissection of the lower trapezius myocutaneous pedicle flap based on two vascular pedicles, i.e., the superficial cervical and dorsal scapular vessels, allowed achieving a great vascularization of the flap, avoiding partial loss or necrosis, without presenting any difficulty with their rotation toward the cervical and thoracic regions. In addition, no associated functional losses were observed, contrarily to what was suggested by Haas et al.9. There is a lack of data in the literature on the morbidity of double-vascularized flaps, whereas this study demonstrates a concrete technique with safe results. However, further investigations on this technique are still required to corroborate our findings.
CONCLUSION
Despite the continuous improvement of microsurgical techniques, myocutaneous pedicle flaps are still indicated for reconstruction procedures after extended cancer resections. The use of the lower trapezius myocutaneous flap is safe and represents a suitable option for the reconstruction of soft tissues of the lateral and posterior cervical regions, side of the head, shoulder, and upper paravertebral and parascapular regions.
REFERENCES
1. Mathes SJ, Nahai F. Trapezius flap. In: Mathes SJ, Nahai F, editors. Reconstructive surgery: principles, anatomy and technique. New York: Churchill Livingstone; 1997. p. 651-77.
2. Nishio S, Cordeiro AC, Brandão LG, de Britto e Silva Filho G, Dos Santos LR, Cernea CR, et al. Posterior trapezius myocutaneous flap. Rev Paul Med. 1993;111(2):367-74. PMid:8284581.
3. Siberchicot F, Barthelemy I, Phan E, Michelet V, Pinsolle J. [Lateral trapezius flap in cervico-facial surgery. Apropos of 89 cases]. Ann Chir Plast Esthet. 1995;40(2):130-5. PMid:7574390.
4. Aviv JE, Urken ML, Lawson W, Biller HF. The superior trapezius myocutaneous flap in head and neck reconstruction. Arch Otolaryngol Head Neck Surg. 1992;118(7):702-6. http://dx.doi.org/10.1001/archotol.1992.01880070032006. PMid:1627289
5. Yang D, Morris SF. Trapezius muscle: anatomic basis for flap design. Ann Plast Surg. 1998;41(1):52-7. http://dx.doi.org/10.1097/00000637-199807000-00010. PMid:9678469
6. Horch RE, Stark GB. The contralateral bilobed trapezius myocutaneous flap for closure of large defects of the dorsal neck permitting primary donor site closure. Head Neck. 2000;22(5):513-9. http://dx.doi.org/10.1002/1097-0347(200008)22:5<513::AIDHED12> 3.0.CO;2-N. PMid:10897113
7. Tan KC, Tan BK. Extended lower trapezius island myocutaneous flap: a fasciomyocutaneous flap based on the dorsal scapular artery. Plast Reconstr Surg. 2000;105(5):1758-63. http://dx.doi.org/10.1097/00006534-200004050-00025. PMid:10809110
8. Netterville JL, Wood DE. The lower trapezius flap. Vascular anatomy and surgical technique. Arch Otolaryngol Head Neck Surg. 1991;117(1):73-6. http://dx.doi.org/10.1001/archotol.1991.01870130079020. PMid:1986765
9. Haas F, Weiglein A, Schwarzl F, Scharnagl E. The lower trapezius musculocutaneous flap from pedicled to free flap: anatomical basis and clinical applications based on the dorsal scapular artery. Plast Reconstr Surg. 2004;113(6):1580-90. http://dx.doi.org/10.1097/01.PRS.0000117188.03152.10. PMid:15114117
10. Demergasso F, Piazza MV. Trapezius myocutaneous flap in reconstructive surgery for head and neck cancer: an original technique. Am J Surg. 1979;138(4):533-6. http://dx.doi.org/10.1016/0002-9610(79)90414-8. PMid:384820
11. Baek SM, Biller HF, Krespi YP, Lawson W. The lower trapezius island myocutaneous flap. Ann Plast Surg. 1980;5(2):108-14. http://dx.doi.org/10.1097/00000637-198008000-00004. PMid:7447278
12. Haas F, Pierer G, Weiglein A, Moshammer H, Schwarzl F, Scharnagl E. [The lower trapezius muscle island flap. Anatomic principles and clinical relevance]. Handchir Mikrochir Plast Chir. 1999;31(1):15-20. http://dx.doi.org/10.1055/s-1999-13900. PMid:10080056
13. Rosen HM. The extended trapezius musculocutaneous flap for cranio-orbital facial reconstruction. Plast Reconstr Surg. 1985;75(3):318-27. http://dx.doi.org/10.1097/00006534-198503000-00003. PMid:3856286
14. Chandrasekhar B, Terz JJ, Kokal WA, Beatty JD, Gottlieb ME. The inferior trapezius musculocutaneous flap in head and neck reconstruction. Ann Plast Surg. 1988;21(3):201-9. http://dx.doi.org/10.1097/00000637-198809000-00003. PMid:3223698
15. Linss W, Fuhrmann P, Knappe K, Schumann D. [Anatomic studies of the availability of the transverse cervical artery as the stem vessel of pedicled myocutaneous flaps in plastic surgery]. Anat Anz. 1990;170(3-4):227-36. PMid:2375502.
16. Lynch JR, Hansen JE, Chaffoo R, Seyfer AE. The lower trapezius musculocutaneous flap revisited: versatile coverage for complicated wounds to the posterior cervical and occipital regions based on the deep branch of the transverse cervical artery. Plast Reconstr Surg. 2002;109(2):444-50. http://dx.doi.org/10.1097/00006534-200202000-00005. PMid:11818818
17. Weiglein AH, Haas F, Pierer G. Anatomic basis of the lower trapezius musculocutaneous flap. Surg Radiol Anat. 1996;18(4):257-61. http://dx.doi.org/10.1007/BF01627601. PMid:8983103
18. Haas F, Pierer G, Weiglein A, Moshammer H, Schwarzl F, Scharnagl E. Der untere M. trapezius-Insellappen. Anatomische Grundlagen und klinische Relevanz. Handchir Mikrochir Plast Chir. 1999;31(1):15-20. http://dx.doi.org/10.1055/s-1999-13900. PMid:10080056
19. Sobin LH, Hermanek P, eds. TNM classification of malignant tumours. 4th ed. New York: Springer Berlin-Heidelberg; 1992.
20. Conley J. Use of composite flaps containing bone for major repairs in the head and neck. Plast Reconstr Surg. 1972;49(5):522-6. http://dx.doi.org/10.1097/00006534-197205000-00008. PMid:4554701
21. McCraw JB, Dibbell DG, Carraway JH. Clinical definition of independent myocutaneous vascular territories. Plast Reconstr Surg. 1977;60(3):341-52. PMid:142995.
22. Panje WR. Mandible reconstruction with the trapezius osteomusculocutaneous flap. Arch Otolaryngol. 1985;111(4):223-9. http://dx.doi.org/10.1001/archotol.1985.00800060047005. PMid:3883977
23. Chen WL, Li J, Yang Z, Huang Z, Wang J, Zhang B. Extended vertical lower trapezius island myocutaneous flap in reconstruction of oral and maxillofacial defects after salvage surgery for recurrent oral carcinoma. J Oral Maxillofac Surg. 2007;65(2):205-11. http://dx.doi.org/10.1016/j.joms.2005.10.056. PMid:17236922
24. Chen WL, Zhang B, Wang JG, Yang ZH, Huang ZQ, Zhang DM. Reconstruction of large defects of the neck using an extended vertical lower trapezius island myocutaneous flap following salvage surgery for neck recurrence of oral carcinoma. J Plast Reconstr Aesthet Surg. 2011;64(3):319-22. http://dx.doi.org/10.1016/j.bjps.2010.05.012. PMid:20541988
25. Uğurlu K, Ozçelik D, Hüthüt I, Yildiz K, Kilinç L, Baş L. Extended vertical trapezius myocutaneous flap in head and neck reconstruction as a salvage procedure. Plast Reconstr Surg. 2004;114(2):339-50. http://dx.doi.org/10.1097/01.PRS.0000131984.55825.9D. PMid:15277797
26. Rasheed MZ, Tan BK, Tan KC. The extended lower trapezius flap for the reconstruction of shoulder tip defects. Ann Plast Surg. 2009;63(2):184-7. http://dx.doi.org/10.1097/SAP.0b013e318189a9a7. PMid:19574889
27. Taylor GI, Palmer JH. The vascular territories (angiosomes) of the body: experimental study and clinical applications. Br J Plast Surg. 1987;40(2):113-41. http://dx.doi.org/10.1016/0007-1226(87)90185-8. PMid:3567445
1. Certified Plastic Surgeon by the Brazilian Society of Plastic Surgery (BSPS), Master's Degree from the State University of Campinas (UNICAMP), Staff Member at the Plastic Surgery and Microsurgery Service of the National Cancer Institute, Rio de Janeiro, RJ, Brazil
2. Specialist in Plastic Surgery by the Brazilian Society of Plastic Surgery (BSPS), Resident in Plastic Surgery with Microsurgery Specialization at the National Cancer Institute, Rio de Janeiro, RJ, Brazil
Institution: Study performed at the National Cancer Institute, Rio de Janeiro, RJ, Brazil.
Correponding author:
Juliano Carlos Sbalchiero
Plastic Surgery and Microsurgery Service of INCA
Praça da Cruz Vermelha, 23
Rio de Janeiro, RJ, Brazil ZIP 20230-130
Phone: (21) 3207-1085; Fax: (21) 3207-1085
E-mail: jsbalchiero@terra.com.br
Article received: October 29, 2012.
Article accepted: January 28, 2013.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter